What Medical Equipment And Supplies Does Medicare Cover
En español | Medicare Part B helps to pay for many items of medical equipment and supplies that help you function for example, wheelchairs, artificial limbs, pacemakers, commode chairs, hospital beds, appliances to help breathing, neck and back braces, oxygen supplies and many more. The equipment must be durable . With only a few exceptions, Medicare doesnt cover disposable items.
To qualify for Medicare coverage, the equipment or supplies must be:
- Medically necessary for you not just convenient
- Prescribed by a doctor, a nurse practitioner or another primary care professional
- Not easily used by anyone who isnt ill or injured
- Reusable and likely to last for three years or more
- Appropriate for use within the home
- Provided by suppliers that Medicare has approved
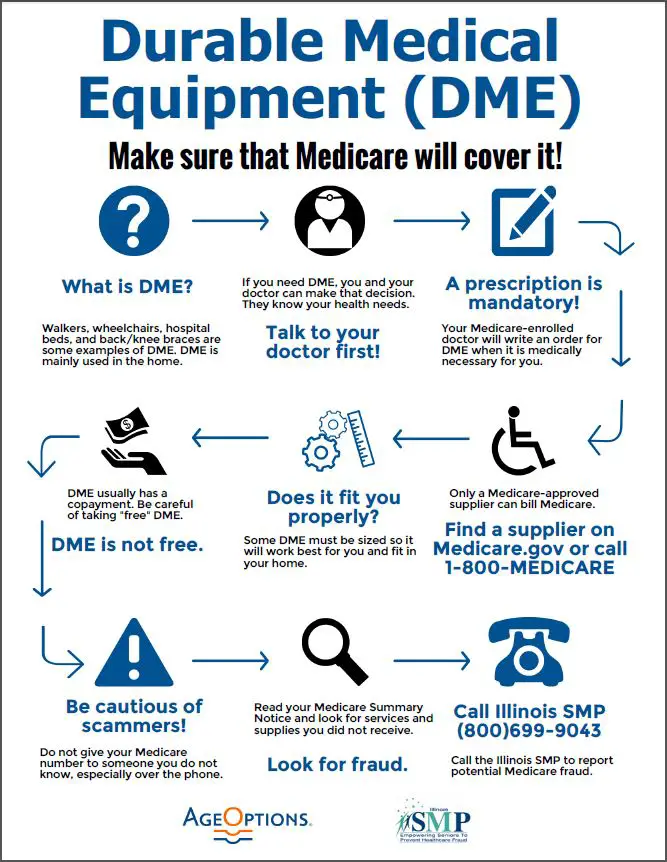
For some items such as oxygen equipment or a seat lift to help you get into and out of a chair Medicare requires a doctor to fill out and sign a certificate of medical necessity without it, Medicare will deny coverage.
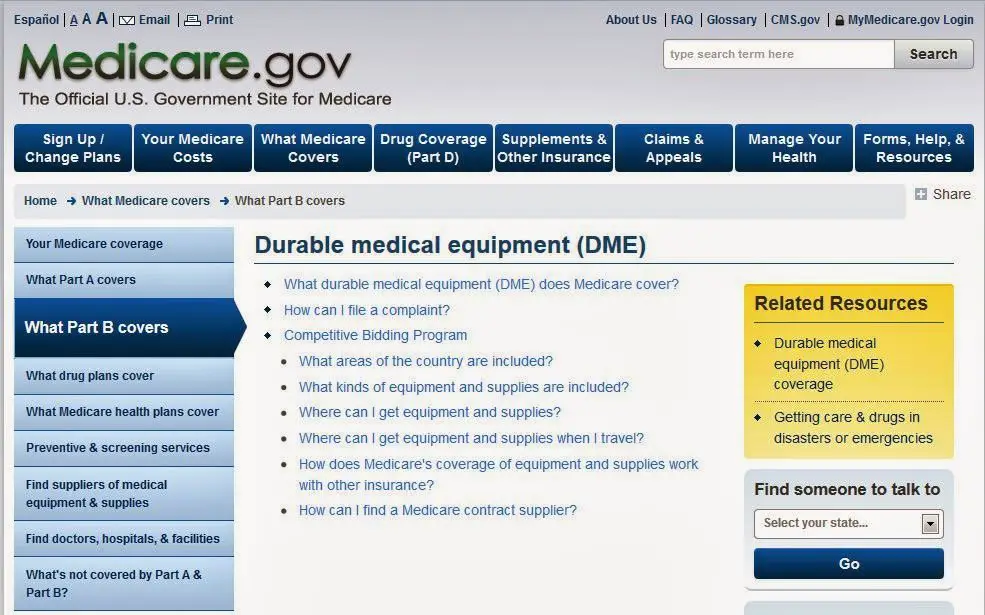
Medical equipment is most often rented, but some items may be purchased. Either way, you must get it from a Medicare-approved supplier. To find approved suppliers in your area, go to the supplier directory on Medicares website at .
