How Do I Know If Im Eligible For Free Therapy
To be eligible for free therapy, you need to enrol in Medicare. What this means is that youve opted in to let Medicare assist you with the cost of healthcare in Australia. While they dont cover everything, enrolling can help you access a wide range of health care services. Including those for mental health.
People who can enrol in Medicare are:
-
Australian citizens,
You may also be able to apply to enrol in Medicare if youre visiting Australia from a country. Provided your country of origin has a reciprocal healthcare agreement with Australia. .
Not sure if youre eligible? Its worth checking out some additional information over at
Enrolling means filling out Medicares form and providing some certified documents relating to your identity. Once youre enrolled, youll be able to access a range of mental health services at a lower or free rate.
What If Ive Still Got Sessions On My Last Mental Health Care Plan But Its A New Calendar Year
Okay, so strap in this is where it gets a little confusing for everyone involved.
Remember that youâre allowed 20 rebated sessions per calendar year, but hereâs the funny thing your GP is only allowed to provide you with a Mental Health Care Plan once every 12 months.
So letâs say you used 8 sessions one year from a plan that was created in October. As soon as January 1st rolls around youâre entitled to a new 20 sessions for that new year. But, your GP canât write a new plan until October. What to do?
Basically, you use those remaining 2 sessions with your Psychologist and then youâll have to go back to your doctor for a Mental Health Care Review/Re-referral. Because itâs a Review and not new Mental Health Care Plan, the Doctor can only provide an additional 4 sessions. Once those 4 sessions are up youâll have to go back again for another Review. And so on. So youâll still get your 20 sessions for the year, just with a little more leg work.
Isnât red tape great? Please donât ask me to create a diagram of that!
Getting The Counseling You Need
You dont have to wait for your annual wellness visit or depression screening to talk to your doctor about mental health care. Medicare pays for visits with your primary care doctor if you want to talk about your mental health concerns now.
So, if you feel anxious or depressed, make an appointment with your doctor without delay. Medicare pays for mental health evaluations and tests to help your doctor diagnose a potential problem. Medicares comprehensive mental health coverage means youll get the counseling services you need to feel your best.
AgingInPlace.org keeps our resources free by working as an affiliate partnerwith some companies mentioned on our site. We may earn a commission when you click on certain product links.
Don’t Miss: What Is Deductible On Medicare
Does Medicare Cover Therapy With Prescription Drugs
If you receive mental health care services in an inpatient setting, Part A covers the medications your doctor prescribes.
If you receive outpatient counseling and therapy services, Part B typically doesnt cover any prescription drugs your doctor recommends.
If you have a Part D prescription drug plan, medications for treatment for mental health conditions are usually covered. Medicare requires all Part D plans to cover all antidepressant and antipsychotic medications approved by the FDA.
As Part D is private insurance, your copayments and deductible are set by the insurance company. You may have coverage restrictions with certain medications. For example, your plan may first require a trial with a less expensive medication before it pays for a more expensive one. You may need prior authorization for psychiatric medications, and there may be quantity limits that restrict how many doses you can get at one time.
You can find specifics about your prescription drug coverage in your plan formulary. The formulary is a list of medications covered by your plan and what you pay for each one. It also lists any restrictions and special requirements associated with each drug, such as prior authorization required for use and/or procurement.
What Is A Mental Health Treatment Plan
A Mental Health Treatment Plan is a plan for people with a mental health disorder. If you have mental health issues, your doctor can write a plan for you.
The plan identifies what type of health care you need and spells out what you and your doctor have agreed you are aiming to achieve. It may also refer you to local mental health services.
Don’t Miss: Does Medicare Pay For Penile Pumps
Does Medicare Cover Online Counseling
Medicare didnt used to cover online therapy, but it does now. In 2020, Medicare removed many long-standing restrictions on its coverage of telemedicine.
In the past, Medicare only covered telehealth services provided in rural locations and other federally designated Professional Shortage Areas. It also covered telehealth services only when they were provided in a medical facility like a hospital or clinic. This ruled out in-home telehealth services like online counseling.
Thanks to the changes made to Medicare policy in 2020, Medicare no longer limits telehealth coverage to people in rural areas and now covers telehealth services provided in a persons home.
