Does Medicare Cover Online Counseling
Medicare didnt used to cover online therapy, but it does now. In 2020, Medicare removed many long-standing restrictions on its coverage of telemedicine.
In the past, Medicare only covered telehealth services provided in rural locations and other federally designated Professional Shortage Areas. It also covered telehealth services only when they were provided in a medical facility like a hospital or clinic. This ruled out in-home telehealth services like online counseling.
Thanks to the changes made to Medicare policy in 2020, Medicare no longer limits telehealth coverage to people in rural areas and now covers telehealth services provided in a persons home.
For more information, you can go to Medicares telehealth coverage information page.
Does Medicare Pay For Therapy Services
As part of Medicares mental health care benefits, therapy, or counseling is typically covered under Part B as an outpatient service with Original Medicare. MA plans provide the same benefits as Part B does. Therapy generally can be for an individual or a group. Family therapy is covered if it is to support the Medicare beneficiarys mental health treatment goals.
As with all mental health services, you must receive therapy from a provider that accepts assignment for Original Medicare or is in-network with your MA plan. The provider must be licensed in your state. Copay or coinsurance and deductibles apply.
In 2022, for instance, for outpatient mental health care through a UnitedHealthcare MA HMO plan, you pay $25 copay for each Medicare-covered individual therapy session and $15 copay for group therapy. For a similar type of plan with Humana, you pay a $20 copay for mental health services received from a specialist, an outpatient hospital, or intensive therapy that is part of the day program in a hospital. For a similar plan with BCBS/Anthem, you pay $40 for each Medicare-covered visit, group, or individual.
Your copays vary depending on your MA plan. To find out what your out-of-pocket costs will be and precisely what your plan will cover based on Medicare rules, talk with your plans administrator, review your EOC, and talk with your healthcare provider. Allow for the time it takes to get a referral and prior authorization.
Medicaid Mental Health Reimbursement Rates For Individual Therapy
Below is a table showing the rates that have been determined by Medicaid for these differing license levels for commercial insurance polices:
| 45-50 minutes | |
| Practitioner Level 5 | $75.64 |
Now you must be wondering: What??!! Medicaid doesnt pay that much!!! And youre right.
These are the rates that they established as averages nationally based on a huge survey of insurance policies by their relative license. These are the commercial insurance reimbursement rates for psychotherapy determined by Medicaid.
Medicaid mental health reimbursement rates differ in that medicaid reduces these rates to providers at Practitioner Levels 2-5, which cover all licensed mental health providers except MDs.
So, take the above charts and then reduce their numbers and you can expect to get payment more like the following:
| 45-50 minute therapy session |
Again, these are the rates that have been determined as average payment rates by insurance based on research done by that States medicaid program, in this case Mississippi.
These rates get reduced but these are useful to look at to see what they believe are the average reimbursement rates by procedure code.
This information does not take into account the effect of the license or practitioner level on total reimbursement rate.
Read Also: Who Is My Medicare Carrier
Cpt Code : Complete Guide With Reimbursement Rates
CPT Code 90834 is the most common procedure code used in mental health and behavioral health billing.
Learn how to bill Cpt Code 90834 accurately every time with our insurance billing guide.
Youll discover the differences between procedure codes 90834 and 90837, the reimbursement rate for 90834, which add-on codes to use, and how to code your claims using procedure code 90834.
Article Index
If youd rather hand these sorts of tasks off to a team of billers who can help, consider reaching out to our mental health billing service.
Medigap Medsup And Mental Health Care
For starters, both Medigap and MedSup are terms for a product normally called Medicare supplement insurance.
As implied, this policy supplements the costs related to Original Medicare. To put it another way, it helps people pay for some of the expenses Medicare doesnt cover.
Learn more about this type of plan in our Medicare Supplement Insurance Policy FAQ.
Thats true whether youre talking about general health care or mental health care. For example, most Medigap plans cover the costs Medicare Parts A and B wont pay for if youre hospitalized for mental illness.
