Top Rated Assisted Living Communities By City
Medicare will cover 100% of the costs for medically necessary home health care provided for less than eight hours a day and a total of 28 hours per week. The average cost of home health care as of 2019 was $21 per hour.
Many seniors opt for home health care if they require some support but do not want to move into an assisted living community. For seniors who are generally in good health but require help with the activities of daily living, or someone to remind them to take medication, home health care is a viable solution.
Helpful Resources
How To Obtain Medicare Home Care
Most often, Medicare consumers receive home care from CHHAs. To obtain care, a doctor must fill out paperwork to validate the need for home health care. CHHAs then send a nurse to evaluate the patient and determine the services they require. Medicare consumers in the community who needs home health care can contact a local CHHA, which will likely be happy to assist them with obtaining the required paperwork so they can access care.
If someone is in a hospital or rehabilitation center and will need home health care upon their return home, a discharge planner at the facility will usually help with arranging these services. If you or a loved one are in this position, be sure to speak with the discharge planner about home health care arrangements upon the return home.
What Does Medicare Home Health Not Cover
Round the clock care at home
Prescription medication
Homemaker services- shopping, cooking, cleaning etc.
Personal care by an aide when it is the only care needed
Medical services or supplies that Medicare doesnt pay for
20% of the Medicare-approved cost for Medicare-covered equipment For more information visit: Medicare.gov
If you or a loved one are in need of information related to your Medicare Home Health Benefits, Contact Us today or call 561-989-0441 for your free consultation.
Recommended Reading: Is Shingrix Vaccine Covered By Medicare
Does Medicare Cover Custodial Care
Medicare may not pay for personal or custodial care, which includes the six activities of daily living: toileting, bathing, eating, dressing, transferring, and continence. Medicare will cover these services only if you also need other covered home health care services, and only if you need part-time care.
Does Medicare Help With Family Caregivers
With the advancement of nutrition science, medical research and healthcare technology, seniors today have been blessed with longevity uncommon in past generations. However, many people need assistance due to age, illness, or injury. Access to caregivers depends heavily on residential location and financial resources. Some Medicare recipients are fortunate enough to have family members care for them and want to know if Medicare can help.
Benefits for Medicare Recipients Who Need Care at HomeOriginal Medicare is structured to cover costs incurred during hospital stays and medical office visits . Medicare recipients may be eligible for part-time skilled care if they are homebound and meet specific criteria. If you qualify for home health services, Medicare Part A benefits include medically necessary part-time or periodic skilled care delivered by a nurse, physical therapist or speech-language pathologist. The home health agency servicing you must be Medicare-certified, meaning they are approved by Medicare and accept assignment. If Medicare approves the claim for home health services, the authorized fees may be covered.
Custodial Care for Day-to-Day LivingMedicare benefits do not include custodial care, which is help with the activities of daily living, when that is the only care needed. This includes bathing, personal hygiene, dressing, eating, toileting and transferring to or from a bed, chair or wheelchair.
Related articles:
Also Check: When Is The Enrollment For Medicare
How Do I Know If I Qualify For Medicare Home Health Care
It is common for an elderly person to need assistance upon discharge from a hospital or in-patient rehabilitation stay. That individuals physician, sometimes in concert with family members and the patient him/herself, would determine the in-home health care need and complete paperwork that refers the patient to home health care.
Other common situations include the slow physical decline elderly people experience when that decline includes inability to care for oneself on a daily basisbut nursing home care is not yet requiredthe physician may recommend home health care for just those tasks the senior is unable to perform.
These four conditions must be met before home health services can be prescribed and covered by Medicare:
1. Your doctor must decide that you need medical care in your home, and make a plan for your care at home and
2. You must need at least one of the following: intermittent skilled nursing care, or physical therapy or speech-language pathology services or continue to need occupational therapy and
3. You must be homebound or normally unable to leave home & leaving home takes a considerable and taxing effort. A person may leave home for medical treatment or short, infrequent absences for non-medical reasons and
4. The home health agency caring for you must be approved by the Medicare program. If you or a loved one are in need of information related to your Medicare Home Health Benefits, Contact Us today or call 561-989-0441 for your free consultation.