For more information, you can go to Medicares telehealth coverage information page.
What Part Of Medicare Covers Mental Health Care
Medicare Part A covers mental health care in an inpatient setting. Part A mental health care is in a general hospital or a psychiatric hospital only for people with mental health concerns. If you get inpatient care in a psychiatric hospital, Part A will cover up to 190 days in a lifetime. There is no limit to the number of benefit periods you can have for mental health care in a general hospital.
Part A covers your room , meals, nursing care , therapy and treatment, lab tests, medications, and other services and supplies you need. Part A does not cover personal items or a phone or TV in your room.
Medicare Part B covers mental health care on an outpatient basis in these types of settings:
- A doctors or other health care providers office
- A hospital outpatient department
- A community mental health center
And from these types of providers :
- Psychiatrist or another doctor
- Clinical psychologist, social worker, or nurse specialist
- Nurse practitioner
- Physician assistant
Part B helps pay for these outpatient mental health services:
Part D helps cover self-administered prescribed drugs.
Medicare Advantage plans cover all services offered through Original Medicare Part A, Part B, and usually Part D. Copays and coinsurance amounts vary, depending on your plan. Providers and services must be in-network and typically require referrals and prior authorizations before you can receive services.
Don’t Miss: Can A New Immigrant Apply For Medicare
How Much Does Therapy Cost With A Medicare Plan
Therapy with Medicare will cost different amounts depending on your location, plan, and provider:
- Location: Even though Medicare is a federal health insurance program, each state is responsible for its own Medicare policies. This means that Medicare plans look different across state lines.
- Plan: Receiving your Medicare coverage directly from the state or through a health insurance company will impact your coverage. Sometimes, health insurance companies offer different benefits and have access to different resources.
- Provider: Not all therapists take Medicare for the therapists that do not, you will have to pay the session costs.
In general, for an in-network Medicare provider, expect to pay a copayment or coinsurance for each visit to your therapist. Medicare copayments are generally around $20 and coinsurance rates around 20%, though these will vary based on your situation. For out-of-network therapists, you will typically be responsible for a larger portion of the session fee. Seeing a non-Medicare therapist also may require preauthorization from your Medicare plan.
It is important to note that some Medicare plans limit the number of therapy sessions for which a person receives coverage. Some plans are limited by visit number or by cost . Before starting therapy, learn if your plan limits your care so you dont have to stop in the middle of your treatment.
How Do I Get Rebates From My Psychologist Under A Mental Health Care Plan
Getting your actual rebate all depends on how your Psychologist chooses to operate. Psychologists have two choices to facilitate your rebate: make you do it, or give you a break and do it themselves.
If they choose to get you to do it youâll be provided with an invoice and then have to make your way to Medicare and submit the request yourself.
Alternatively, your Psychologist may opt to submit the request for you. In this instance your Psychologist will still provide you with an invoice, but they will then use the online gateways available to them to submit the rebate request. This normally results in the funds arriving in your bank account within around 24-48 hours.
Also Check: Do I Have To Sign Up For Medicare Part D
Mental Health Treatment Plans
If you have a mental health disorder, you and your doctor can create a plan to treat it.
Your mental health treatment plan will have goals agreed by you and your doctor. Itll also have:
- treatment options
- support services available.
Keep in mind your health information and treatment plan will be private. Doctors cant share your information unless you agree to it.
What Is A Mental Health Care Plan
A Mental Health Care Plan is a brief document created by your General Practitioner , Psychiatrist, or Paediatrician that reviews your current mental health.
To obtain a Mental Health Care Plan youâll need to sit down with your Doctor and complete an assessment. During this time theyâll check in on your current coping, take a short history and may ask you to complete a questionnaire.
Once this is completed your Doctor will create your plan which makes you eligible to receive 6 rebated sessions with any registered Psychologist courtesy of Medicare. After your 6 sessions you can return to your Doctor to get a âreviewâ of your Mental Health Care Plan which may land you another 4 sessions. And now due to COVID-19, you can request an additional 10 sessions once you have completed your normal Medicare sessions.
So each calendar year youâre entitled to receive up to 20 sessions with a Psychologist and get the Medicare rebate.
