How To Apply / Learn More
While this program is available statewide across Ohio, there is a cap on the number of available participants. Approximately 33,000 individuals are provided services simultaneously. However, even at that capacity, the state may run out of slots for qualified persons. Applicants placed on a waiting list will have to wait for a space to open when someone leaves the program.
Ohio residents should contact their local area agency on aging to apply or call the Department of Aging at 1-866-243-5678. The program webpage provides additional details about this waiver.
Ohio residents may also want to consider the Ohio Medicaid supported Assisted Living Waiver.
Member Outreach And Education
In addition to the enrollment packet, all families with an active telephone number receive up to 3 telephone attempts to verbally explain Montana Healthcare Programs benefits and the Passport program, answer questions, and take enrollment information over the telephone.
An education script is followed during these outreach calls to ensure that all members receive the same information about Montana Healthcare Programs/HMK Plus and Passport. Members have additional resources to help them use their Montana Healthcare Programs/HMK Plus services and understand the Passport to Health program.
Member Education Resources
Resource: Member Montana Healthcare Programs/HMK Plus Handbook
Description: All eligible Montana Healthcare Programs/HMK Plus members are sent a postcard informing them how to find the member handbook online or how to request a paper copy. This handbook, which includes a section on the Passport program, is an excellent resource for members enrolled in Montana Healthcare Programs/HMK Plus.
Where to Find:
- Eligible for a non-Montana Healthcare Programs plan.
- Receiving Montana Healthcare Programs under a presumptive eligibility program.
Members Exempt from Passport The Department has determined members who are eligible to participate in the Passport program may request an exempt status for the following reasons:
End of Member Enrollment and Education Chapter
Billing Montana Healthcare Programs/hmk Plus Members
To bill a Montana Healthcare Programs/HMK Plus member, an agreement must be signed by the member in advance of services. There are two types of member agreements:
- Private-pay agreements. State the member is not being accepted as a Montana Healthcare Programs member and will be responsible to pay for the services received.
- Custom agreements. Include specific dates of services, actual services or procedures, and the cost to the member, and states the services will not be covered by Montana Healthcare Programs and the member will be responsible to pay for the services received.
Providers may not bill a member when the provider has informed the member that Montana Healthcare Programs may not pay or when the agreement is contained in a form that provider routinely requires members to sign. Members may be billed for:
- Non-covered services.
- Covered but medically unnecessary services, including services that Montana Healthcare Programs has denied payment for lack of medical necessity.
- When provider is unable to get the Passport referral from the Passport PCP.
- Services received when the provider does not accept the member as a Montana Healthcare Programs member.
- Copayments.
Providers are required to accept the amount paid by Montana Healthcare Programs as payment in full. Unless an agreement is signed, members may not be billed for:
A provider who bills Montana Healthcare Programs for services will be deemed to have accepted the member as Montana Healthcare Programs.
Read Also: Do I Qualify For Medicare If I Am Disabled
Member Case Management Fee
In addition to fee-for-service reimbursement, Passport providers receive a case management fee, or an enhanced fee totaling $6 per member per month for each enrolled Team Care member.
This fee is in a separate payment from the fee-for-service reimbursement and is paid regardless of whether the member is seen during the month. The monthly case management fee is paid with the expectation that the items listed in the provider requirements of this manual are completed as needed for members coordination of care. The monthly case management fee is paid to providers by their Passport number. The fees are listed with procedure code for each Passport enrollee on the providers remittance advice. The date of service for the code is shown as the first of the month for which the fee is being paid.
Tribal Health Improvement Program
The Tribal Health Improvement Program is a historic partnership between the Tribal, State and Federal governments to address factors that contribute to health disparities in the American Indian population eligible for Montana Healthcare Programs and residing on a reservation. This manual will give you an overview of the Tribal Health Improvement Program, goals of the program and a link to the forms necessary to complete the documentation required for program participation.
T-HIP services are designed to help members:
- Maximize the benefits of their medical and other support systems
- Improve knowledge of their disease and self-management skills and
- Remove barriers to achieving better health and a better life.