A few examples:
- All Medigap policies cover your Part A hospitalization copays and coinsurance
- They also cover all or part of your psychiatrists copays and coinsurance
- Most of these plans cover your Part A hospitalization deductible, too
MedSup and Medigap plans help if youre ever get outpatient treatment for mental illness as well. Specifically, they usually cover some or all of your Part B out-of-pocket costs.
Read Also: Does Medicare Part D Cover Shingrix Vaccine
Don’t Miss: What Is The Cost Of Medicare Part C For 2020
What Is Medicare Insurance
Medicare is a government-run national health insurance program that began in 1965 under the Social Security Administration. Today, the Centers for Medicare and Medicaid Services administer its four parts .
As of 2016, Tennessee has some of the highest percentages of citizens receiving disability benefits, thus receiving Medicare.3
Does Medicare Cover Inpatient Psychiatric Care
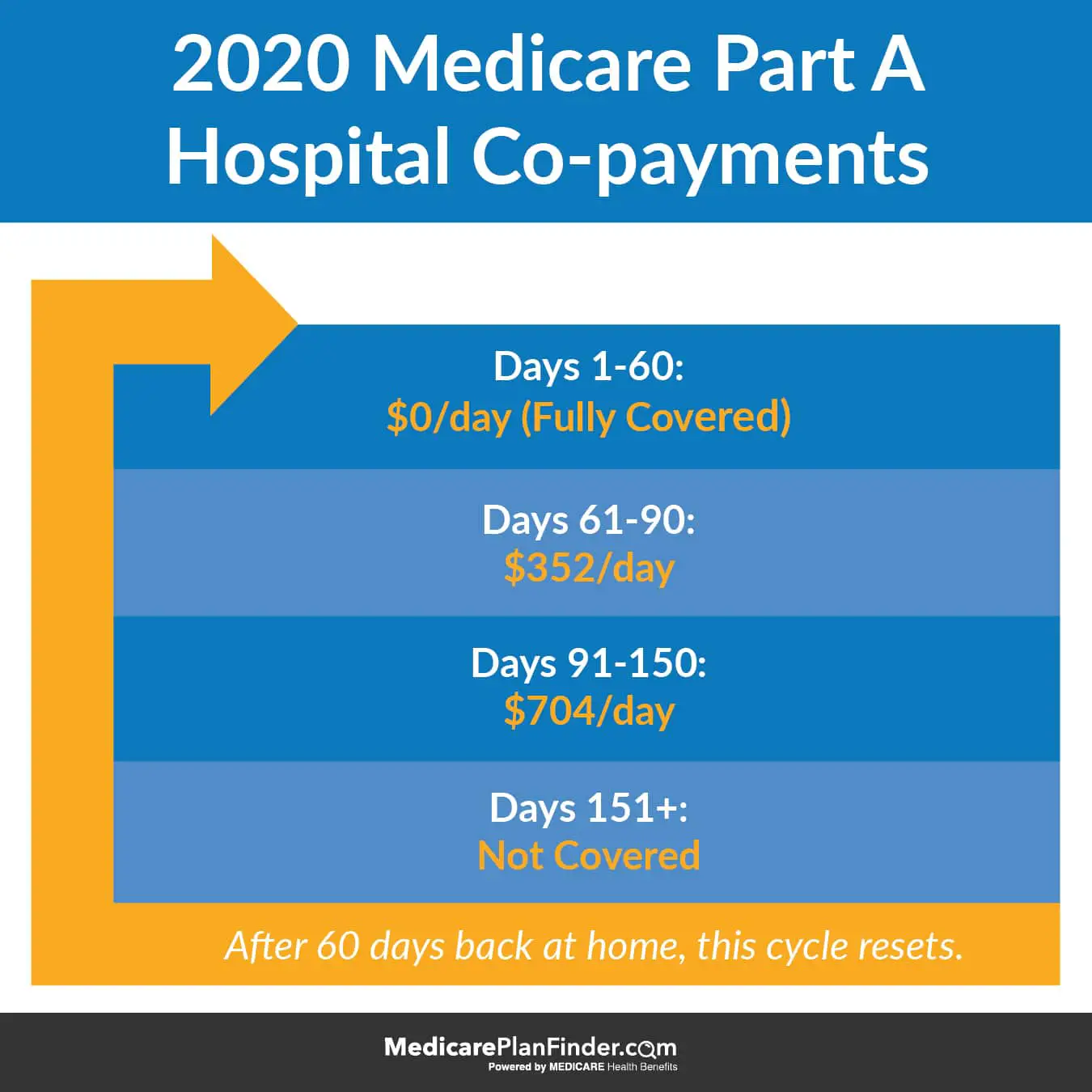
Inpatient psychiatric mental health care falls under Part A benefits. Further, Part A will cover a portion of the cost for the room, meals, nursing, and other services. You can obtain care in a hospital or psychiatric hospital.
