Does Medicare Cover Diabetic Supplies
- Medicare Part B covers certain diabetic supplies and preventive screenings.
- Medicare Part D covers oral diabetic medications, injectable insulin, and self-injection supplies.
- Get prescriptions from your doctor for any medication, supply, or service youll want Medicare to cover.
- Check that your pharmacy or device supplier accepts Medicareset payment rates to avoid overpaying.
Diabetes is a metabolic condition that leads to high blood sugar levels. Most people who have diabetes have type 2 diabetes. According to the American Diabetes Association, around 14 million Americans 65 and older have diabetes, some who are undiagnosed.
Older adults with diabetes face unique challenges including hypoglycemia, brain and nervous system problems, and social support issues that require special monitoring to manage risks.
There are many types of diabetic supplies needed for preventive screening, monitoring, and managing the condition. Medicare has several parts that cover different types of supplies and services. Cost and coverage depend on the type of plan.
What Diabetes Supplies Does Medicare Cover
The diabetes equipment and supplies that are covered by Medicare Part B include the following:
-
Blood sugar test strips
-
Blood sugar testing monitors
-
Lancet devices and lancets
Medicare Part B also provides coverage for some services for people with diabetes:
-
Training in diabetes self-management
-
Medical nutrition therapy services
How To Get Diabetic Supplies With Medicare
You can get diabetic supplies at your local pharmacy or through an approved medical equipment supplier. In order for the item to be covered, you’ll need a prescription from your doctor.
-
If you have Medicare Part B, we recommend you start your search with the Medicare.gov medical equipment and suppliers directory, which provides a Medicare-approved list of diabetic suppliers. The directory includes both products available locally and mail order diabetic supplies, which are labeled “mail order” next to the product name.
It’s important to ask the pharmacy or supplier if it accepts the Medicare assignment so you don’t face any additional costs. In addition to your prescription, coverage for some supplies may require a Certificate of Medical Necessity provided by your doctor.
-
If your coverage is through Medicare Advantage or Medicare Part D, check with your plan’s list of approved in-network pharmacies and suppliers. Where you get your prescription can determine whether you have coverage. Your plan may even offer financial discounts if you shop at a preferred pharmacy.
You’ll still need a prescription before making a purchase, and in some cases, you may also need preapproval from the insurance company. Check your plan’s summary of benefits to see what’s required.
Read Also: What Are My Medicare Premiums
How To Learn More
- For more information on all of the options available under Medicare, visit: www.medicare.gov or call 1-800-MEDICARE . Also look for the Medicare and You handbook which Medicare mails to beneficiaries in the fall and is available by calling 1-800-MEDICARE .
- To read more about Medicare coverage of diabetes services and supplies, go to .
- For information from Medicare on how individuals might be able to get help paying Medicare costs visit www.medicare.gov/your-medicare-costs/help-paying-costs/get-help-paying-costs.html or call 1-800-MEDICARE .
- Free health insurance counseling and personalized assistance for Medicare beneficiaries is available in every state through the State Health Insurance Assistance Program . Call 1-800-MEDICARE or visit www.shiptacenter.org to find the telephone number of the SHIP office closest to you.
Therapeutic Shoes And Inserts Under Medicare
Medicare Part B may also cover therapeutic shoes or inserts if you need them for your diabetes, but you have to meet certain conditions. You may qualify for one pair of depth-inlay shoes and three pairs of inserts per year.
If you cant wear depth-inlay shoes, Medicare may pay for one pair of custom-molded shoes and two pairs of inserts.
You have to meet certain conditions, including being diagnosed with diabetes, are in a comprehensive treatment plan and require the shoes and inserts.
You also must have at least one of these conditions:
- Diabetes-related nerve damage with signs of callus problems
- Partial or complete foot amputation
- Poor circulation
You will also need a podiatrist or other qualified health care professional to prescribe the shoes and to fit and provide them.
