Medicare Resources For Mental Health
If you need information or help with mental health concerns, there are resources for you. The Medicare.gov website has an easy search feature, and you can find information about any Medicare-related topic, with links to other sources.
- in case of an emergency or mental health crisis.
- National Suicide Prevention Lifeline 1-800-273-TALK : Talk to a crisis counselor 24 hours a day, 7 days a week. TTY users can call 1-800-799-4889.
- Medicare.gov/talk to someone: Click on your state to find resources for opioid treatment programs or your state Medicaid offices.
- Mentalhealth.gov offers one-stop access to U.S. government mental health and mental health problems information.
| 1-800-856-4398 |
How Has Expanded Telehealth Coverage Affected Access To Mental Health Benefits And Substance Use Disorder Benefits During The Covid
Prior to the COVID-19 pandemic, Medicare coverage of telehealth services was very limited. Before the COVID-19 public health emergency, telehealth services were generally available only to beneficiaries in rural areas originating from a health care setting, such as a clinic or doctors office. One exception, however, was the removal of the geographic and originating site restrictions for individuals diagnosed with a substance use disorder for the purposes of treatment of such disorder or co-occurring mental health disorder, as of July 1, 2019, based on changes included in the SUPPORT Act.
During the COVID-19 public health emergency, beneficiaries in any geographic area can receive telehealth services, and can receive these services in their own home, rather than needing to travel to an originating site. During the first year of the pandemic, 28 million Medicare beneficiaries used telehealth services, a substantial increase from the 341,000 who used these services the prior year. Beneficiaries used telehealth for 43% of all behavioral health services they received during the first year of the pandemic, including individual therapy, group therapy, and substance use disorder treatment, compared to 13% of all office visits. Behavioral health represented 12.4% of all telehealth services received during the first year of the pandemic.
What Mental Health Benefits And Substance Use Disorder Benefits Does Medicare Cover
Medicare covers a range of mental health and substance use disorder services, both inpatient and outpatient, and covers outpatient prescription drugs used to treat these conditions. Medicare Advantage plans are required to cover benefits covered under traditional Medicare and most cover Part D prescription drugs as well, but out-of-pocket costs may differ between traditional Medicare and Medicare Advantage plans, and vary from one Medicare Advantage plan to another.
Inpatient Services
Medicare Part A covers inpatient care for beneficiaries who need mental health treatment in either a general hospital or a psychiatric hospital.
Outpatient Services
Medicare Part B covers one depression screening per year, a one-time welcome to Medicare visit, which includes a review of risk factors for depression, and an annual wellness visit, where beneficiaries can discuss their mental health status. Part B also covers individual and group psychotherapy with doctors , family counseling , psychiatric evaluation, medication management, and partial hospitalization. Partial hospitalization is a more structured program of individualized and multidisciplinary outpatient psychiatric treatments that is more intensive than in a doctor or therapists office, as an alternative to an inpatient stay. Partial hospitalization programs are designed for patients with mental health conditions who do not require 24-hour inpatient care, but have not benefitted from a less intensive outpatient program.
Read Also: How Do You Get A Medicare Part B Penalty Waiver
What Medicare Covers For Outpatient Mental Health Services
Medicare Part B, which pays doctor bills and related health care expenses, covers many mental health services rendered to patients not admitted to a hospital. Covered costs include:
-
An initial Welcome to Medicare visit that includes a review of your risk factors for depression.
-
One depression screening per year, performed in the office of a primary care doctor or in a primary care clinic that provides follow-up treatment and referrals.
-
Psychiatric evaluation to diagnose mental illness and prepare a care plan.
-
Diagnostic testing.
-
Individual and group psychotherapy or counseling provided by physicians or certain other professionals licensed to do so in your state.
-
Family counseling where the main purpose is to aid in your mental health treatment.
-
Medication management and some prescription drugs that are not self-administered.
-
Partial hospitalization, which typically includes many hours of treatment per week without admission to a hospital.
-
Testing to find out if youre getting the services you need and if your current treatment is helping you.
-
An annual wellness visit with a doctor or other provider to discuss any mental health changes.