End of Other Passport Programs Chapter
Recommended Reading: Why Sign Up For Medicare At 65
What Information Should I Have Ready For My Assessment
In order for the assessor to determine your eligibility for in-home assistance, you must be willing to provide the following information at the time of assessment:
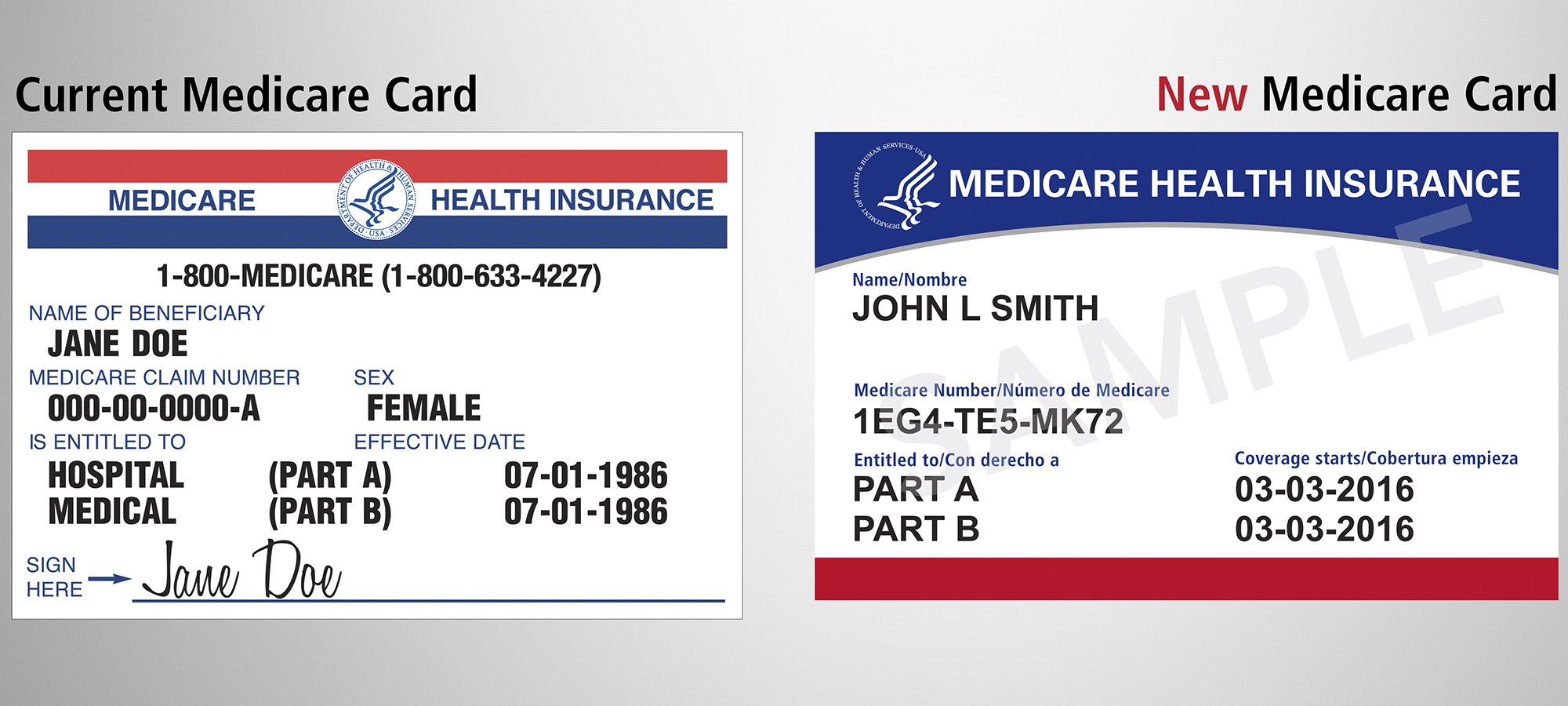
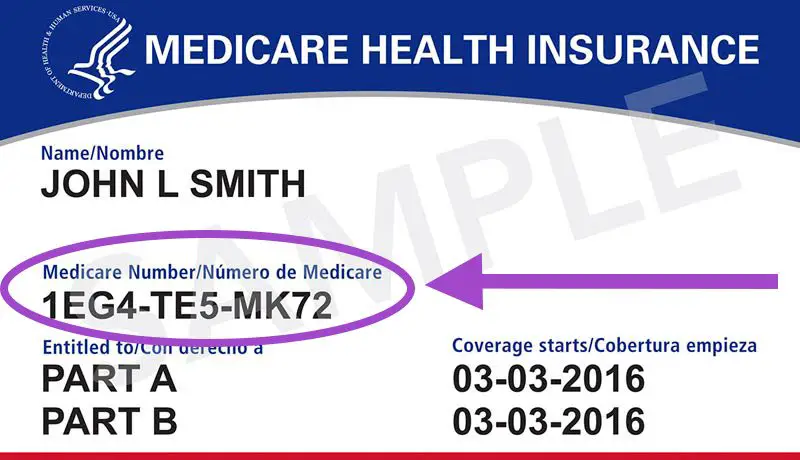
- Social Security card
- Medicare card, if you have one
- Proof of age
- Your doctors names, addresses, and phone numbers
- Your medical problems
- Medicines and treatments you are receiving
- Names of family or friends who help you
- Names of any agencies currently providing help
How Do I Qualify For Passport
The primary criteria for enrollment in PASSPORT are age, level of care, and income.
You must be at least 60 years old.
You need the same level of care as someone in a nursing home extensive help with personal care or requiring 24-hour supervision to prevent harm. Level of care is determined at the initial assessment.
You must qualify for the Medicaid waiver, but do not assume that you will be ineligible if you have been denied traditional Medicaid in the past. The assessor will determine your Medicaid eligibility during the initial home visit.
Read Also: Can You Get Medicare Advantage Without Part B
Does Estate Recovery Apply To Passport
Yes. PASSPORT is a Medicaid program, and under federal and state law, the state may recover money paid for your Medicaid benefits from your estate. The purpose of estate recovery is to allow states to recoup some of the tax dollars invested in Medicaid, in order to reduce the escalating cost of one of the largest and fastest growing government programs.
Molina Healthcare Announces The Closing Of Its Acquisition Of Passports Medicaid Plan Assets
