Q Where Do I Go To Apply For Medicaid
A. There are several ways to apply for Medicaid and other medical assistance programs:
- On the internet, you can use ASSIST to check your eligibility for several different assistance programs by completing a self-screening questionnaire. ASSIST then allows you to apply online.
- You may also print an Application for Health Insurance/Medicaid. The application form is also available in Spanish/en Español.
- By phone, you can contact Medicaid Customer Relations at 1-800-372-2022 or 255-9500 to be directed to the Division of Social Services office closest to where you live. DSS staff members will help you find out more about eligibility for Medicaid and other assistance programs. Then the appropriate information and application forms will be mailed to you. Complete, sign and date the application form in ink and mail it to the address provided.
- For Long Term Care applications, please call the Long Term Care Medicaid Unit listed for the county where you live.
Current Law: 16 Weeks Of Federal Additional Income Included In Eligibility
At present, vulnerable workers who become unemployed can receive $600 in additional federal income for 16 weeks. This federal unemployment compensation is included in income eligibility determinations for ACA marketplace eligibility but not for Medicaid and CHIP eligibility.
Eligibility for assistance of any kind is not substantially different between expansion and nonexpansion states when all the cash assistance available is received, the researchers stated.
READ MORE:Medicaid Expansion States May See Lower Uninsurance Amid COVID-19
However, workers in expansion states are seven times more likely to be eligible for Medicaid, the researchers found. This is a critical metric because Medicaid usually has limited additional out-of-pocket healthcare spending for beneficiaries, as opposed to health plans on the ACA federal or state health insurance marketplace. This would make healthcare more affordable for Medicaid-eligible workers in Medicaid expansion states.
In both Medicaid expansion and nonexpansion states, under the current law, a similar percentage of vulnerable workers are not eligible for any federal funding . The percentage is slightly lower in Medicaid expansion states.
Recommended Reading: North Carolina Medicaid Income Guidelines
Newly Eligible Missourians Can Now Apply For Medicaid
Newly eligible Missourians can now apply for Medicaid health benefits by applying online, or by phone 373-9994.
Adults under the age of 65 with household incomes up to 138% of the federal poverty level are now eligible for Missouri Medicaid. In 2021, this amounts to about $17,774 for an individual or $24,039 for a household of two. Unsure if youre eligible? Use the Medicaid Eligibility Calculator to find out.
The Missouri Department of Social Services began processing newly eligible adult applications on October 1, 2021.
Pregnant women and children were already eligible for Medicaid or CHIP at higher income levels. In addition, low-income residents who are blind or have disabilities are also eligible but must meet strict asset limits to qualify. Please visit the MO HealthNet website for more eligibility information.
Read Also: Who Qualifies For Medicare Part C
What Other Restrictions Apply
Medicare only pays the additional amount for administering the COVID-19 vaccine in the home if the sole purpose of the visit is to administer a COVID-19 vaccine. Medicare doesnt pay the additional amount if you provide another Medicare service in the same home on the same date. In those situations, Medicare pays for administering the COVID-19 vaccine at the standard amount .
If you administer the COVID-19 vaccine to more than 1 Medicare patient in a single home in the same multi-unit or communal living arrangement on the same day, Medicare pays:
- Approximately $40 to administer each dose of the COVID-19 vaccine, including additional doses and booster doses
- For dates of service between June 8, 2021 and August 24, 2021, Medicare pays the additional payment amount of approximately $35 only once per date of service in that home regardless of how many Medicare patients receive the vaccine
- Effective on August 24, 2021, Medicare pays the additional payment amount , for up to a maximum of 5 vaccine administration services per home unit or communal space within a single group living location but only when fewer than 10 Medicare patients receive a COVID-19 vaccine dose on the same day at the same group living location. When 10 or more Medicare patients receive a COVID-19 vaccine dose at a group living location on the same day, the additional payment can only be billed once per home .
People Who Have Both Medicare & Medicaid
People who have both Medicare and full Medicaid coverage are dually eligible. Medicare pays first when youre a dual eligible and you get Medicare-covered services. Medicaid pays last, after Medicare and any other health insurance you have.
You can still pick how you want to get your Medicare coverage: Original Medicare or Medicare Advantage . Check your Medicare coverage options.