Recommended Reading: How To Determine Medicare Eligibility
Medicare And Diabetes Coverage
Home / FAQs / Medicare Coverage / Medicare and Diabetes Coverage
Medicare and diabetes coverage is a concern for many Americans. Diabetes can cause a persons health and well-being to deteriorate over time. Close monitoring is often necessary because diabetes causes other health concerns and conditions. Below we go into full detail about what you need to know regarding Medicare and diabetes coverage.
Read Also: Does Medicare Help Pay For Mobility Scooters
Insulin Pumps Covered By Medicare
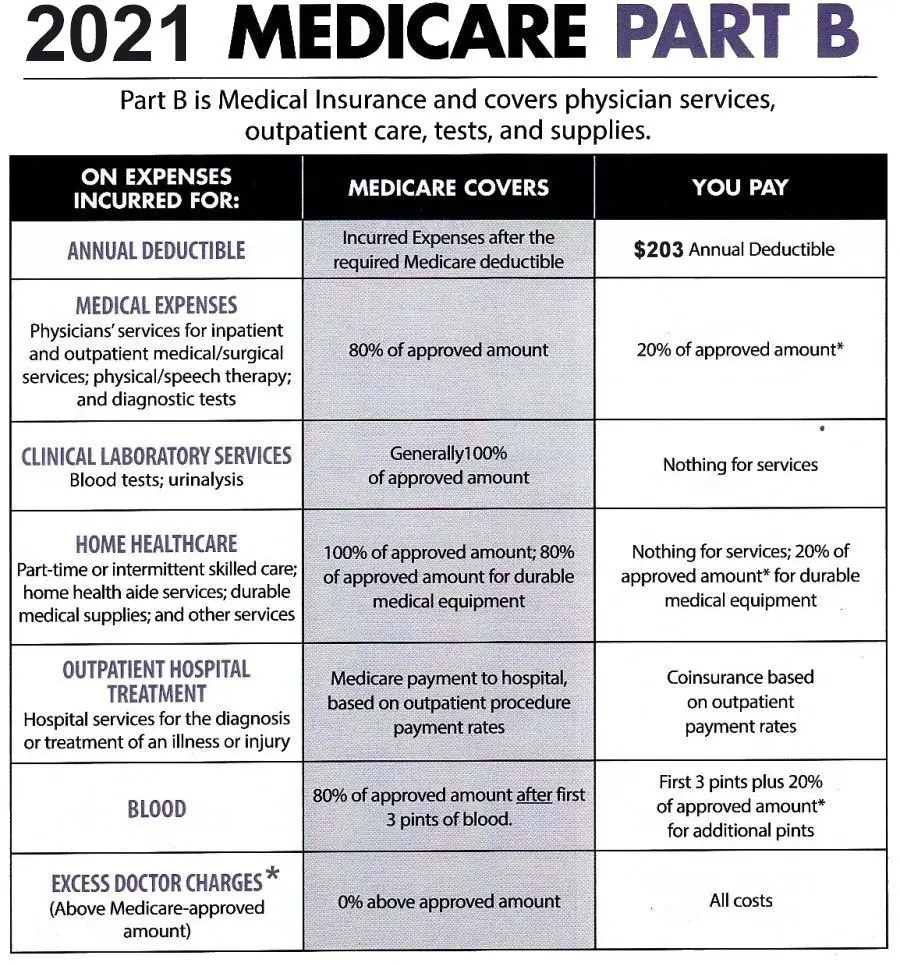
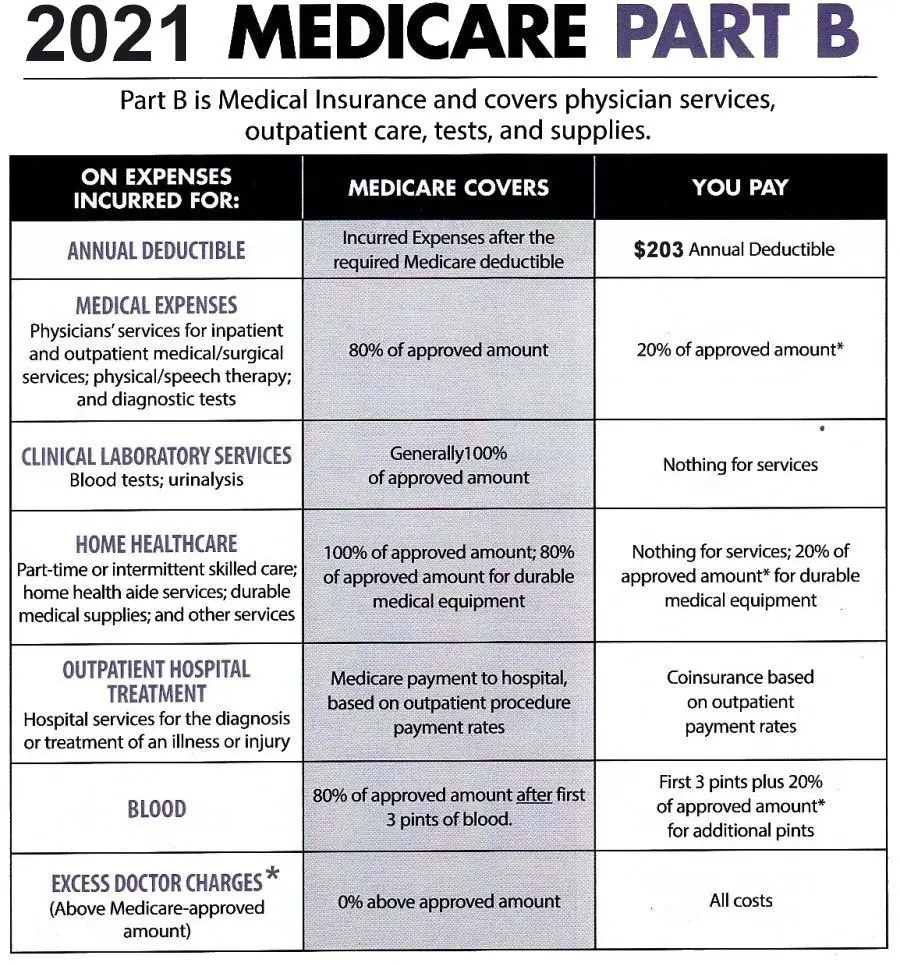
If you need a tubed insulin pump , it may be covered under Medicare Part B if you have diabetes and meet certain conditions. The same holds true for the insulin used to fill these pumps. Under Original Medicare, youll need to pay 20 percent of the amount approved by Medicare for these products after your annual Part B deductible. Medicare will cover the remaining 80 percent.
Medicare Part B covers the Tandem t:slim X2. Meanwhile, tubless options including the Insulet OmniPod, OmniPod DASH, and the brand new Omnipod 5 are covered under Medicare Part D. Of course, all of these insulin pump options are available from US MED!
You May Like: Do Medicare Advantage Plans Cover Cataract Surgery
How To Get Diabetes Supplies Through Medicare Part B
To get your diabetes supplies under Medicare Part B, you need a prescription from your doctor. The prescription should state:
Simply hand one of the Medicare cards shown here and your prescription to your pharmacist when you go to the pharmacy.
The Best Diabetic Supply Companies Of 2022
- Best for Medicare and Medicaid Insurance: Edgepark
- Best Support for Medtronic Users: Medtronic
- Best for Specialized Insulin Pump & Technology: Tandem
- Best for Pediatric Population: Insulet
- Best for Replacements: Dexcom
-
Will review all your insurance options to help save money
-
May not be available to all types of Medicare plans
-
Pump users may be locked into warranties
Why we chose it: Many health professionals and people living with diabetes recommended Byram Healthcare to us for diabetes supplies. Its deliveries are very reliable and because it offers so many products, it may serve as a one-stop-shop for diabetes supplies. Priding itself on convenience, affordability, and choice, Byram Healthcare offers a comprehensive product line of diabetes supplies ranging from diabetes test strips, lancing devices, lancets, control solution, batteries, blood glucose meters, insulin pump supplies, continuous glucose monitor supplies, insulin and pen needles, and more.