LONG BEACH, Calif.—-Molina Healthcare, Inc. today announced the closing of its acquisition of certain assets related to the Medicaid line of business of Passport Health Plan, Inc. . In addition, Passports Medicaid contract with the Commonwealth of Kentucky has been novated to Molina. Effective September 1, 2020, Molina Healthcare of Kentucky, Inc. will provide Medicaid managed care benefits to Medicaid members that were previously being served by Passport. As of August 1, 2020, Passport served approximately 315,000 Medicaid members in Kentucky.
In addition to the acquisition of Passports Medicaid contract, Molina acquired and will utilize the Passport name, a well-known brand in Kentucky, and has agreed to hire approximately 500 Kentucky-based Passport and Evolent Health employees.
About Molina Healthcare
Molina Healthcare, Inc., a FORTUNE 500 company, provides managed health care services under the Medicaid and Medicare programs and through the state insurance marketplaces. Through its locally operated health plans, Molina Healthcare served approximately 3.6 million members as of June 30, 2020. For more information about Molina Healthcare, please visit molinahealthcare.com.
Also Check: Does Medicare Cover Hospice Expenses
Diagnostic Testing And Referrals
If a screening indicates the need for further diagnostic testing or treatment, those services should be provided without delay. If the service cannot be provided by the Passport provider, a referral must be made.
Montana Healthcare Programs covers all services that are determined to be medically necessary to members under age 21, even if those services are not covered for adults. Examples of additional services for pediatric members include chiropractic treatment, nutrition, private duty nursing, residential treatment, respiratory therapy, school-based services, and substance abuse inmember and day treatment.