If you choose to join a Medicare Advantage Plan, there are special plans for dual eligibles that make it easier for you to get the services you need, include Medicare coverage , and may also cost less, like:
- Special Needs Plans
- Medicare-Medicaid Plans
- Program of All-Inclusive Care for the Elderly plans can help certain people get care outside of a nursing home
Don’t Miss: Does Medicare Cover Prescription Costs
Q How Do I Join A Managed Care Organization
A. After being notified that you are eligible for Medicaid , you will receive in the mail a packet of information about the different MCO plan options for receiving your Medicaid benefits. You may choose any plan described in this mailing. You probably want to choose a Managed Care Organization to which your doctor belongs. If you need help making this decision, call the Health Benefit Manager at the phone number in the mailing.
Additional Payment For Administering The Vaccine In The Patients Home
View the infographic ) ) for COVID-19 vaccine administration in the home.
Effective June 8, 2021, Medicares additional payment amount for administering the COVID-19 vaccine in the home for certain Medicare patients is approximately $35 per dose. This payment also applies when you administer any of the additional or booster doses listed in the Medicare Payment Rates table.
Medicare will pay approximately $35 in addition to the standard administration amount , for a total payment of approximately $75 for a vaccine dose administered in a patient’s home. We also geographically adjust the additional amount and administration rate based on where you administer the vaccine.
We established this payment amount of approximately $35 on a preliminary basis to ensure access to COVID-19 vaccines during the PHE. We continue to evaluate the needs of Medicare patients and these policies, and we’ll address them in the future, as needed.
Read Also: How Is Medicare Part B Financed
Can You Have A Medicare Advantage Plan And Medicaid At The Same Time
Medicare Advantage plans are Medicare plans offered by private insurers, while Medicaid provides health coverage for low-income eligible Americans. In some cases, you can have both at the same time if you qualify for dual eligibility.
What you should know
| 1. Medicare Advantage is a private Medicare plan, also referred to as Medicare Part C or MA plans. | 2. Medicaid is offered to those who meet low-income eligibility and covers additional health services that are not covered by Medicare. |
| 3.Dual eligibles can have both Medicare Advantage and Medicaid at the same time. | 4. Private healthcare providers offer specialized plans for dual eligibles that can coordinate Medicaid benefits with a Medicare Advantage plan. |
For those who meet income eligibility, Medicaid can be an important resource for covering healthcare expenses that Medicare does not. In addition, some people can benefit from having both Medicaid and Medicare Advantage, which is Medicare coverage through private insurance companies. Those who qualify are known as dual eligibles. Learn more about how it works.
What Are Dual Health Plans
Dual health plans are designed just for people who have both Medicaid and Medicare. Theyre a special type of Medicare Part C plan. Dual health plans combine hospital, medical and prescription drug coverage. Youll keep all your Medicaid benefits. Plus, you could get more benefits than with Original Medicare. And you could get it all with as low as a $0 plan premium.
View the “Do I Lose My Medicaid Benefits?” article.
Read Also: Do Teachers Get Medicare When They Retire
What Is The Medicaid Income Limit In My State
Most states use a standard of 138% of the federal poverty level as a basis for Medicaid eligibility. But each state is free to set its own limits.
The table below shows the income limit as a percentage of the FPL required for Medicaid eligibility in each state for two-parent households and for individuals adults.
If 0% appears, that means individuals may not qualify for Medicaid in that state based on income alone and must meet other criteria, such as being pregnant or disabled.
Medicaid Income Limit by State|
State |
|
|---|---|
| 52% | 0% |
FPL is used to determine eligibility for Medicaid, certain welfare benefits and other assistance programs. The FPL is computed by the U.S. Census Bureau and can be adjusted every year based on inflation.
Medicaid uses a percentage of the FPL to determine its income limits for eligibility. For example, you may qualify for Medicaid if you earn less than 133% of the federal poverty level. Or you may qualify if you earn less than 150% of the federal poverty level and are disabled. Again, each state sets its own income limits to determine Medicaid eligibility.
Contact your state Medicaid program for more eligibility information, as most states offer different types of Medicaid programs that may each have their own income limits and other qualifying criteria. Even if you make more than the standard limit found below, there may be additional programs for which you still qualify.