Recommended Reading: How Long Can You Stay In The Hospital Under Medicare
How Much Do Testing Supplies Cost
If youve met your Part B deductible , you will pay 20 percent of the Medicare-approved amount for diabetic testing supplies. Medicare pays the other 80 percent.
Depending on the type of equipment or supplies you need, you may need to:
- rent the equipment.
- buy the equipment.
- choose whether to rent or buy the equipment.
Additionally, your durable medical equipment will only be covered if your doctors and DME suppliers are enrolled in Medicare. You must also purchase your testing supplies from a supplier who accepts assignment. In this case, they can only charge you the coinsurance and Part B deductible.
Accepting assignment means the supplier agrees to be paid directly by Medicare and accepts the payment amount Medicare approves for the service. The Medicare-approved amount is the amount a supplier can be paid by Medicare, and you pay the rest.
To ensure your supplier is enrolled in Medicare, ask if they participate in Medicare before you order the supplies.
How much you will specifically pay for supplies depends on a variety of factors such as:
- Other insurance you may have.
- How much your doctor charges.
- Where you get your supplies.
- Whether your doctor and supplier accept assignment.
What Does Part D Cover
Medicare Part D will cover medications such as insulin and the tools like needles and syringes you need to inject your insulin. It also covers your routine medications at home.
- Medical supplies to administer insulin
- Inhaled insulin devices
Part D is a private plan, and you must be enrolled in Part A or B to be eligible.
Recommended Reading: Does Medicare Cover Hospital Bills
How Do I Get Free Diabetic Supplies
Its no secret that diabetic supplies can get pricey. Buying glucose monitors, test strips, and insulin can add up fast. Thankfully Medicare has you covered if you know how to get the right supplies.
To receive free diabetic supplies youll need to work closely with your doctor to get appropriate supplies. Your doctor will write you a prescription for all the supplies, equipment, and medication you need.
Your doctor will help you find the right blood sugar monitor for you and explain how often you should test your blood sugar levels. Theyll also determine how many lancets or test strips youll need in a month. You wont get coverage for any additional supplies that your doctor doesnt prescribe.
Youll need to get a new prescription for diabetes supplies every year. This is a great time to evaluate your treatment and make sure its right for you.
D Senior Savings Model
Coinsurance also applies every time you fill your prescriptions for insulin or other medications. Copayments depend on your Part D plan and what medications are covered by your plan formulary.
If youre over 65, you can get additional savings by enrolling in the Part D Senior Savings Model. This plan puts a cap on out-of-pocket spending for insulin. You can choose between several covered types of insulin, and your co-payment is capped at $35 for a 1-month supply.
What extra benefits and savings do you qualify for?
Read Also: Does Medicare Cover Toenail Removal
Does Medicare Cover Insulin
Medicare Part B will not coverinsulin unless it is used in an insulin pump. Medicare Part B also does not cover certain medical supplies used to administer insulin such as syringes, needles, insulin pens, alcohol swabs or inhaled insulin devices.
Medicare does not cover anti-diabetic drugs used to maintain blood sugar.
How Do I Cope With Finding Out I Have Diabetes
If youve recently received a diabetes diagnosis, take a big breath. Its easy to feel overwhelmed, but youre not alone. There are several ways you can cope with finding out you have diabetes and help you focus on maintaining your health.
- Start by talking to your doctor. Theyre the best source of information about your diabetes. Theyll help you make a treatment plan and make sure you get the supplies you need to manage diabetes.
- Talk to your family and friends and tell them how youre feeling. Be honest about your emotions and ask for help. Just telling someone else about your diagnosis can relieve stress.
Get the health benefits and savings youre entitled to.
Recommended Reading: How To Find My Medicare Claim Number
Does Medicare Part B Pay For Insulin Needles
However, if the beneficiary injects their insulin with a needle , Medicare Part B does not cover the cost of the insulin, but the Medicare prescription drug benefit covers the insulin and the supplies necessary to inject it. This includes syringes, needles, alcohol swabs and gauze.