How Much Do Medicare Beneficiaries Pay For Mental Health Benefits And Substance Use Disorder Benefits
Inpatient Services
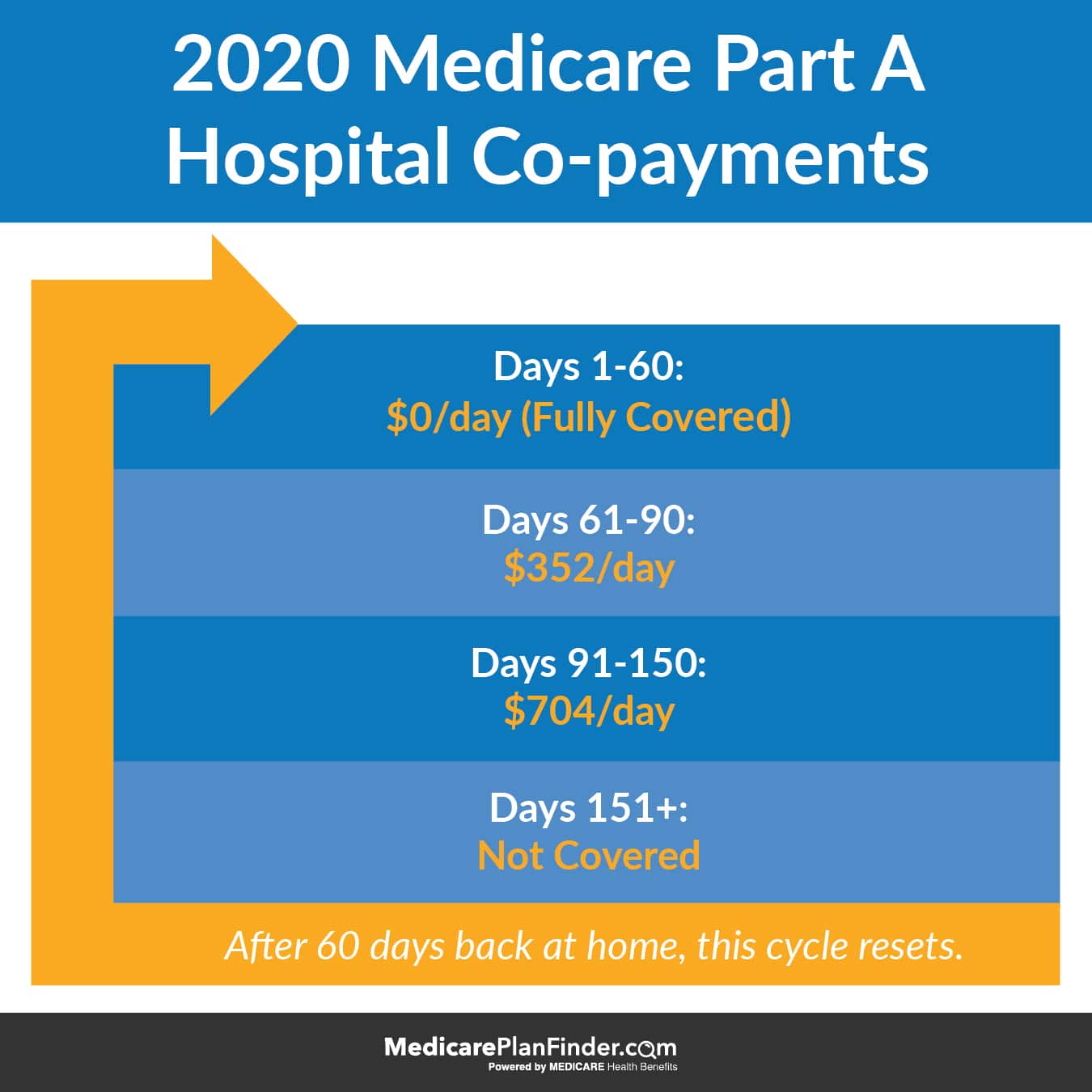
Beneficiaries who are admitted to a hospital for inpatient mental health treatment would be subject to the Medicare Part A deductible of $1,556 per benefit period in 2022. Part A also requires daily copayments for extended inpatient hospital stays. For extended hospital stays, beneficiaries would pay a $389 copayment per day and $778 per day for lifetime reserve days. For inpatient stays in a psychiatric hospital, Medicare coverage is limited to up to 190 days of hospital services in a lifetime. Most beneficiaries in traditional Medicare have supplemental insurance that may pay some or all of the cost sharing for covered Part A and B services.