District Of Columbia Medicaid
Eligibility overview: Washington, D.C., has one of the most generous Medicaid programs in the U.S., covering adults with household incomes up to 215% of the FPL as part of its expansion program. It also has programs for pregnant, parent/caretaker, elderly, disabled and child residents.
Income requirements: The expansion covers adults without dependents who make up to $2,082 a month when applying on their own. Elderly, blind or disabled D.C. residents are eligible if they make up to 100% of the FPL, or $1,073.33 per month for one individual, and have resources below $4,000 for one person. D.C. also covers pregnant women with incomes up to 319% of the FPL, or $4,703.40 monthly for a two-person household, and parents/caretakers with incomes up to 216% of the FPL.
How to apply for Washington, D.C. Medicaid: You can apply online at DC Health Link or by visiting your closest Income Maintenance Administration Service Center.
Other notable programs: Long-term care and nursing home care services Spend Down, a Medicaid program for people who exceed income limits, but have high medical bills Emergency Medicaid for people who canât qualify for standard Medicaid due to citizenship/immigration status.
Read Also: Does Md Anderson Cancer Center Accept Medicare
What Is The Highest Income To Qualify For Medicaid
Washington D.C. has the highest allowable income to qualify for Medicaid, at 215% of the FPL for individuals and 221% for a family of three.
That means an individual in Washington D.C. can make up to $27,692 per year and still be eligible for Medicaid. Washington D.C.s high cost of living factors into its higher income limit for Medicaid. No other state uses more than the standard 138% limit for individuals.
A family of three can make up to $48,531.60 and still qualify for Medicaid in Washington D.C. Connecticut is the only other state to use a limit higher than 138%.
Learn More About Medicare And Medicaid

If you need health insurance now, Medicaid or Medicare may be the solution for you. We can help guide you through the enrollment process, just give us a call at 709-5513. Our agents will walk you through the process of applying for or enrolling in either one of these insurance plans.
Celebrating 17 years of service to our clients, agents, and employees.
You May Like: What Is Cigna Medicare Supplement Plan G
When And Why Was The Federal Poverty Level Established
The federal poverty thresholds were first introduced in 1965, based on the work of the Social Security Administrations Mollie Orshansky. The amounts were tied to the bare minimum amount that people needed in order to have adequate food, with a multiplier used to account for other necessary expenses. Orshansky noted at the time that the poverty thresholds were a measure of the amount of income that would be inadequate for people to live, as opposed to a minimum adequate amount.
Dont Miss: Apply For Montana Medicaid Online
Who Qualifies For Medicare Vs Medicaid
Nearly every American will one day qualify for Medicare, but Medicaid is only for those with a low income. Beneficiaries can enroll in Medicaid through the state program office. If you think you are eligible for Medicaid benefits, contact your state health department to apply. To qualify for Medicaid, your income will need to be below a predetermined amount set by your state government.
If your income is above this amount, but you struggle with high medical costs, you may want to check if a Medicaid spend-down program is available in your state. Medicaid spend-down programs allow beneficiaries who exceed the income requirement to deduct their medical costs from their income to meet the state-appointed income requirement.
To qualify for Medicare, you must meet the below requirements:
Get A Free Quote
Find the most affordable Medicare Plan in your area
Be a U.S. Citizen or documented resident for at least five years AND one of the following:
- Age 65 or above
- Amyotrophic lateral sclerosis diagnosis
- Receiving SSDI benefits for at least 24 months
As you can see, eligibility requirements for the two health insurance programs differ. However, some people fit into the cross-section of qualifications. If you qualify for both, the two health programs work together.
Also Check: How To Sign Up For Medicare Advantage
If Your Income Is Low And Your State Hasnt Expanded Medicaid
If your state hasnt expanded Medicaid, your income is below the federal poverty level, and you dont qualify for Medicaid under your states current rules, you wont qualify for either health insurance savings program: Medicaid coverage or savings on a private health plan bought through the Marketplace.
- Find out why
-
- When the health care law was passed, it required states to provide Medicaid coverage for all adults 18 to 65 with incomes up to 133% of the federal poverty level, regardless of their age, family status, or health.