What Is A House Call Doctor
A house call doctor, or house call physician, is simply a doctor who performs medical visits in the patient’s place of residence. House call doctors may be employed by an agency, or they may have their own practice.
What Are the Benefits of Physician House Calls?
The primary benefit of physician house calls is that patients receive quality care, from qualified physicians, in the comfort and convenience of their own home or place of residence. Additional benefits of physician house calls include the following:
- It ensures regular medical care to patients who have few or no other options
- It helps monitor and treat both preventable and chronic conditions to keep patients out of ERs and hospitals
- It encourages patients to keep up with regular medical visits by bringing the doctor directly to the patient’s home
- It saves the patient time and money traveling to the doctor’s office
Though there are many benefits associated with medical house calls, there are also some challenges, namely that house calls are not ideal for emergency medical problems, and availability of physicians and scheduling options may be limited in some areas.
How Often Do House Call Doctors Visit?
House call visits can be scheduled as often as required by the patient, but on average patients are seen on a monthly basis. Visits are typically scheduled on weekdays, though the physician may be available by phone on weekends or after hours.
Also Check: How Do I Cancel Medicare Part A
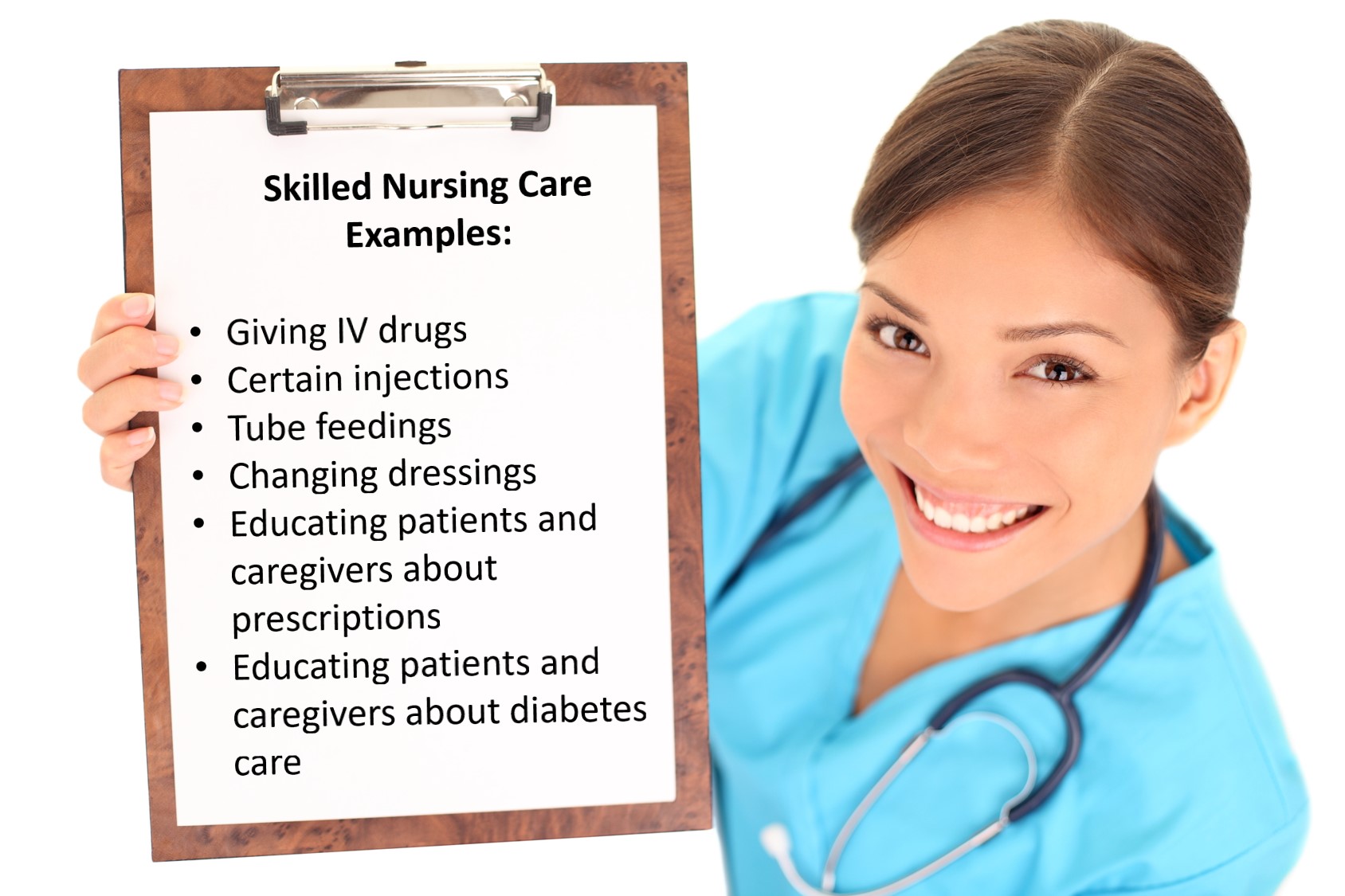
Is Skilled Nursing Care Covered
Medicare covers intermittent nursing services. This means that nursing care is provided fewer than seven days a week, or for less than eight hours a day, up to a limit of 21 days. In some cases, Medicare will extend the window if your doctor can provide an accurate assessment of when the care will end.