But, the lifetime limit of inpatient psychiatric hospital care is 190 days. Also, you may incur costs for Part B while an inpatient in the hospital, this could be from doctor services.
Also Check: What Is Medicare Gap Insurance
Do Mental Health And Substance Use Disorder Parity Laws Apply To Medicare
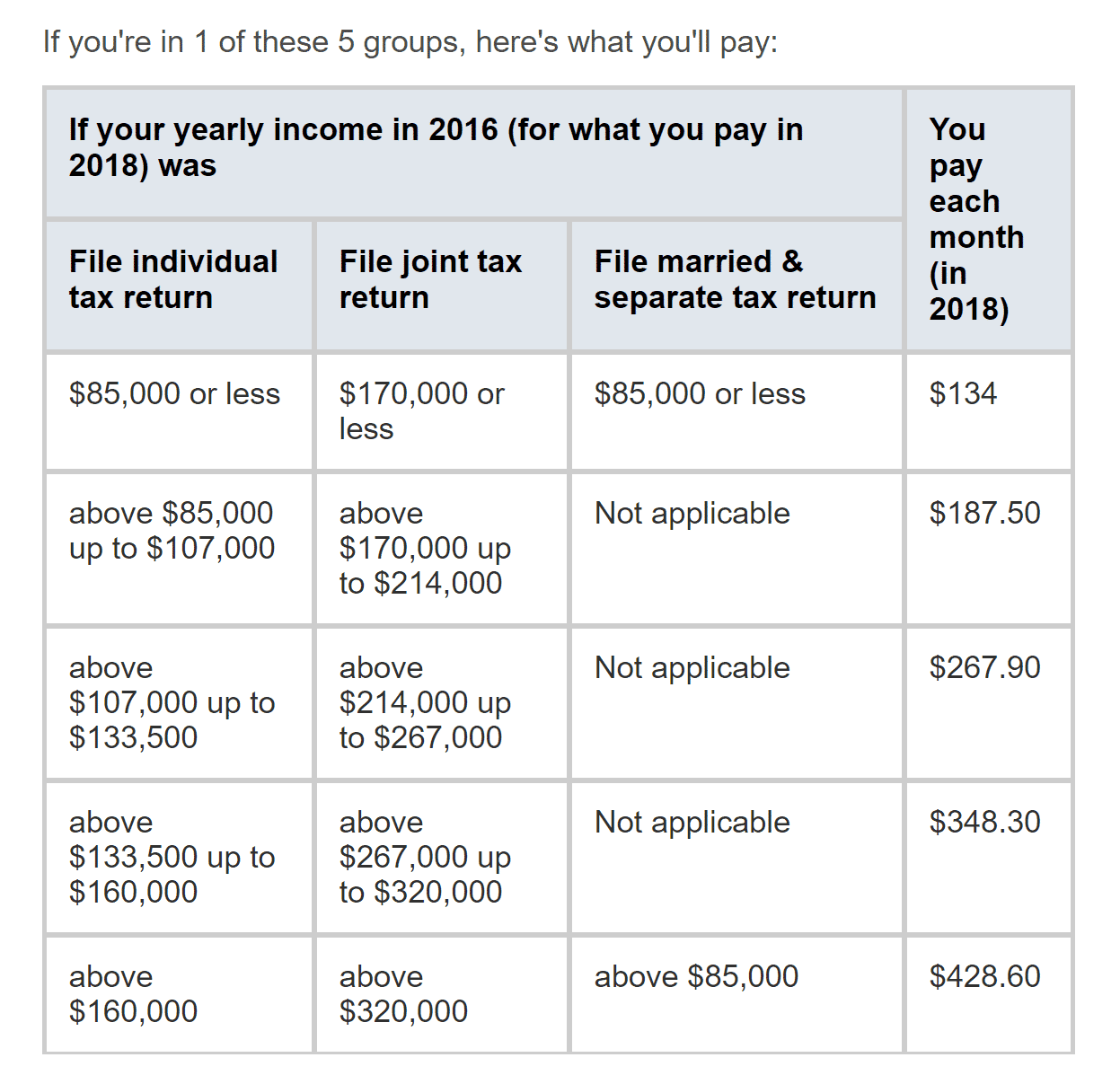
Prior to 2010, Medicare beneficiaries paid a higher coinsurance rate for outpatient mental health services than for other outpatient services covered under Part B . The Medicare Improvements for Patients and Providers Act of 2008 phased in parity for cost sharing for all outpatient services covered under Part B between 2010 and 2014, so that as of 2014, cost sharing for outpatient mental health services is the same as for other Part B services.
Federal parity laws, including the Mental Health Parity Act of 1996 and the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 , do not apply to Medicare, however. The Mental Health Parity Act of 1996 requires parity in annual and aggregate lifetime dollar limits for mental health benefits and medical or surgical benefits in large groups plans, but not Medicare. The Mental Health Parity and Addiction Equity Act of 2008 , which expanded on the 1996 law, extends parity to substance use disorder treatments, and prevents certain health plans from making mental health and substance use disorder coverage more restrictive than medical or surgical benefits, also does not apply to Medicare. In 2016, some of these parity rules were applied to Medicaid Managed Care Organizations but not to Medicare benefits that are provided by Medicaid MCOs to beneficiaries dually enrolled in Medicare and Medicaid.
Who Is Eligible For Medicare