- The law also provides premium tax credits for people with incomes between 100% and 400% of the federal poverty level to buy private insurance plans in the Health Insurance Marketplace®.
- The U.S. Supreme Court later ruled that the Medicaid expansion is voluntary with states. As a result, some states havent expanded their Medicaid programs.
- Adults in those states with incomes below 100% of the federal poverty level, and who dont qualify for Medicaid based on disability, age, or other factors, fall into a gap.
- Their incomes are too high to qualify for Medicaid in their states.
- Their incomes are below the range the law set for savings on a Marketplace insurance plan.
-
States are continuing to make coverage decisions. They could expand Medicaid in the future.
Recommended Reading: General Doctor That Accepts Medicaid
Can I Select An Insurance Plan For My Medicare And Medicaid Benefits
If you are dual eligible, you are can enroll in a dual eligible special needs plan that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid dont over individually, including over-the-counter items, hearing aids, and vision or dental care.
Beneficiaries who are dual eligible can change between Original Medicare and Medicare Advantage or switch Part D plans at each quarter.
Read more about the Medicaid benefits available to Medicare enrollees.
Josh Schultz has a strong background in Medicare and the Affordable Care Act. He coordinated a Medicare ombudsman contract at the Medicare Rights Center in New York City, and represented clients in extensive Medicare claims and appeals. In addition to advocacy work, Josh helped implement health insurance exchanges at the technology firm hCentive. He also has held consulting roles, including at Sachs Policy Group, where he worked with insurer, hospital and technology clients.
Don’t Miss: When Do You Receive Medicare Card
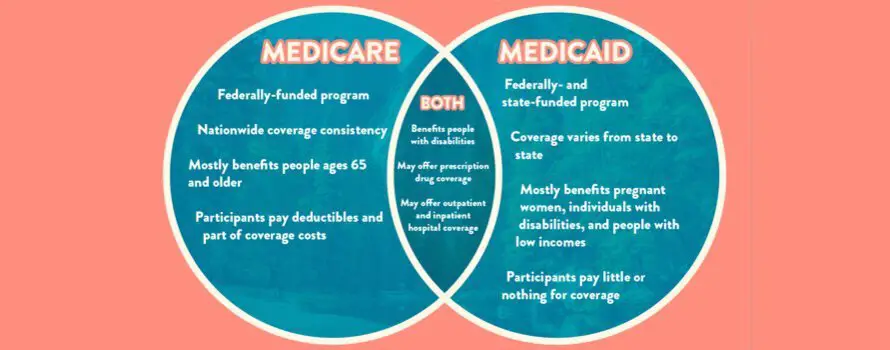
What Is Medicare Vs Medicaid
Medicare and Medicaid are not the same. Many confuse the benefits of Medicare vs. Medicaid as they are both government-run health insurance programs in the United States. However, Medicare is federal, and Medicaid differs by state.
Medicare benefits are the same across all states and U.S. territories. Typically, Medicare benefits are available to those 65 and over or receiving Social Security Disability benefits under 65. Medicare offers standardized premiums that are consistent for those in the same income bracket.
On the other hand, each states government operates Medicaid. Every state has different qualifications and requirements for enrollment in Medicaid. While there is no age requirement for Medicaid, there is a financial requirement. Your income and resources may not exceed state-specific thresholds to be eligible for Medicaid coverage. Medicaid coverage typically comes at no cost to the beneficiary.
Get A Free Quote
Find the most affordable Medicare Plan in your area
To differentiate the two, with Medi-care, think of care for those 65 and over or those with disabilities. Then, Medic-aid is an aid to those with a low income.
Medicaid Spend Down: How To Qualify For Medicaid If You Make Too Much Money
The Medicaid Spend Down is an often overlooked way to qualify for Medicaid when you make too much money and dont otherwise qualify.
The reason you might want to do a Medicaid Spend Down is if you are needing medical care services like long-term nursing care or a home caregiver the Medicaid program will pay for some of these costs.
In this article, I will explain the basics of the Medicaid Spend Down and tell you about a special type of lawyer who can help you to through this process so that you qualify for Medicaid.
Lets first start with what is the Medicaid Spend Down.
Recommended Reading: When Can You Apply For Part B Medicare