Skilled nursing services are usually employed to help treat an illness or assist the patient with recovering from an injury. The nurse needs to be licensed to administer the medical treatment you need .
Home Health Care Not Covered Under Medicare
While Medicare pays for many aspects of home health, not all services are covered.
Medicare does not pay for:
- 24-hour home care
- Meals delivered to your home
- Homemaker services, such as grocery shopping or housework
- Personal care such as bathing, dressing and eating when this is the only care you need
Don’t Miss: Does Medicare Have Long Term Care Insurance
Does Medicare Advantage Cover Home Health Care
Yes, Medicare Advantage plans cover home health care at the same level as Original Medicare. But Medicare Advantage plans may impose added rules, limitations and costs. Your plan may:
- Restrict your care to plan-contracted providers
- Require prior authorization or a referral from your family doctor on top of the mandatory Medicare certification
- Charge deductibles, copays or coinsurance
There’s only one home-care related benefit that sets Medicare Advantage apart from Original Medicare: meal delivery. But not every Medicare Advantage plan offers it, and the benefits vary by plan: For example, one plan provides meals only for patients with a specific medical diagnosis. As a result, we don’t recommend choosing Medicare Advantage based on this benefit alone.
In general, we found the Original Medicare home health benefit to be the better option for home care due to full coverage and fewer potential roadblocks to receiving care. Medicare Advantage plans may limit provider choice, assess fees or require referrals and preauthorizations for care. Medicare Advantage plans add very few extras for home health care or durable medical equipment when needed as part of home care.
Improve Medicare For All Beneficiaries
Medicare is extremely popular, but it needs attention to ensure all beneficiaries receive comprehensive coverage and equitable treatment. The Medicare program that Americans know and cherish has been allowed to wither. Traditional Medicare, preferred by most beneficiaries, has not been improved in years, yet private Medicare Advantage plans have been repeatedly bolstered. Its time to build a better Medicare for all those who rely on it now, and will in the future.
You May Like: What Age Can You Get Medicare Part B
Is A Hysterectomy Covered By Medicare
Hysterectomy is covered under Medicare. With Medicare, there are little to no out of pocket expenses for hysterectomy surgery if you are a registered public patient and have surgery in a public hospital. Depending on how quickly you need to have surgery, you may consider going private for speedier treatment.
Find A Home Health Care Provider
You can search for a provider by using the online home health care provider tool at Medicare.gov. Just enter your zip code and the tool will give you a list of home health care providers in your area. You can also ask your doctor, hospital social worker or discharge administrator to arrange for a home health provider in the event you need home care after a hospital stay.
Dont let an injury or illness prevent you from getting the help you may need. Talk to your doctor and ask if you qualify for home health care.
Don’t Miss: Can You Go On Medicare If You Are Still Working
How To Get Home Health Care
There are several ways to apply for home health care, but the first step is to have your doctor evaluate your condition and draw up a home health care plan. Once you have a physician-prescribed plan, you can contact your health insurance company or work directly with an agency to establish service.
