What Kind Of Medicare Coverage Is Best If You Need Home Health Aides
Home health aide services are covered under Medicare Part A, long as you qualify for home health services and require the services of another skilled professional. Your copay for home health aide services provided within the limits set by Medicare is $0. You can receive your services from any Medicare-approved home health agency.
If you have a Medicare Advantage Plan instead of Original Medicare, your requirements and coverage for home health aide services are the same. Home health aide services are a Medicare-covered service under Part A, so Medicare Advantage Plans must offer the same coverage as Original Medicare. Your Medicare Advantage Plan may require you to receive home health care services from an in-network home health agency, and a copay or coinsurance may apply, depending on your plan.
If you receive your Medicare benefits through a Medicare health plan , contact your plan to find out how it provides your Medicare-covered home health benefits.
Does My Medicare Cover Dental
Medicare doesnt cover most dental care, dental procedures, or supplies, like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices. Part A can pay for inpatient hospital care if you need to have emergency or complicated dental procedures, even though it doesnt cover dental care.
Effects Of The Patient Protection And Affordable Care Act
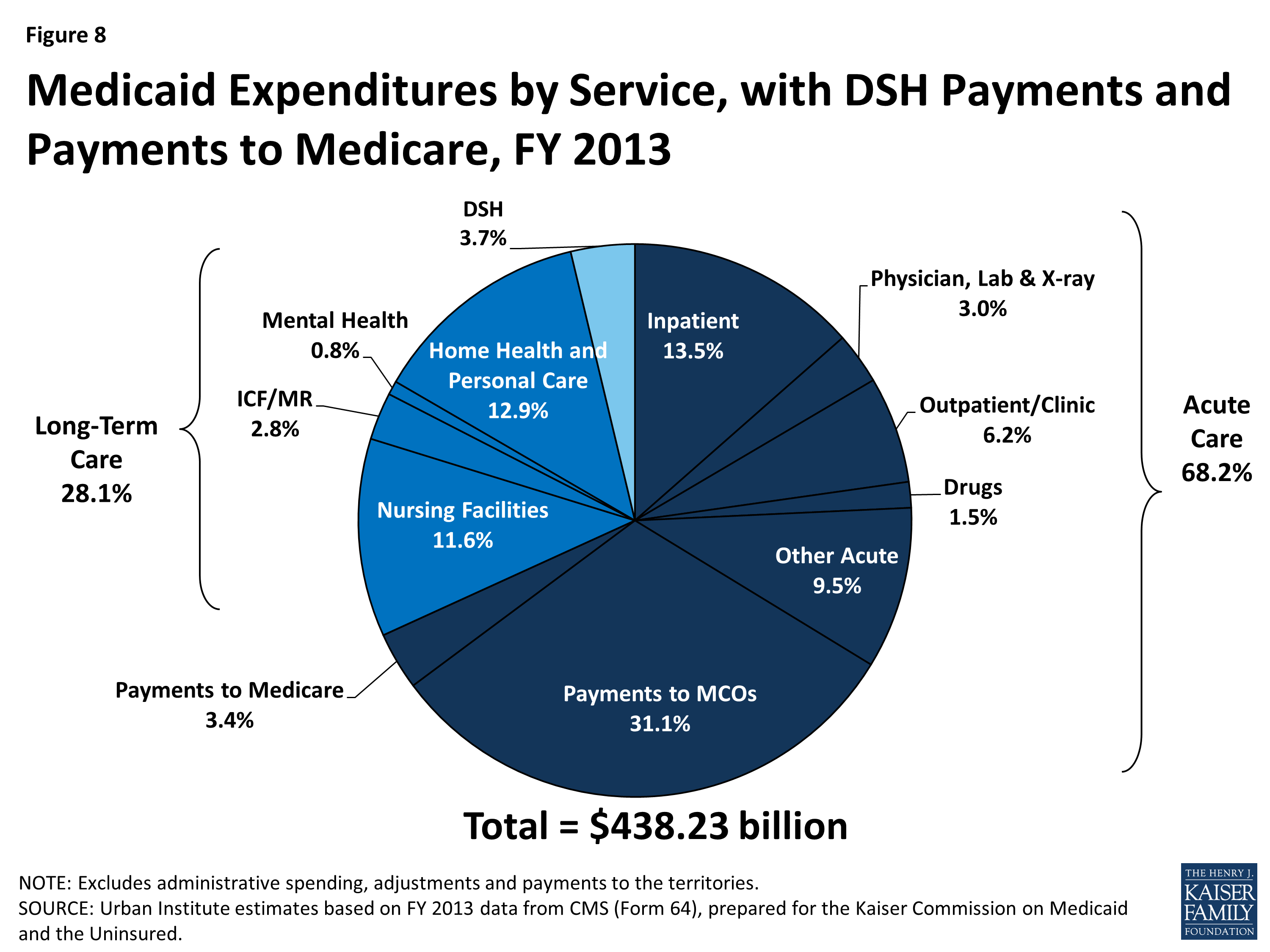
The Patient Protection and Affordable Care Act of 2010 made a number of changes to the Medicare program. Several provisions of the law were designed to reduce the cost of Medicare. The most substantial provisions slowed the growth rate of payments to hospitals and skilled nursing facilities under Parts A of Medicare, through a variety of methods .
PPACA also slightly reduced annual increases in payments to physicians and to hospitals that serve a disproportionate share of low-income patients. Along with other minor adjustments, these changes reduced Medicareâs projected cost over the next decade by $455 billion.
Additionally, the PPACA created the Independent Payment Advisory Board , which was empowered to submit legislative proposals to reduce the cost of Medicare if the programâs per-capita spending grows faster than per-capita GDP plus one percent. The IPAB was never formed and was formally repealed by the Balanced Budget Act of 2018.