Recommended Reading: Where Do I File For Medicare
Low Cost Or Free Mental Health Services
3-minute read
If you have a mental health condition that needs treatment, you might be able to get help with payment through a government program.
If you qualify for the Better Access initiative, you will be able to receive a Medicare rebate for selected mental health services.
Your GP can also refer you to psychological services through the local Primary Health Networks. These have funding to provide services to populations in their area deemed to be at high risk or that have poor access to mental health support. Ask your GP if you can access these services.
Can I Claim Psychology Sessions On Both Medicare And Private Insurance

That would be nice wouldnât it? In an ideal world you wouldnât be penalised for trying to look after yourself and your family. Unfortunately, you can only claim back money on your sessions with either a Mental Health Care Plan or your private health fund.
Of course once youâve used up all of your 20 Medicare sessions for the year youâre welcome to change to using your private health insurance for any other sessions you attend.
Recommended Reading: Are Podiatrists Covered By Medicare
Medicare And Mental Health Coverage
When a person first enrolls in Medicare, they receive a Welcome to Medicare preventive visit. During this visit, a doctor reviews risks of depression.
Yearly wellness visits can then include discussions with a persons doctor on any changes to mental health that may have occurred since the last visit.
In addition to the wellness visits, Medicare covers certain mental health services both inside and outside of a hospital.
If You Have Medicare And Need Mental Health Services What Can You Expect To Pay Out Of Pocket
Medicare doesnt cover 100% of the costs for mental health services. You will typically have to pay a monthly premium, annual deductible, and coinsurance. Your payment will all depend on the services you need. Medicare Part A covers hospital insurance, and Medicare Part B provides medical insurance for mental health services.
There are usually no monthly premiums for Medicare Part A. The reason is that most people work enough hours during their lifetime to qualify for premium-free Part A. This is 40 quarters or 10 years for either you or your spouse.
Medicare Part A has a deductible of $1,556 for 2022. This is for the admission to a hospital or psychiatric facility for each benefit period. A supplemental Medicare plan will cover part or all of the deductible.
| Over 90 days | $778 per day for up to 60 days.This is called the lifetime reserve. Medicare gives you a total of 60 reserve days during your lifetime. You are responsible for paying 100% of your costs after youve used your lifetime reserve days. |
For example, suppose you spend 63 days in a psychiatric facility. You will pay the $1,556 deductible and $1,167 for 3 days of coinsurance. The total will be $2,723.
If you need psychotherapy and other mental health services, youll need to review the costs of Medicare Part B.
Also Check: Are Doctors Required To Accept Medicare
You May Now Access 20 Medicare Subsidised Counselling Sessions Per Year
You will require a MHCP to be eligible for a Medicare rebate to reduce your out-of-pocket expenses.
New Vision Psychology applauds the Australian Governments announcement to provide ten additional Medicare subsidised psychological therapy sessions per year, increasing from 10 psychology sessions to 20.
Physical distancing, isolation, and financial uncertainty as a result of coronavirus has undoubtedly increased levels of anxiety, stress and worry among the population and we echo Treasurer Josh Frydenbergs statement that mental health and suicide prevention is a national priority.
The additional $100.8 million in funding for the Better Access initiative is welcomed,
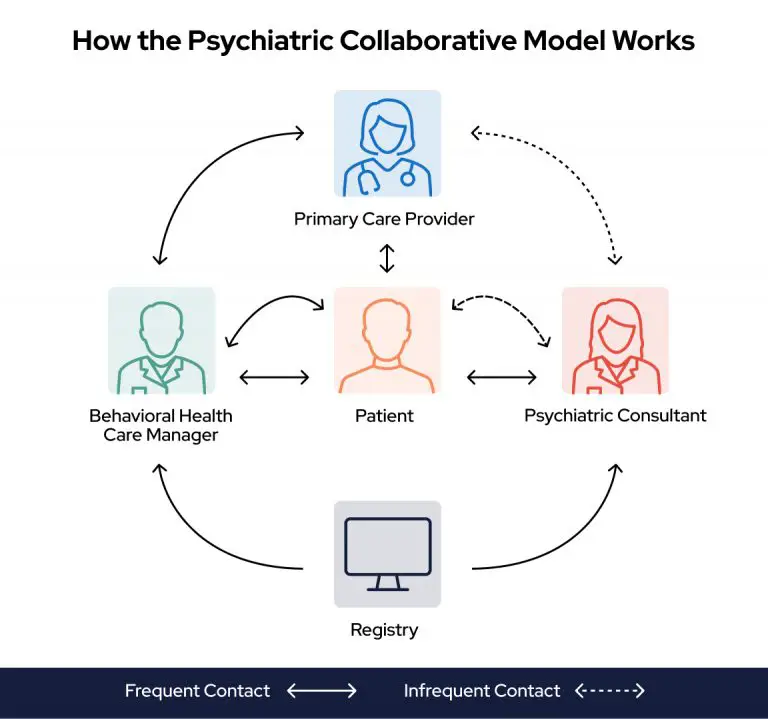
The Better Access to Psychiatrists, Psychologists and General Practitioners through the Medicare Benefits Schedule initiative provides GPs with a structured framework to provide early intervention, assessment and management of people with mental disorders. In essence, the Better Access initiative hopes to provide better access to mental health practitioners through Medicare.