People who work pay into Medicare during their working years through a payroll tax, then are eligible to enroll when they turn 65 years old. Youre eligible for premium-free Medicare Part A if you worked and paid into Medicare for at least ten years.
Its possible to get Medicare Part A at age 65 even if you havent worked, but youll probably have to pay out of pocket to cover your premium. The exception is if you are married to someone who paid into Medicare for ten years or more. In that case, you should still be able to get Part A without paying a premium.
How Long Have We Had Medicare?
Medicare was passed in 1965 to increase access to healthcare for Americas senior citizens. Most people in America enroll in Medicare when it becomes available to them at retirement age. Before Medicare was passed, 54 percent of elders aged 65 and over had health insurance. Now, 98.4 percent of elders in America have health insurance through Medicare.
Medicare also covers people who are younger than 65 when they have disabilities. People with end-stage renal disease or Lou Gehrigs disease can enroll in Medicare before they turn 65 years old.
People who qualify for Social Security Disability Income for any reason are eligible for Medicare 24 months after they start receiving SSDI.
You can inquire about your Medicare eligibility at your local Social Security office.
Read Also: Can I Get Medicare And Medicaid At The Same Time
Get Your Billing Handled
It’s our goal to ensure you simply don’t have to spend unncessary time on your billing.
You want to get paid quickly, in full, and not have to do more than spend 10 or 15 minutes to input your weekly calendar.
You want to know you can call your billing admin, a real person you’ve already spoken with, and get immediate answers about your claims.
You want to not have to deal with it!
Learn how to offload your mental health insurance billing to professionals, so you can do what you do best.