For more information, and to find out how to select an approved supplier, see the official publication Medicare Coverage of Durable Medical Equipment and Other Devices.
Equipment Mainly Intended For Use Outside The Home
Medicare Part B covers for durable medical equipment that patients can use around the house. So, if you can walk on your own for short distances within your home, Medicare will not cover for equipment that you only need outside the home, such as
- Motorized scooter
- Motorized wheelchair
Unless you are unable to walk or operate a manual wheelchair, a motorized scooter or wheelchair would be very difficult to get approved. You can only qualify for a motorized wheelchair or scooter if you have upper extremity paralysis or weakness as a result of serious conditions, such as stroke, multiple sclerosis, etc.
Where Can I Find Medicare Durable Medical Equipment
Durable medical equipment can typically be obtained from three different types of providers, and each may carry a different cost for the same item.
Be sure to check with your doctor and your DME supplier to find out how much your equipment may cost.
- Participating providersA participating provider accepts the Medicare-approved amount as full payment for their equipment. The Medicare-approved amount is the amount of money that Medicare has determined it will pay for particular services and items.
- Non-participating providersA non-participating provider accepts Medicare patients, but does not accept the Medicare-approved amount as full payment. Non-participating providers reserve the right to charge you up to 15 percent more than the Medicare-approved amount for their durable medical equipment, which becomes your responsibility to pay. This extra charge is known as a Medicare Part B excess charge.
- Opt-out providersAn opt-out provider has elected to opt out of Medicare entirely and does not accept Medicare insurance as payment. Medicare beneficiaries may still receive care from these providers but will not be able to pay for any services or items using their Medicare coverage.
You can enter your ZIP code and search the Medicare.gov Supplier Directory to find DME suppliers near you.
Don’t Miss: Does Medicare Part C Cover
What Is Medicare Coverage For Durable Medical Equipment
What is Medicare Coverage for Durable Medical Equipment ? Whether you use a walker, a blood pressure monitor, crutches or other items that are used to improve your health, theres no doubt that having access to medical equipment can improve your quality of life and maybe even save it.
Medicare Benefits Solutions
3 people found this article useful
Medicare benefits may cover medical equipment purchases and rentals, depending on your circumstances and the type of equipment you need. If you are eligible for Medicare and are wondering how it will help pay for medical equipment or supplies, youre not alone. Millions of Americans rely on Medicare to help pay for durable medical equipment.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
The classification of DME extends to DMEPOS, or durable medical equipment, prosthetics, orthotics and supplies. Items in this classification include prosthetics such as artificial limbs or other body parts, along with things like braces and wound dressings.
You May Like: How Do I Apply For Medicare In Ohio
What Is Upgraded Equipment And How Does One Purchase It With Medicare
Sometimes suppliers will reduce the cost of upgraded equipment in order to make a sale.
Typically, when Medicare approves an item of durable medical equipment, they will approve only the most basic item available. For example, Medicare may approve the purchase of a walker, but not one with wheels and a hand brake this would be considered upgraded equipment.
It is possible that an upgrade is medically necessary, and if so, Medicare will pay for its part of the upgrade cost. Ones prescription must state specifically the medical reason for why an upgrade is necessary. For example, the individual does not have the physical strength or balance required to lift a standard walker, and therefore, one with wheels is required.
How Much Does Oxygen Equipment Cost
Medicare Part B covers oxygen equipment rental instead of an outright purchase. You must first meet the Part B deductible before Medicare begins paying its share. In 2022, the Medicare Part B deductible is $233.
Once you meet your annual deductible, you pay the standard Part B coinsurance of 20 percent of the Medicare-approved amount, with Medicare covering the remaining 80 percent.
The cost to rent oxygen equipment varies widely depending on the type of equipment, supplier, tank size, and more. On average, though, you can expect to pay around $140 per week for an oxygen concentrator rental if you don’t have health insurance.
That price rises considerably when you add in the portability factor. Renting a portable oxygen concentrator costs around $210 per week on average.
For either option, Medicare pays their 80 percent, leaving you owing between $30 and $40 per week, on average, for oxygen equipment rental.
These calculations assume that the Medicare-approved amount is about the same as the market price for oxygen equipment rental. However, Medicare typically contracts a much lower rate than the going market price. You’ll need to call medical equipment suppliers in your area to get a better idea of what your cost would be.
Recommended Reading: Will Medicare Pay For An Inversion Table
What Medical Supplies Are Covered By Medicare
Medicare covers durable medical equipment as well as supplies that go along with it. For example, when you get a blood sugar meter , you also need test strips and lancets as supplies to use the glucometer. Medicare will usually cover these supplies as DME.