Outpatient Services
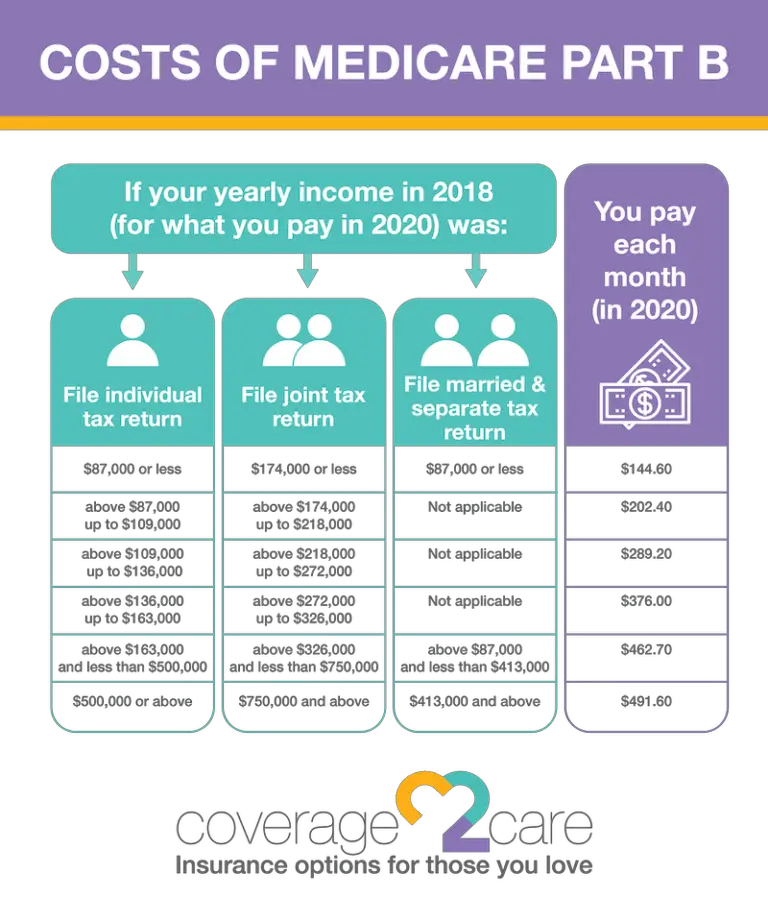
For most outpatient services covered under Part B, there is a $233 deductible and 20 percent coinsurance that applies to most services, including physician visits. However, some specific Part B services have different cost-sharing amounts :
Prescription Drugs
Those with Part D coverage face cost-sharing amounts for covered drugs and may pay an annual deductible and a monthly premium. For example, most Part D enrollees pay less than $10 for generic drugs, but many pay $40-$100 for brand-name drugs. Beneficiaries with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing.
You May Like: Will Medicaid Pay My Medicare Premium
Which Health Providers Can Bill Medicare Directly For Mental Health And Substance Use Disorder Services And How Much Does Medicare Pay For These Services
Medicare provides coverage and reimbursement for mental health services provided by psychiatrists or other doctors, clinical psychologists, clinical social workers, clinical nurse specialists, nurse practitioners, and physician assistants. Medicare does not provide coverage or reimbursement for mental health services provided by licensed professional counselors and licensed marriage and family therapists.
Medicare fees vary by type of provider, according to the Medicare Physician Fee Schedule :
Does Medicare Cover Inpatient Psychiatric Care
Inpatient psychiatric mental health care falls under Part A benefits. Further, Part A will cover a portion of the cost for the room, meals, nursing, and other services. You can obtain care in a hospital or psychiatric hospital.
But, the lifetime limit of inpatient psychiatric hospital care is 190 days. Also, you may incur costs for Part B while an inpatient in the hospital, this could be from doctor services.
Don’t Miss: What Will Medicare Pay For Home Health Care
Does Medicare Cover Counseling Services
Yes, Medicare covers counseling and therapy services as long as they are provided by a qualified professional licensed in your state who accepts Medicare assignments. With Original Medicare, counseling is covered as an outpatient service under Part B. You are responsible for 20% coinsurance payments for each session. With a Medicare Advantage Plan, counseling is covered. Still, you must typically pay a copay for each session and abide by your plans rules regarding network providers, referrals, and prior authorizations.