Meanwhile, Medicare Part B and D premiums were restructured in ways that reduced costs for most people while raising contributions from the wealthiest people with Medicare. The law also expanded coverage of or eliminated co-pays for some preventive services.
Recommended Reading: When Is The Next Medicare Open Enrollment
Don’t Miss: How To Apply For Medicare Card Replacement
Find A Home Health Care Provider
You can search for a provider by using the online home health care provider tool at Medicare.gov. Just enter your zip code and the tool will give you a list of home health care providers in your area. You can also ask your doctor, hospital social worker or discharge administrator to arrange for a home health provider in the event you need home care after a hospital stay.
Dont let an injury or illness prevent you from getting the help you may need. Talk to your doctor and ask if you qualify for home health care.
Read Also: Which Medicare Plan Covers Hearing Aids
Is Home Health Covered Under Part A Or Part B Medicare
Actually, it turns out that both Part A and Part B cover certain aspects of home health care.As you probably know, Medicare is broken down into several parts. Once your insurance approves a senior for Medicare, theyll get coverage under either Part A or Part B. You may have heard of these terms in passing, but now that they apply to someone you love, youll want to learn about them as much as you can.
Recommended Reading: Can I Submit A Claim Directly To Medicare
What Parts Arent Covered
There are some aspects of in-home care that are convenient and even sometimes necessary to help sustain certain lifestyles, but they arent all covered by Medicare. These services include:
- 24-hour skilled nursing care: If you or a loved one needs this, you may be better off in a skilled nursing home facility, which Medicare does cover.
- Meals delivered to your home: While there may be aides who help do this in your home, you will not be reimbursed for having meals brought to you because you cant leave the house.
- Custodial care when its the only service you need: Custodial care refers to any non-medical help you need, such as with bathing or getting dressed. However, this type of care could be included in your plan if your doctor deems that its necessary to improve your condition.
- Homemaker services: This includes activities such as shopping, cleaning, and laundry, as described by the Medicare website. This also could be covered if they are related to your home health plan prescribed by your doctor.
So now that we know what Medicare covers , lets discuss how you can qualify for in-home care.