Before applying for home health care, make sure you meet all eligibility requirements.
Who Qualifies for Home Health Care?
There are rules for how to qualify for home health care, especially if you want it to be covered by your insurance or Medicare plan. In order to be eligible, you must meet these requirements:
- Be under the care of a physician who orders home health services
- Meet the definition of “homebound”
- Require skilled nursing or therapy services on an intermittent basis
Specific home health agencies may have additional requirements of their own, and you may also need to meet certain qualifications for your insurance plan. Be sure to familiarize yourself with these requirements before applying for home health care.
How to Pay for Home Health Care
Patients and their families can save considerably by choosing home health care over long-term hospitalization or a skilled nursing facility. Still, medical care is expensive. When it comes to paying for home health care, there are several options:
- Self-pay
- Public third-party pay
- Private third-party pay
At Keystone Health, we accept Medicare along with other private insurance plans and self-pay options.
What Medicare Prescription Drug Plans Cover
Each Medicare prescription drug plan, whether it is a stand-alone plan or a Medicare Advantage Prescription Drug plan, has a list of prescription drugs that it covers. This list is called a formulary, or drug list. Plans may cover both generic and brand-name prescription drugs. Most prescription drugs used by Medicare beneficiaries will be on a planâs drug list. To find out which drugs a plan covers, contact the plan or visit the planâs website.
Medicare drug plans may have rules about prior authorization, quantity limits, and step therapy:
- Prior authorization means that the beneficiary and/or the doctor must contact the plan before certain prescriptions can be filled. The doctor may need to show that the drug is medically necessary for it to be covered.
- Quantity limits are limits on how many pills or doses a beneficiary can get at a time.
- Step therapy is a type of prior authorization in which a beneficiary must try one or more similar, lower-cost drugs before the plan will cover the drug the doctor prescribed.
If the doctor believes that one of these coverage rules should be waived, the person can ask for an exception.
Read Also: Does Medicare Provide Dental Care
Medicare’s Home Health Benefit
If you qualify, Medicare will cover your home health care. You are entitled to Medicare coverage of your home health care if you meet the following requirements:
- You are confined to your home .
- Your doctor has ordered home health services for you.
- At least some elements of the services you receive are “skilled” .
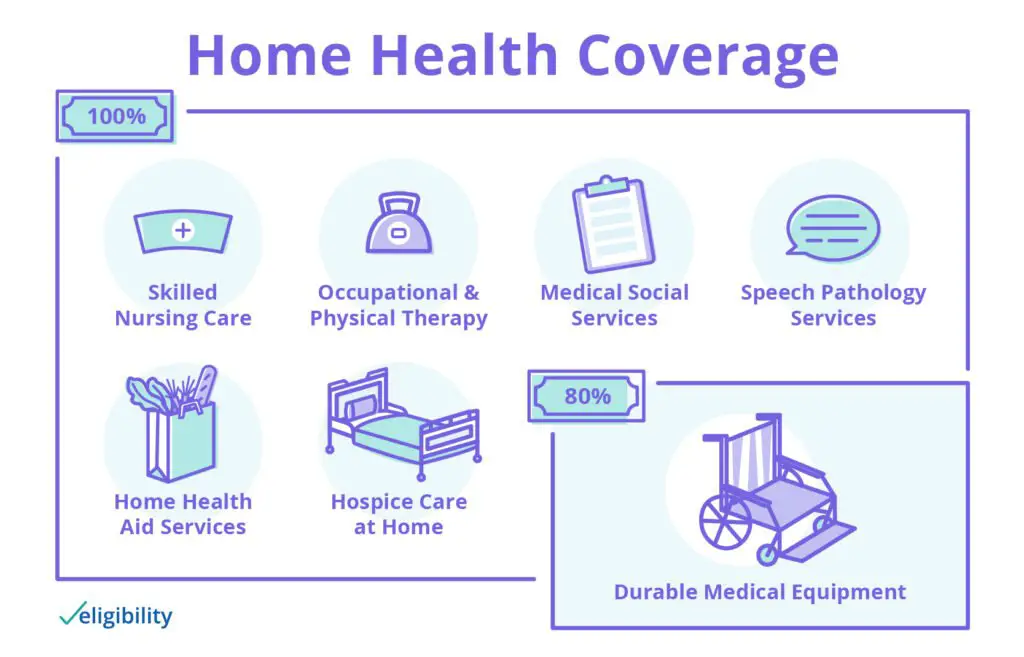
If you need an element of “skilled” care, then you will also be entitled to Medicare coverage of social services, part-time or intermittent home health aide services, and necessary medical supplies and durable medical equipment. You can receive up to 35 hours of services a week, although few beneficiaries actually get this level of service. You are entitled to the same level of services whether you are a member of an HMO or are enrolled in traditional fee-for-service Medicare.