What Outpatient Mental Health Care Services Does Medicare Cover
Medicare covers these outpatient mental health services:
- One depression screening per year that must be done in a primary care doctors office or primary care clinic that can provide follow-up treatment and referrals.
- Individual and group psychotherapy with doctors or certain other licensed professionals are allowed by the state where you get the services.
- Family counseling, if the main purpose is to help with your treatment.
- On-going evaluation and testing to find out if your plan of care for services and treatment is helping you.
- Psychiatric evaluation.
- Medication management.
- Certain prescription drugs that arent usually self-administered , like some injections.
- Diagnostic tests.
- Partial hospitalization for more intensive treatment.
- A one-time Welcome to Medicare preventive visit that includes a review of your possible risk factors for depression.
- A yearly Wellness visit when you can talk to your health care provider about changes in your mental health.
- Treatment of inappropriate alcohol and drug use.
Your costs for Medicare outpatient mental health services:
- You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment, or in the case of a Medicare Advantage Plan, are in-network
You May Like: Does Medicare Pay For Wheelchair Lifts For Vehicles
What Original Medicare Doesnt Cover
Your health care provider may recommend you receive services more frequently than Medicare covers, or services that Medicare doesnt cover, and you may end up paying some or all of these costs. Ask your provider why they are recommending such services and whether Medicare will cover them.
You will have to pay for private duty nursing or a private room, unless its medically necessary. Other limits may apply.
Medicare Coverage For Depression
An estimated 17.3 million American adults had at least one major depressive episode in 2017. This number represented 7.1% of all U.S. adults. Many others suffered from bipolar disorder, dysthymia, seasonal affective disorder, premenstrual dysphoric disorder, and depressive symptoms related to medical conditions or substance use.
Treatment for these conditions may include medications, psychotherapy, and hospitalization as mentioned above. For severe depression that fails to respond to other treatments, electroconvulsive therapy or transcranial magnetic stimulation may also be an option.
Electroconvulsive therapy is a procedure that uses electrical currents to trigger seizure activity in the brain. The procedure is performed under anesthesia. Transcranial magnetic stimulation , on the other hand, uses alternating magnetic fields instead of electrical currents to stimulate targeted areas of the brain. Seizures are not induced with the procedure and no anesthesia is required.
Both treatments are FDA-approved but are generally reserved for treatment-resistant depression. By changing chemistry in the brain, namely the level of certain neurotransmitters, these treatments aim to reduce the severity of depressive symptoms.
For care to be covered, it must be sought at a Medicare-approved facility and must meet certain criteria to meet local requirements for coverage. Before seeking treatment, find out what those criteria are to avoid paying all costs out of pocket.
Read Also: What Is The Phone Number For Medicare Providers
How Does Medicare Cover Counseling
Medicare Part BMedicare Part B is medical coverage for people with Original Medicare benefits. It covers doctor visits, preventative care, tests, durable medical equipment, and supplies. Medicare Part B pays 80 percent of most medically necessary healthcare covers many different outpatient mental health services:Medicare.gov, Mental health care , Accessed November 3, 2021
Medicare Part AMedicare Part A is hospital coverage for Medicare beneficiaries. It covers inpatient care in hospitals and skilled nursing facilities. It also covers limited home healthcare services and hospice care. provides coverage for counseling services as part of treatment in an inpatient facility, such as a general hospital or psychiatric hospital.Medicare.gov, Mental health care , Accessed November 3, 2021
Does Medicare Cover Therapy Counseling And Psychologists
Medicare Part B covers mental health services from professionals like psychiatrists, doctors, clinical psychologists, clinical social workers, clinical nurse specialists, nurse practitioners, and physician assistants.
Family counseling will be covered, but only if its main function is to help with your treatment. Individual and group therapy are also covered however, it needs to be performed by a licensed doctor/professional in the state you reside in.
Original Medicare will only cover said visits if you receive them from a health care provider who accepts the assignment. Not all health care professionals will accept Medicare assignments.
You May Like: Will Medicare Pay For Hospice Care
Does Medicare Cover Occupational Therapy
If you need therapy to help you perform daily living activities, like dressing or bathing, Medicare Part B will cover a portion of the services delivered. Occupational therapy helps beneficiaries maintain daily capabilities or slow decline. Part B helps pay for medically necessary outpatient occupational therapy.