MORE ADVICE
MORE ADVICE Discover more tips for comfortably aging in place
You cant simply decide that you prefer your nursing care and other therapy needs in your home. You must meet the qualifications for in-home care.
What If My Home Health Care Is Ending Too Soon
If your home health care is ending, it is likely because you are getting better and no longer need it. But that is not always the case and you may feel that your home health care coverage is ending prematurely. If so, you can file a fast appeal to continue home health care.
When you receive your NOMNC, it will let you know when your services are ending and instructions on how to file for a fast appeal. A Beneficiary and Family-Centered Care Quality Improvement Organization will go over your appeal, discuss your condition with your doctor, and notify you of their decision within three days after the end date on the NOMNC.Medicare.gov, Medicare & Home Health Care, Accessed December 15, 2021
Don’t Miss: Does Medicare Cover Heart Catheterization
What Is Custodial Care Vs Skilled Nursing Care
Nursing homes mostly offer custodial care. You receive help with daily activities, such as bathing, eating, and dressing. Activities of Daily Living is the term used in the industry to refer to such activities, and help with ADLs can be provided by informal caregivers, such as family and friends, or formal caregivers who are associated with a formal service system, like a home health agency. Help with ADLs is not provided by doctors and nurses.
Medicare does not cover custodial care. But Medicare Part A will cover medically necessary care that requires skilled nursing care or therapy. You must receive it at one of the over 15,000 Medicare-certified nursing facilities in the U.S.2A beneficiary can also receive skilled nursing care or therapy at home, as home health care, discussed later.
A skilled nursing facility offers more medical services than a traditional nursing home or assisted living facility. A facility may provide both skilled nursing care and custodial care. You will receive care from a qualified technician or health professional. For example, a registered nurse may inject medicine into your body intravenously.
- Physical, occupational or speech therapy
- Medications, supplies, and equipment
Medicare Coverage: What Costs Does Original Medicare Cover
Heres a look at the health-care costs that Original Medicare may cover.
If youre an inpatient in the hospital:
- Part A typically covers health-care costs such as your care and medical services.
- Youll usually need to pay a deductible .
- You pay coinsurance or copayment amounts in some cases, especially if youre an inpatient for more than 60 days in one benefit period. Your copayment for days 61-90 is $371 for each benefit period in 2021.
- After youve spent more than 90 days in the hospital during a single benefit period, youll generally have to pay a coinsurance amount of $742 per day in 2021. You pay this coinsurance until youve used up your lifetime reserve days . After that, you typically pay all health-care costs.
*A benefit period begins when youre admitted as an inpatient. It ends when you havent received inpatient care for 60 days in a row. You could have more than one benefit period within a year, and you generally pay a deductible for each benefit period.
If youre not a hospital inpatient:
For example, if the Medicare-approved amount for a doctor visit is $85, your coinsurance would be around $17, if youve already paid your Part B deductible.