Thousands of people suffering from erratic blood sugar has been using this ground-breaking solution
To help them burn away dangerous fat from their vital organs and bellies
While stabilizing their blood sugar levels naturally and effectively.
And starting today
How Does Medicare Cover Diabetes
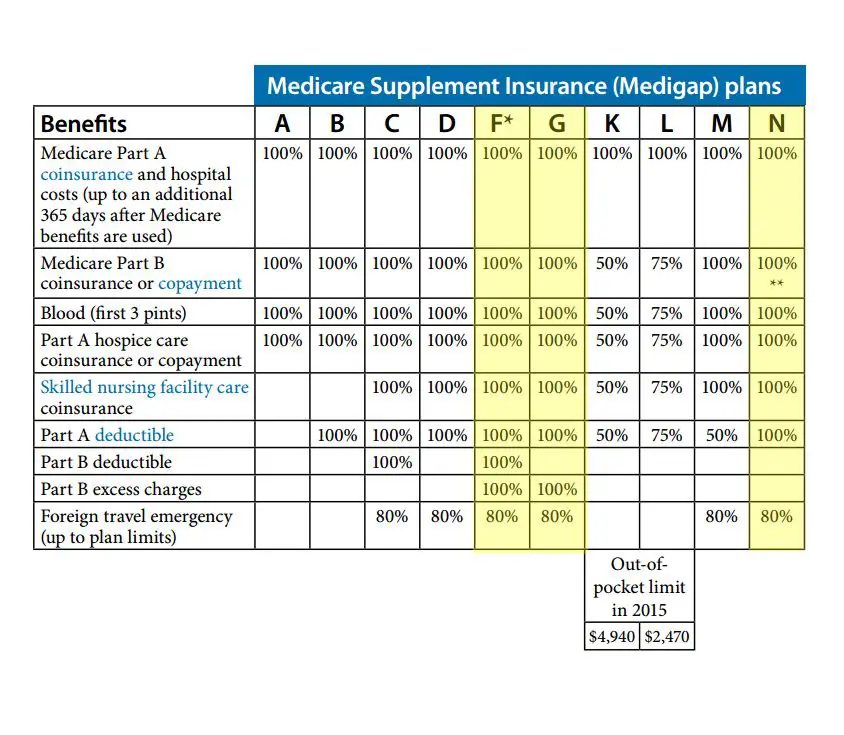
Different parts of Medicare cover different services and supplies. That said, some things arent covered by Medicare, and in many cases, you will pay a portion of the cost, unless you have another insurance plan that covers it.
Medicare coverage for diabetes would usually be obtained by enrolling in Original Medicare or a Medicare Advantage plan .2
Read Also: Does Medicare Cover Medical Emergencies In Foreign Countries
Keeping Health Insurance After Leaving A Job
A federal law called COBRA allows you to stay on your employers health plan for 18 to 36 months after leaving a job. Youll pay both your own monthly premiums and the employers portion, so your cost is likely to be higher than before.
- People with a disability may be able to extend COBRA coverage for an extra 11 months.
- COBRA may also cover young adults who age out of a parents policy when they reach the age limit of 26.
Learn more about COBRA online or call the U.S. Department of Labor at 18664USADOL .
Medicare & Diabetic Supplies: Coverage And Best Plans
Find Cheap Medicare Plans in Your Area
Diabetic supplies are covered by Medicare when they’re medically necessary and when you have a prescription.
Medicare Part B covers screenings, doctor exams, glucose monitors and diabetic shoes. Medicare Part D covers insulin and diabetes medications. And Medicare Advantage plans bundle all your coverage within a single plan.
Beginning in 2023, insulin copays will be capped at $35 per month, as a result of a change in federal law.
Also Check: Can I Sign Up For Medicare Supplement Anytime
How Do I Know Which Diabetic Supplies My Medicare Advantage/prescription Drug Coverage Plan Will Cover
Knowing which types of diabetic supplies that your Medicare plan will cover is crucial. In order to learn which diabetic supplies and diabetic testing supplies Medicare covers under your Part C or Part D plan, youll need to do any of the following:
- Read the coverage materials that you received when you purchased your plan.