Other examples of supplies that Medicare considers as DME include supplies for infusion pumps, such as tubing, and nebulizer medications that go along with a nebulizer used to treat breathing problems.
Are you eligible for cost-saving Medicare subsidies?
How Do I Order Medical Supplies From Medicare
You can get Medicare-approved DME in several ways: from your doctor, in-person at a supplier, or online.
First, your doctor may supply it, such as a knee or ankle brace they keep on-site. Second, your doctor may give you a list of Medicare suppliers in your area. Third, you can obtain a list of Medicare-approved suppliers from Medicares website. Medicare has a page called Find medical equipment & suppliers. There, you provide your zip code and a brief description of what equipment type you need. The search tool may ask further questions, such as if you need the item custom-fitted before giving you a list of suppliers.
Once you find a supplier, you can contact them to find out pricing information. Youll usually need your doctors prescription to get the most accurate estimate. If you need or want a particular brand or model of DME, your doctor must specify this in the prescription.
Read Also: Does Medicare Cover Vision Insurance
What Is Durable Medical Equipment
Medicare defines Durable Medical Equipment as
Durable Medical Equipment is reusable medical equipment like, walkers, wheelchairs, or hospital beds
Medicare Part B will not, in general, cover medical supplies which are usually disposable and not reusable there are exceptions to this where the supplies are used in combination with DME which are covered.
Recent Developments Highlight The Importance Of Medical Necessity Documentation
The U.S. Supreme Court recently denied review in a case, reaffirming the long-standing Medicare principle that suppliers must be able to demonstrate the medical necessity of durable medical equipment , such as power wheelchairs and scooters, provided to beneficiaries to receive payment. The Supreme Courts action ended decade-long Medicare payment dispute. Coincidentally, on the same day, the Centers for Medicare & Medicaid Services announced that it was enhanc program integrity efforts to fight fraud, waste and abuse in Medicare..
CMS Acting Administrator Kerry Weems told attendees at an American Health Lawyers Association conference that the agency was going to zero in on Medicare fraud involving the highest paid DME suppliers and the highest billed equipment and supplies, including power wheelchairs..
The combination of these two events underscores the importance of securing and retaining documentation of medical necessity for those involved in furnishing DME and submiting claims for Medicare payment. This article discusses these issues further.
Read Also: What Age Does Medicare Eligibility Start
What Are The Costs
Costs of DME depend on a few different factors like the type of plan you have , whether youd like to buy or rent, whether you use Medicare-approved providers, and even where you live.
Medicare requires you to purchase all DME supplies from providers that accept assignment. Those who agree to accept assignment have signed agreements that theyll accept the rates set by Medicare. This keeps costs low both for you and for Medicare.
If you buy or rent supplies from a non-participating provider, you may have to pay a higher amount that Medicare will not reimburse. Avoid using non-approved suppliers except under certain special circumstances, such as an emergency. Always check with a supplier that they accept assignment first.
How Much Does Medicare Cover For Durable Medical Equipment
Under Original Medicare, Medicare covers 80 percent of the cost, so you need to pay 20 percent of the Medicare-approved amount. The Part B deductible also applies. Just make sure that the doctor prescribing the equipment and the supplier are both enrolled in Medicare. If not, Medicare won’t pay the claims.
Medicare also covers DME in different ways. Depending on what equipment you need, Medicare might say that you need to rent the equipment, that you need to buy the equipment, or that you can choose whether to rent or to buy the equipment.
Recommended Reading: When Is Someone Medicare Eligible
How Do You Get Durable Medical Equipment Covered By Medicare
You must get your DME from a Medicare-approved supplier. Both Original Medicare and Medicare Advantage plans have approved lists of suppliers. To find them in your area, go to the supplier directory at www.medicare.gov/supplierdirectory/search.html. You will need to use suppliers that are approved by your plan either original Medicare or Medicare Advantage.Medigap plans will also cover DME if Medicare approves it. It will be covered as a normal Part B charge the Medicare Part B deductible will apply if you have a Medigap plan that does not cover the deductible. But after that Medicare and the Medigap plan should cover your costs in full for covered equipment.
Will Medicare Pay For A Portable Oxygen Concentrator For Air Travel
No, because this is not a use associated with your home. You will have to make alternative arrangements.
For more information on the durable medical equipment that is covered by Medicare, please give us a call today. If you are shopping for rates in your area, you can request a no-obligation quote so you can compare the rates side by side with the top carriers.