Medicare recipients do not have to pay anything for these services except 20 percent of the cost of medical supplies and equipment, which is covered by some Medigap policies.
Local Elder Law Attorneys in Your City
City, State
Most Medicare beneficiaries are not informed of their appeal rights when given notice that their home health care benefits will be terminated. If your benefits or those of a family member are reduced or terminated, you should take the following steps:
Does Medicare Cover Home Health Care
Recovery at home can be more comfortable and less costly than a lengthy hospital stay. Home health care can be a good solution for those patients who need care for recovery after an injury, monitoring after a serious illness or health complication, or medical care for other acute health issues. Medicare recipients may get help paying for home health care if you meet specific criteria.
What is Home Health Care?
Home health care covers a wide range of treatment options that are performed by medical professionals at home. Care may include injections, tube feedings, condition observation, catheter changing, and wound care. Skilled therapy services are also included in home health care, and these include occupational, speech, and physical therapy services that are necessary to treat your specific illness or injury. Occupational therapy aims to increase daily functionality in regular activities, such as eating or changing clothes. Speech-language pathology can improve language and speech skills, and physical therapy can help you get back on your feet and may include walking, improving mobility, and and increasing strength.
Medical social services may also be covered under your Medicare benefits. These include counseling services and can provide community resources to address social and emotional distresses.
Home Health Care Coverage Options for Medicare Recipients
If you require full-time care, other options besides home health care need to be explored.
Related articles:
Read Also: Does Medicare Pay For Varicose Veins
Medicare Coverage For Home Health Care
Home health care is for someone who needs to receive skilled nursing care or rehab therapy in their own home. Without home health care, some individuals may not get the health care they need.
Medicare may cover the following services and items for those who qualify for the benefit.
- Part-time or intermittent skilled nursing care. Care must be provided by or under the supervision of a professional registered nurse.
- Physical, speech or occupational therapy.
- Durable medical equipment and supplies, such as a hospital bed for use at home.
Medicare beneficiaries who receive any part of the home care benefit may also be eligible to receive additional services, including:
- Medical social services, such as counseling or resources to help with the health condition
- A home health aide to help with activities of daily living like bathing and dressing
How Do Medigap Plans Cover Home Health Care
Medigap plans are designed to cover the 20% coinsurance left over after Medicare pays 80% of approved charges. But because Medicare covers home health care in full, there is no coinsurance to file with a Medigap plan.
However, if you need durable medical equipment such as a wheelchair or walker while receiving home care, those charges are billed separately and subject to the Medicare Part B deductible and coinsurance. If you have Medigap coverage, you pay the deductible and submit the 20% coinsurance charges to your Medigap plan for payment. Most Medigap policies cover your cost in full, but benefits vary by plan.
Read Also: Does Medicare Cover Eye Refraction Test
Medicare Advantage May Offer More Comprehensive Coverage
Private insurance companies run Medicare Advantage. Those companies are regulated by Medicare and must provide the same basic level of coverage as Original Medicare. However, they also offer additional coverage known as supplemental health care benefits.
These benefits can be used to cover the cost of health care or medical equipment that could reduce the risk of injury, reduce the impact of lost mobility or injury or help a person maintain their health and independence.
Medicare Advantage covers many services that are excluded from original Medicare. Individual insurers are permitted to exercise discretion when deciding what services to offer under supplemental benefits, so Medicare Advantage customers should contact their insurers to discuss their options before deciding on a care plan.