- Visit your insurance providers website and sign in to their beneficiary portal to find out which diabetic supplies are covered by your plan.
Some Medicare Advantage insurance providers offer what are known as Special Needs Plans, or SNPs. SNPs provide additional or specific services for beneficiaries with chronic conditions, including diabetes. As always, the coverage may vary, but a diabetes SNP can offer additional benefits that Original Medicare or other Advantage plans may not provide, including assistance with supplies.
When it comes to obtaining the supplies you need to help keep your diabetes under control, never leave what your plan covers up to guesswork. The diabetic supplies that you need may be covered by your Medicare plan. All it takes is a simple phone call, a few moments to read your plan booklet, or the click of a mouse to find out.
Are Diabetes Testing Supplies Covered By Medicare
Traditional blood sugar monitors, test strips, lancets, and control solutions are all covered under Medicare Part B. If youre a Medicare patient with diabetes who uses insulin, you can get up to 300 lancets and 300 test strips every three months.
Medicare patients with diabetes who dont use insulin can still get these products, but not in the same amount. Instead, theyre eligible for 100 lancets and test strips in a three-month period.
The True Metrix Air, Prodigy AutoCode, and Embrace glucose meters are all covered by Medicare and available from US MED. We also sell test strips and control solutions compatible with these meters.
Also Check: Can You Qualify For Medicare Through Your Spouse
When It Comes To Diabetes What Does Medicare Advantage Cover
In order to understand Medicare Advantage diabetes coverage, itâs important to first understand what Original Medicare covers for diabetes. The Centers for Medicare & Medicaid Services reports that Original Medicare offers coverage many basic diabetes supplies, including:
- Annual diabetes prevention, screening, and wellness checks
- Blood sugar monitoring equipment such as lancets and blood glucose monitorsâwith limits on which supplies you can use or how often you can buy them
- Durable insulin pumps and the accompanying insulin, under certain conditions
- Diabetes-related foot care for those who have peripheral neuropathy and a loss of protective sensation, including foot exams as well as orthotic diabetes shoes and inserts
Medicare Advantage plans are an alternative to Original Medicare. Advantage plans are supplied by private companies that must follow Medicareâs rules and regulations. While all Advantage plans must offer all of the benefits of Original Medicare, they may come with different rules, costs, rights, protections, and options.
Many Medicare Advantage plans provide benefits you cannot get with Original Medicare. According to the Centers for Medicare and Medicaid Services, some Medicare Advantage plans cover additional diabetes supplies and services, including:
With Medicare Advantage, youâll also have an annual out-of-pocket limit that may help you spend less on health care.
What Other State Programs Can Help
Medicare Savings Programs in certain states may pay Medicare premiums, deductibles, and coinsurance if a person has a low income and few assets. Learn more online.
State Health Insurance Assistance Programs give advice about health insurance in every state to people who have Medicare. SHIP counselors can help you choose the best plan for your needs. Find a SHIP counselor at ShiptaCenter.org or call 1-877-839-2675.
-
Phone: 1-800-872-5827 or 202-776-0406
You May Like: How To Appeal Medicare Part B Late Enrollment Penalty
Does Medicare Cover Diabetes Shoes
Medicare pays for therapeutic shoes and inserts when necessary. Patients often need shoes because diabetes takes a toll on the feet and circulation. Medicare pays for the shoes when a qualifying doctor prescribes diabetic shoes.
However, compression stockings dont receive Medicare coverage.
Medicare pays for one of the following each year:
- One pair of depth-inlay shoes + 3 pairs of shoe inserts
- One pair of custom-molded shoe
- patients that are unable to wear the custom shoes because of a foot deformity may substitute for two extra shoe inserts
Some instances allow Medicare to cover separate shoe adjustments instead. When your treating doctor certifies that you meet the three following conditions, Medicare will pay for your therapeutic shoes.
You must have one of the following in one foot or both:
- Partial or complete foot amputation
- History of foot ulcers
- Deformity of the foot