End of EPSDT Services Chapter
Passport Advantage Drug Coverage And Formulary
A formulary is divided into tiers or levels of coverage based on the type or usage of your medication or benefit categories, according to drug costs. Each tier will have a defined out-of-pocket cost that you must pay before receiving the drug. You can see complete 2020 Passport Advantage H9870-001 Formulary here.
| Drug Tier |
|---|
Also Check: How Much Do Medicare Supplements Increase Each Year
What Happens At An Assessment
A nurse or social worker visits you in your home to assess your needs and discuss options. You will answer many questions and the assessor will observe your level of independence. The assessor will need to review documentation of income and assets to make a preliminary determination about your eligibility for in-home assistance. If enrolled in one of our home care programs, you will work with the assessor to develop an initial plan of care.
If you qualify for Medicaid but are not currently enrolled, the assessor can assist with completion of the Medicaid application. You must then follow up with the application process through the Department of Job and Family Services.
What Is Passport Health Plan
Passport was established in 1997 as a pilot project for the sole purpose of providing managed care for Medicaid in the Louisville region to help the state with growing healthcare costs.
The latest:Passport Health to suspend work on west Louisville HQ amid Kentucky Medicaid cuts
It was organized by hospitals, doctors and other health providers as a nonprofit entity to handle Medicaid claims and promote wellness in Jefferson and 15 surrounding counties.
For many years, Passport operated as the only Medicaid managed-care organization in Kentucky until the state decided in 2011 to seek other outside, for-profit companies to provide managed care statewide for most of its Medicaid patients.
Also Check: Does Medicare Cover Smoking Cessation Products
Passport To Health Program
Passport to Health is the primary care case management program for the following Montana Healthcare Programs: Standard Montana Healthcare Programs, Healthy Montana Kids Plus, and the HELP Program. The Passport to Health program provides case management related services that include locating, coordinating, and monitoring primary healthcare services. To achieve this, the Passport program works with the states other care coordination programs:
- Nurse First Advice Line
- Team Care
- Tribal Health Improvement Program
Montana Healthcare Programs and HMK Plus members who are eligible for Passport must enroll in the program. See the Member Enrollment and Eligibility Chapter of this manual for a list of members who are ineligible for Passport. Each member has a designated Passport provider such as a physician, mid-level practitioner, or primary care clinic.
The Passport provider delivers PCCM services to their members. This means they provide or coordinate the members care and make referrals to other Montana Healthcare Programs providers when necessary. With some exceptions, all services to Passport members must be provided or approved by the members Passport provider Montana Healthcare Programs will not reimburse for those services. The members Passport provider is also referred to as the primary care provider .
Key Contacts And Websites
Contact hours are 8 a.m. to 5 p.m. MondayFriday, Mountain Standard Time, unless otherwise stated. The phone numbers designated In state will not work outside Montana. The numbers designated TDD and TYY have a telecommunication device for people who need assistance hearing. Persons with disabilities who need an alternative accessible format of this information, or who require some other reasonable accommodation to participate in Montana Healthcare Programs/HMK Plus, should contact DPHHS through the Passport to Health program.
You May Like: What Is The Extra Help Program For Medicare
Disenrolling Passport Or Team Care Members
A provider may disenroll a Passport or Team Care member for the following reasons:
- Providermember relationship is mutually unacceptable.
- Member has not established care.
- Member is seeking primary care elsewhere.
- Member fails to follow prescribed treatment.
- Member is physically or verbally abusive and poses a threat to providers or other members.
- Member could be better treated by a different type of provider, and a referral process is not feasible.
- Member consistently fails to show up for appointments.
A provider cannot disenroll a Passport or Team Care member for the following reasons:
- An adverse change in the enrollees health status.
- Members utilization of medical services.
- Members diminished mental capacity.
- Uncooperative or disruptive behavior as a result of the members special needs. The exception is if enrollment seriously impairs the PCPs ability to furnish care to the member or other members. If this is the case, disenrollment must be approved by the Passport program officer.
- Any reason that may be considered discrimination.