You May Like: What Is The Medicare Supplement Plan
Coverage For Disposable Medical Supplies
In most cases, Medicare does not cover disposable medical supplies that are used once and then thrown away. However, some can be covered, such as supplies like test strips for diabetes. Youll want to check with Medicare or your Medicare plan provider directly to see if the item you need is covered. Sometimes it may be that Part D provides coverage. For example, some diabetes supplies are also covered under Part D.
*Note: If you qualify for Medicare home health, Medicare may cover certain disposable supplies, such as intravenous supplies, gauze or catheters.
Dme Not Covered By Medicare
Original Medicare does not cover any durable medical equipment that does not meet strict criteria set by the U.S. Centers for Medicare & Medicaid Services.
5 Medicare Criteria for Durable Medical Equipment
- Must be deemed medically necessary by a doctor or other qualified health care provider
- Should have a usable life of at least three years
- Must be durable able to withstand repeated use
- Should not be useful to someone who is not sick or injured
- Must be used in your home
For example, a powered wheelchair or scooter you need only outside your home is not covered by Original Medicare. But if your doctor determines that it is medically necessary that you have one to get around your home, Medicare will cover it.
Typical DME that Medicare will cover includes hospital beds, wheelchairs, walkers and home oxygen equipment.
Medicare will not cover any disposable supplies unless the supplies are used in conjunction with recognized durable medical equipment that is used inside the home. For example, Medicare will cover diabetes test strips , but not supplies like adult diapers.
Read Also: Does Medicare Pay For Insulin Pumps
Durable Medical Equipment Items Medicare Covers
While the list below is not complete, and other items may be covered, the below are some examples of common durable medical equipment items often covered by Medicare Part B.
Some examples of Durable Medical Equipment Covered by Medicare:
- Wheelchairs
This is not a complete list, and some equipment items are subject to specific conditions for coverage. To see more, .
Medicare does also cover certain prescriptions, medications and supplies that you may use with your durable medical equipment item.
If you are uncertain whether you may be covered by Part B for an item on this list, its best to reach out to your plan provider. If you dont see an item you need on this list, talk with your doctor or health care provider to see if its considered medically necessary and then with your plan provider to see if youll qualify for Medicare to cover it. Medicaid may offer coverage for some things Medicare may not, so keep that in mind if you have Medicaid as well.
How To Rent Equipment
In most cases, DME equipment is rented, not purchased, unless it is made specifically for you. The process for eligibility is the same as for buying DME. After visiting the doctor to get an order, you can take the prescription for DME to an approved supplier to rent the equipment.
Keep in mind that Medicare Advantage plans may have specific rental requirements, like using an in-network supplier or renting a specific device brand or manufacturer. You can check with your plan to find out what the specific rules are for coverage.
Also Check: What Does Medicare Do For You
What Is Dme Medicare
Durable medical equipment or DME is the equipment you need to use in your home to support your health and keep you safe. Examples of DME include walkers, oxygen, blood sugar monitors, patient lifts, sleep apnea devices, and more. Medicare has a long list of DME it will cover, but you have to go through a Medicare-approved provider and supply manufacturer to make sure Medicare will reimburse you.
As a general rule, Medicare DME must meet the following criteria:
- Durable
- Not useful to a person who isnt injured or has a chronic medical condition
- Will usually last at least three years
Medicare Part B pays for DME.
Find a local Medicare plan that fits your needs
Medicares Basic Criteria For Dme
Durable medical equipment to be covered by Medicare Part B has to meet these following basic criteria
- durable
- used for a medical reason, as opposed to for comfort
- not usually useful to someone who isnt sick or injured
- used in your home
- has an expected lifetime of at least 3 years
If the equipment you are looking at doesnt meet these criteria, it will be hard to get it covered by Medicare.
Equipment which Medicare considers to be not primarily medical in nature, or for convenience will not be covered.
These would be items such as
- bed wedges
- shower chairs
Now, you may have a piece of durable medical equipment which qualifies and is typically covered by Medicare, but you still have to qualify as well !
Medicare Part B, will cover DME only if
- it has been prescribed as medically necessary by a Medicare-enrolled Physician or treating provider
- certain DME may demand extra documentation of the medical necessity of the equipment. Source :
- the equipment must be purchased or rented, through a Medicare-enrolled supplier to qualify for coverage
Medical equipment used in skilled nursing facilities, including DME for short term stays, is covered by Original Medicare Part A .
Recommended Reading: How Will Bernie Sanders Pay For Medicare For All
Equipment That Is Not Suitable For Use In The Home
Medicare Part B does not cover for Durable Medical Equipment that is not suitable for use in the home. This includes some types of equipment used in skilled nursing facilities or hospitals, such as:
- Oscillating beds
- Telephone arms
- Standing table
Since these types of DME are not covered by Medicare, you may have to buy or rent them out of pocket.