As private practitioners, our clinical work alone is full-time. Add in the unnecessarily difficult insurance billing system and we run the risk of working way over full-time. TheraThink provides an affordable and incredibly easy solution. My daily insurance billing time now is less than five minutes for a full day of appointments. My cost is a percentage of what is insurance-approved and its my favorite bill to pay each month! Denny and his team are responsive, incredibly easy to work with, and know their stuff. I cannot capture in words the value to me of TheraThink. Thank you. You free me to focus on the work I love!
Medicare Psych Reimbursement Rates By Cpt Code:
Medicare pays well! Find the rate that Medicare pays per mental health CPT code in 2022 below.
You can use these rate differences as estimates on the rate changes for private insurance companies, however its best to ensure the specific CPT code you want to use is covered by insurance.
Call and verify eligibility and benefits or hire a billing team to take care of it for you.
Don’t Miss: What Are The Five Steps In The Medicare Appeals Process
Medicare Reimbursement For Therapy By State
Enjoy learning about the comparative difference in Medicare Reimbursement Rates for Therapy by State. Youll learn how Medicare divides each state and territory by locality, what Medicare pays for CPT Code 90791, and which localities pay the most.
The data below represents Medicare 2022 reimbursement rates for a diagnostic interview by a licensed mental health professional. Reimbursement rates depend on license level, professional vs facility services, and payment modifiers that may or may not apply.
| State | CPT Code 90791 Reimbursement Rate 2022 | Reimbursement Compared to National Rate |
|---|---|---|
| NATIONAL | ||
| SANTA CLARA | $224.26 | |
| SAN JOSE-SUNNYVALE-SANTA CLARA | $225.09 | |
| SAN FRANCISCO | $219.23 | |
| SAN MATEO | $219.23 | |
| OAKLAND-BERKLEY | $219.23 | |
| RIVERSIDE-SAN BERNARDINO-ONTARIO | $202.15 | |
| SACRAMENTO-ROSEVILLE-ARDEN-ARCADE | $202.86 | |
| LOS ANGELES-LONG BEACH-ANAHEIM | $209.34 | |
| SAN LUIS OBISPO-PASO ROBLES-ARROYO GRANDE | $201.63 | |
| HAWAII, GUAM, AMERICAN SAMOA, MARSHALL ISLANDS, PALAU, NORTHERN MARIANA ISLANDS, FEDERATED STATES OF MICRONESIA | $201.98 | |
| PORTLAND | $199.43 | |
| METROPOLITAN ST. LOUIS | $193.86 | |
| METROPOLITAN KANSAS CITY | $192.91 | |
| SUBURBAN CHICAGO | $201.46 | 103.07% |
| IL – Illinois | EAST ST. LOUIS | $195.81 |
| NEW ORLEANS | $194.52 | |
| DETROIT | $198.15 | |
| MIAMI | $203.91 | |
| FORT LAUDERDALE | $199.41 | |
| ATLANTA | $194.94 | |
| 100.72% | ||
| DC – Washington, DC | DC + MD/VA SUBURBS | $215.43 |
| NORTHERN NEW JERSEY | $211.50 | |
| METROPOLITAN PHILADELPHIA | $203.36 | |
| NYC SUBURBS/LONG ISLAND | $220.07 | |
| POUGHKPSIE/N NYC SUBURBS | $207.12 | |
| SOUTHERN MAINE | $193.75 | |
| METROPOLITAN BOSTON | $211.15 |
Does Medicare Cover Mental Health Medications
Under Original Medicare, prescription drugs form a unique category and are usually not covered if they are self-administered. This is also the case when it comes to psychiatric medications, such as antidepressants, anticonvulsants, and antipsychotic medications. To get prescription psychiatric drugs covered, you will need to have a Medicare Part D prescription drug plan.
These plans are offered by private insurance companies, not by the U.S. government. For this reason, youll need to shop around and find a Medicare prescription drug plan that works for you. Each plan will usually cover slightly different drugs, so make sure that the plan you choose covers everything you need.
Don’t Miss: What Is A Coverage Gap In Medicare
Does Medicare Cover Inpatient And Outpatient Mental Health Services
Original Medicare consists of Medicare Part A and Part B . You will have access to inpatient and outpatient mental health services under Medicare Part A and Part B. Both may have deductibles and coinsurance.