- Failure of Members to pay co-payments owed prior to January 1, 2020 or other bills.Effective for all claims paid on or after January 1, 2020 copayment will not be assessed.
Guidance For Appropriate Care
If a provider sees a member for a routine visit or sees the member frequently and is not that members Passport provider, the provider should talk to the member about the importance of having a medical home.
It is acceptable to deny service if the member is able to see his/her Passport provider. Conversely, the Passport provider is under no obligation to provide a referral if the member is able to see them. Suggest to the member that he/she see their Passport provider every time they are sick or hurt it is also acceptable to suggest that the member changes to your clinic as their Passport provider. To change their provider, the member can call the Montana Healthcare Programs/HMK Plus Member Help Line from your office or have the provider fax a Provider Change Form signed by the member.
Passport referrals and prior authorization are different. For more information, see the Additional Montana Healthcare Programs/HMK Plus Requirements for Passport Members chapter in this manual and Prior Authorization chapters in your provider type manual and the General Information for Providers manual.
Don’t Miss: What Is The Best Medicare Supplement Plan In Arizona
How Big Is Passport
Passport now is one of five private companies that manage health care for most of the 1.4 million Kentuckians covered by Medicaid, an $11.5 billion program that gets most of its money from the federal government.
The other four are commercial health insurance companies that operate in multiple states.
Passport is the second largest of the five, managing health care for about 315,000 Medicaid enrollees, most of them in the Jefferson County region.
Early And Periodic Screening Diagnostic And Treatment Services Program
EPSDT is a benefit package for all HMK Plus members designed to ensure that children receive comprehensive healthcare. The provider is encouraged to actively screen for specific pediatric problems, order diagnostic tests as indicated, and treat problems found, or if necessary, refer members to other providers for treatment.
You May Like: What Information Do I Need To Sign Up For Medicare
Role Of The Passport Provider
A PCP can be a physician or a mid-level practitioner who provides PCCM services by agreement with the Department. The Department allows any provider who has primary care within his/her professional scope of practice to be a PCP. However, the Department does recognize that certain specialties are more likely to practice primary care, and actively recruits these providers.