As such, Medicare rebates are available for psychological treatment by registered psychologists. Under this scheme, individuals diagnosed with a mental health disorder can access up to 10 individual Medicare subsidised psychology sessions per calendar year.
As of October 9, 2020 this has been doubled to 20.
Medicare Part D And Medigap
Medicare Part D covers prescription drug benefits. Part D plans help pay for antidepressants, mood stabilizers, and most other protected mental health treatment medications.
If you do not have a Medicare Advantage plan, Medigap may also pay for some of your deductibles, copayments, and coinsurance related to inpatient or outpatient care.
You May Like: Where Do I Get A New Medicare Card
Can A Supplemental Medicare Plan Provide Coverage For Mental Health
A supplemental Medicare or Medigap plan is private insurance. You pay a monthly premium, and the policy covers one person. You still have to pay premiums on Medicare Part A and Part B.
Medigap plans are for the gaps in coverage for Medicare. These Medigap policies may include Plan A, B, C, D, F, G, K, L, M, or N. A Medigap plan will pay for all or part of the deductible, copays, and coinsurance for Medicare Part A and Part B. This includes coverage for qualified mental health services. You may want to seek the help of an insurance agent or financial planner to help you pick the best plan for you.
Does Medicare Cover Counseling
- Activity therapies like art, dance, and music therapy
- Family counseling to address a mental health condition
- Drugs that usually arent self-administered
- An annual depression screening with a primary care physician
- An annual alcohol misuse screening with a primary care physician
Medicare Part B has an annual deductible that changes over time. It was $183 in 2018 and is $233 in 2022. After the deductible, Medicare covers 80% of outpatient services and you have to pay 20% coinsurance on the Medicare-approved amount for the service you are receiving.
The standard monthly premium for Medicare Part B in 2022 is $170.10. This amount is usually deducted from your Social Security check.
Read Also: How Much Is Taken Out Of Ss For Medicare
Does Medicare Cover Mental Health Services Like Therapy
Sometimes it can be hard for older adults to separate signs of mental health problems from aging-related changes. You may think that feeling sad or anxious is a normal part of getting older, especially when you live with challenging health conditions or lose loved ones.
Medicare covers many benefits to care for your mental well-being, including psychological counseling, preventive screenings, and outpatient treatment programs
Hereâs an overview of Medicareâs mental health coverage.
How Much Does Medicare Cover For Therapy
The typical monthly premium for Medicare Part B is $170.10 for 2022. It could be more than that if your income in 2020 exceeds the thresholds. There is also an annual deductible of $233. After you pay your deductible, you may have a coinsurance of 20%. The coinsurance is calculated using the Medicare-approved amount.
For example, suppose you have a $1,000 bill for mental health therapy services.
-
You will pay the $233 annual deductible. This is what you pay before Medicare covers any qualified expenses for therapy.
-
Then, you will pay 20% of $767 for coinsurance. Coinsurance represents your share of health care costs you split with your insurer until the end of the plan year. You pay your coinsurance after youve met your annual deductible.
-
Your total out-of-pocket expenses will be $386.40 . Traditional Medicare does not have any limits on out-of-pocket expenses.
You May Like: Can Medicare Cancel Your Coverage