Medicare Part A provides for inpatient services. These are for hospitals and psychiatric facilities.
You get coverage for the following:
-
Toothpaste, razors, and other personal items
-
TV or phone for your room
Medicare And Mental Health Benefits
The human body is a complex and highly sophisticated system that has many delicate parts working in harmony. The command center for this entire system is, of course, the brain, which is why mental health is so crucial to overall well-being. As you grow older, life and tough circumstances can lead to issues such as depression, anxiety and more. The good news is that these ailments are treatable. Health sciences have already come a long way and continue to grow as doctors and scientists work hard to discover new ways to alleviate mental health issues. There is effective treatment already available for so many mental health issues, with more being developed as time goes on.
If you are on a Medicare health coverage plan you may be wondering, does Medicare cover mental health? The simple answer is yes. However, there are limitations and specific terms involved in the process. Heres everything you need to know about what Original Medicare Parts A and B cover in terms of mental health treatments.
Also Check: How Old Do You Need To Be To Collect Medicare
Medicare Reimbursement Rates For Psychotherapy
Please see our updated Medicare Rates:
| CPT Code |
|---|
| $42.17 | $25.30 |
The reduced rate here isnt the exact amount Medicare pays out but represents a rough estimate of the suggested reduction to expect from Medicare. In our experience, Medicare over-estimates the contracted rate for most private insurance companies so their total reduction, while large, still leaves providers with a modest but much higher earning than Medicaid.
Part of the reason why is Medicare is more selective with their network.
Medicare Coverage Of Mental Health Services
A persons mental health refers to their state of psychological, emotional, and social well-being and its important to take care of it at every stage of life, from childhood to late adulthood. Fortunately, Medicare beneficiaries struggling with mental health conditions may be covered for mental health services through Medicare. Mental health services are a system of care that aim to assess, diagnose, treat, and counsel in an individual or group setting anyone who needs help alleviating mental or emotional illness, symptoms, conditions, and disorders. Find out what is included in your Medicare coverage for mental health services and get the help you or a loved one need.
You May Like: How To Become A Medicare Insurance Broker
Kathleen Cameron Senior Director At Ncoa
adults have been impacted pretty significantly, particularly by the social isolation and loneliness that they experience that could have exacerbated existing conditions that they had or in some cases, new diagnosis of depression, anxiety, sleep problems happened during the pandemic
For those on Medicare, knowing what mental health services are covered can make seeking help more daunting. Medicare beneficiaries might be aware that they have some sort of mental health coverage, but may not understand what it entails regarding services, co-payments, and prescriptions, says Lindsay Malzone, Medicare expert at Medigap.com.
To help navigate the ins and outs of Medicare, experts share insight.
Additional Depression Treatment Options
There are some additional depression treatment options seniors can consider, though these options are not typically covered by Medicare.
- Electroconvulsive therapy, or electroshock therapy, is typically used in cases of severe depression where the risk of suicide or harm to others is very high.
- Transcranial magnetic stimulation is often used to treat major depression in people who have already tried antidepressants. An electromagnetic coil is placed over the scalp and creates a magnetic field that stimulates the nerves in the prefrontal cortex, which is the area of the brain that controls mood.
- Vagus nerve stimulation is a treatment used when most other options have failed. A device similar to a pacemaker is implanted into the chest with wires leading to the vagus nerve of the neck. The device sends regular electrical currents to the nerve, which is responsible for relaying information to the brain.
- Exercise has been shown by research to fight depression and is a treatment option that comes free of cost and can even be made easier with the help of a Medicare Advantage plan that offers fitness club memberships. High-intensity exercise releases endorphins, which are the bodys positive chemicals responsible for whats commonly called a runners high. Low-intensity exercise sustained over time releases neurotrophic proteins that promote growth in brain function and can make you generally feel better.
Compare Medicare Advantage benefits in your area
About the author
Read Also: Does Medicare Cover Aquatic Therapy