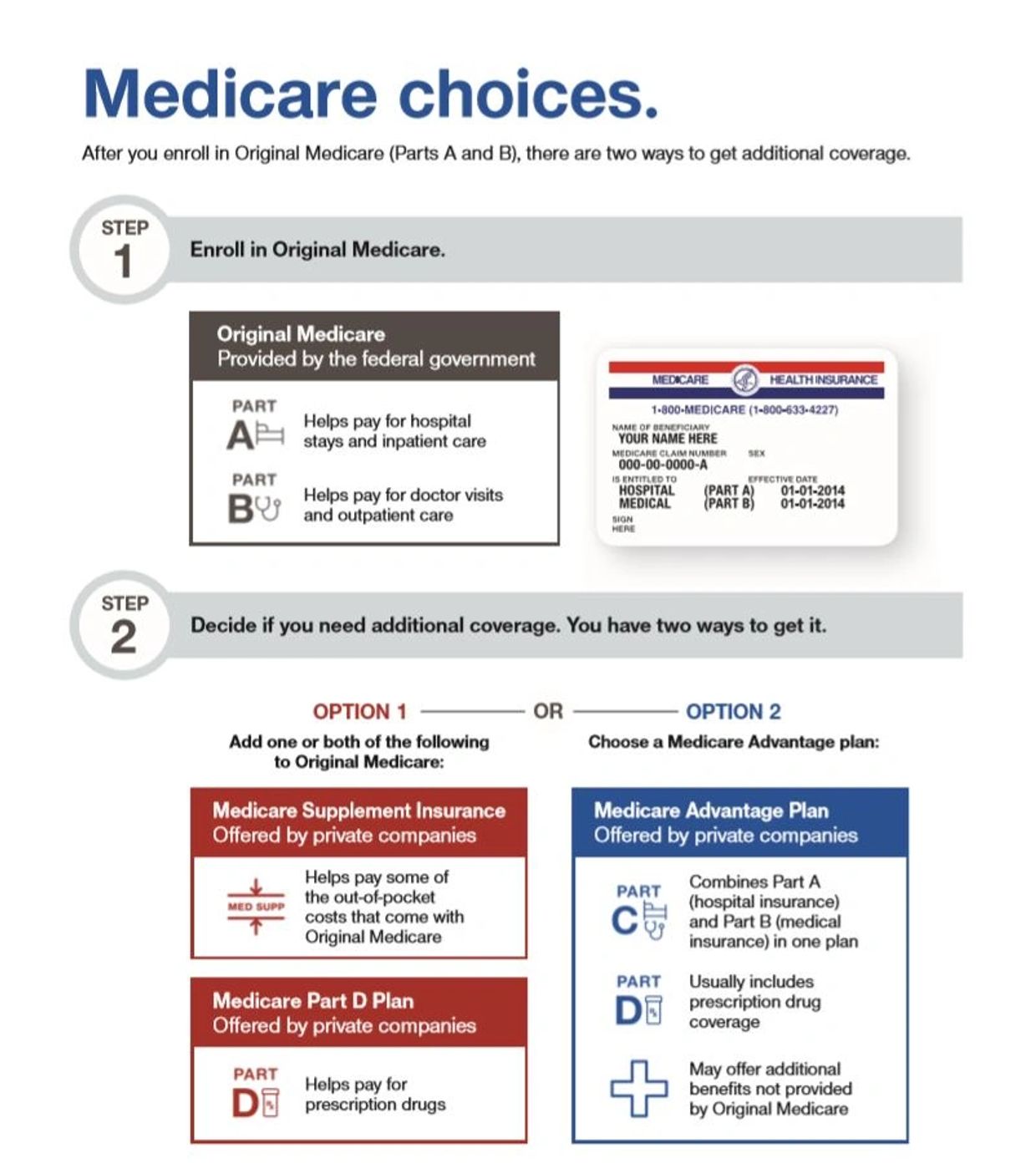
Passport Health Plan Creates New Medicare Advantage Program Called Passport Advantage
Passport Health Plan is proud to announce that it has received full approval from the U.S. Centers for Medicare & Medicaid Services to create and run a Medicare Advantage /Medicare Advantage-Prescription Drug program to offer medical and pharmacy benefits to people who have both Kentucky Medicaid and Medicare benefits.
The program which will be called Passport Advantage will be available to residents of Bullitt, Jefferson, Hardin, and Nelson counties who have both Medicaid and Medicare benefits. This Special Needs Plan for Dual-eligible beneficiaries will allow Passport to provide intensive care coordination and services to a population that often experiences fragmented care.
Passport temporarily exited the Medicare Advantage business at the end of 2011 to focus on our Medicaid product delivery and service. Doing so allowed us to gain record growth while maintaining the highest NCQA ranking for any Medicaid plan in Kentucky, said Passport Health Plan CEO Mark B. Carter. By returning to the Medicare Advantage market with the Passport Advantage product, we will be able to provide improved care and continuity using the same providers for people eligible for Medicaid and Medicare benefits.
Don’t Miss: What Does Medicare Part B Cover
Selecting A Passport Provider
the same Passport provider or everyone can have a different Passport provider based on individual needs. Members are not auto-assigned to a Passport provider unless they have not chosen a provider themselves. Members receive a reminder letter, an outreach call, and are given 45 days to select a provider. After 45 days, Passport to Health automatically assign members to a provider appropriate to the member’s age, sex, and location based on the following criteria :
- Previous Passport enrollment.
- Claims information.Family Passport enrollment.
- Native American members who have declared a tribal enrollment, and who live in a county where there is an Indian Health Service Passport provider.
- Randomly, to a provider in the members geographic area who is accepting new members.
Members who are assigned to a Passport provider are notified at least 10 days in advance of the effective assignment date to allow members to notify Passport to Health if they would like to select a different provider.
Members may change their Passport provider up to once per month but the change will not be effective until the following month at the earliest, depending on the date the choice is made.