Does Medicare Offer Alcohol Misuse Screening & Counseling
Medicare covers one alcohol misuse screening per year for adults who use alcohol but dont meet the medical criteria for alcohol dependency. If your healthcare provider determines youre misusing alcohol, you can get up to four brief face-to-face counseling sessions per year in a primary care setting from a qualified provider.
Medicare doesnt cover:
- Screening or counseling with a non-qualified or out of network provider
- Additional free counseling sessions beyond the four that are allowed
Your costs:
- You pay nothing if the qualified primary care doctor or other primary care practitioner accepts the assignment.
- With a Medicare Advantage Plan, your cost or copay depends on your plans rules. Typically, if a Medicare-covered service is no cost with Original Medicare, your Medicare Advantage Plan will follow suit.
Read Also: Do You Pay Medicare After Retirement
Medicare Eligibility Benefits And Coverage For Mental Health Care
You are eligible for mental health care coverage if you receive Medicare benefits through Original Medicare or a Medicare health plan, including Medicare Advantage Plans. As with all Medicare-covered services, mental health care must be deemed medically necessary. That is, needed according to accepted standards of medicine to diagnose or treat your mental health condition.
You must receive services from licensed professionals who agree to charge what Medicare approves for payment. If you have a Medicare Advantage Plan, you must follow your plans rules for how you receive mental health services, including network, referral, and prior authorization requirements.
Medicare for mental health includes inpatient and outpatient care. Medicare also covers prescription medications, but you must have a Medicare prescription drug plan or a Medicare Advantage Plan that includes drug coverage.
| Medicare clan |
|
What Rules Do Medicare Part D Plans Have Regarding Prescription Drugs For Mental Health
Medicare Part D plans must include safeguards for mental health prescription drugs, many of which are considered controlled substances due to their misuse or abuse potential. Drug plan coverage rules include:
- Opioid safety checks, which may apply if you are taking opioids for pain management along with other commonly used drugs for mental health, like an anti-anxiety medication
- Prior authorization, which may be required depending on your plans rules
- Quantity limits, for safety and cost reasons, a one months supply is standard
- Step therapy, which means that you may be required to try a lower tier, less expensive medication to treat your condition first before using a higher tier drug
Your prescribing physician and pharmacist should be involved in advocating for you to receive the prescription medications that work best for you. You can submit an exception to your plan to request a medication that is not typically covered on their formulary or would bypass step therapy. You must have written documentation and a request from your prescribing physician.
Don’t Miss: Who Is Eligible For Medicare Advantage Plans
Which Insurance Company Covers Mental Health
Bupa and Medibank cover for mental health compared Both funds have a number of other extras policies. Use our online tool to compare health insurance policies from all 36 health funds. How do Bupa and Medibank compare when it comes to psychology? *NSW, Single per month, before health insurance rebate.
Medicare And Outpatient Mental Health Care
If you have Medicare Part B, it can cover a variety of outpatient mental health services, medical supplies, and preventative care. These services include:
- One depression screening per year
- This needs to be performed in a primary care doctors office or clinic so that follow-up treatment and referrals can be administered.
Don’t Miss: What Is Cigna Medicare Supplement Plan G
How Does Medicare Work For Therapy
Medicare covers many forms of therapy, including psychotherapy. This is also referred to as talk therapy. Studies show that psychotherapy tends to be beneficial to about 75% of the people who pursue it to address mental health challenges.
Medicare also helps cover hospitalization at a general or psychiatric hospital if you are admitted for inpatient care. Medicare limits the number of days of inpatient psychiatric hospital services covered during your lifetime.
Your mental health therapy and other services typically are not free under Medicare. You may get free mental health screenings, but you typically have to pay 20% of the Medicare-approved amount for the majority of services. Your total out-of-pocket expenses will depend on your deductible, coinsurance, provider fees, and location where you receive services.
What Outpatient Mental Health Care And Professional Services Does Medicare Cover
Medicare for mental health includes outpatient services that you receive outside of an inpatient setting, such as a clinic, doctors office, community mental health center, residential treatment facility, or outpatient hospital department. Common services include individual and group counseling, depression screening, medication management, and treatment for alcohol and drug abuse.
If you have Original Medicare, outpatient mental health care and services are covered under Part B. If you have a Medicare Advantage Plan , outpatient mental health care and services are covered by your plan according to Medicare guidelines. Still, your plan sets rules on how you obtain care.
Recommended Reading: Do Assisted Living Facilities Accept Medicare