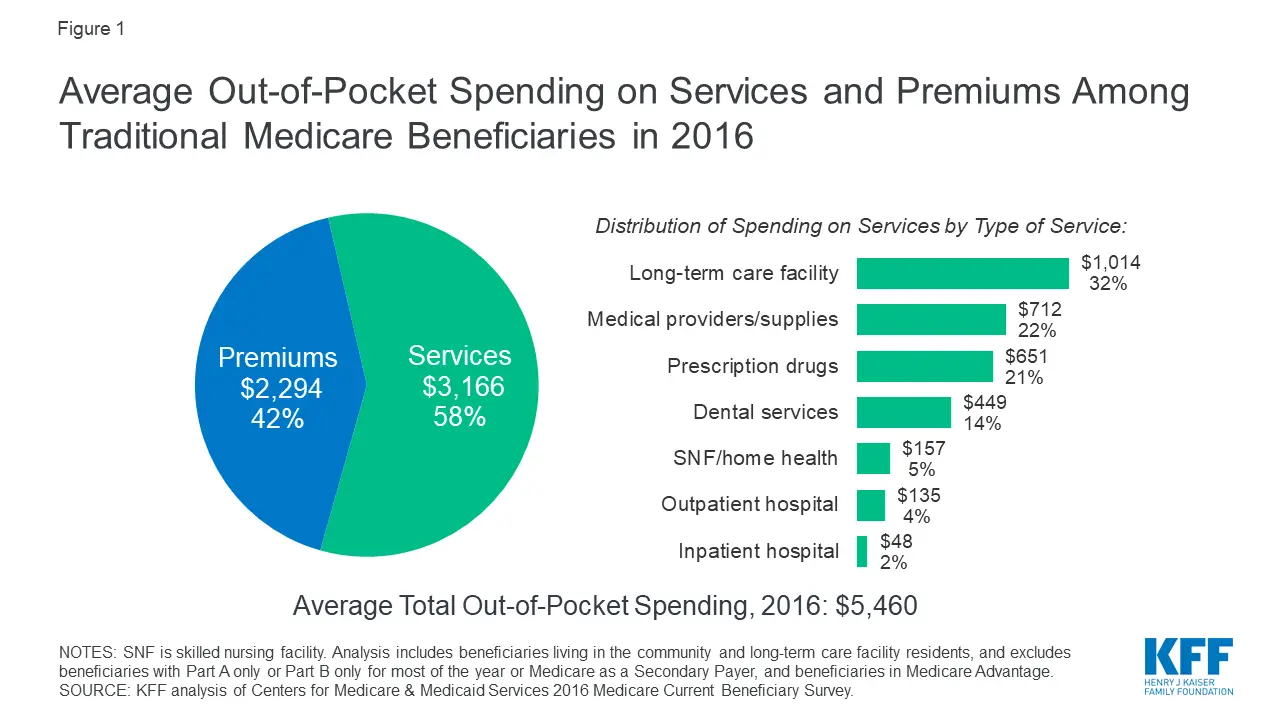
Be aware that Original Medicare has no annual out-of-pocket maximum spending limit. If you meet your Medicare Part A and/or Part B deductibles, you still generally pay a coinsurance or copayment amount and theres no limit to what you might pay in a year.
Don’t Miss: How Do I Sign Up For Medicare Supplemental Insurance
How Much Do Home Health Services Cost
If youâre eligible for Medicare coverage of your home health care, you generally donât have to pay for it. If you need durable medical equipment, youâll typically pay 20% of the Medicare-approved amount.
Be aware, however, that your doctor might request more home health care services for you than Medicare will approve. If you have questions, ask your doctor, or call Medicare at the number listed at the bottom of this page.
What Durable Medical Equipment Is Covered By Medicare
The cost of durable medical equipment is covered by Medicare if it is deemed medically necessary, and has been prescribed by a doctor for use at home. The list of covered durable medical equipment includes:
- Wheelchairs
- Nebulizers
- Blood sugar monitors.
You will pay 20% of the Medicare-approved amount for the equipment, and you will be liable for any remaining deductible under Medicare Part B.
Recommended Reading: Where Can I Go To Apply For Medicare
How Much Will I Have To Pay If I Qualify
With Original Medicare coverage , eligible seniors will pay nothing for home health care services that are ordered by a doctor and provided by a certified home health agency. Any additional services provided outside of the approved care plan will not be covered and must be paid for out of pocket.
Be aware that before services begin, the home health agency should provide an itemized receipt or plan of care that identifies what is eligible for Medicare coverage and what is not. A written notice called the Advance Beneficiary Notice of Noncoverage will detail any services and durable medical equipment that Medicare will not pay for as well as the costs the patient will be responsible for.
Use the guide below to determine the combination of payment options that will help your family cover home care costs.
What Home Health Services Are Not Covered By Medicare
Medicare doesnât typically cover home health aide services if the only care you need is âcustodial.â Custodial care doesnât require medical skills. Itâs care such as dressing or bathing assistance, eating, or using the bathroom. These are just a few examples of custodial care. Also, be aware that:
- Homemaker services, such as shopping or laundry, arenât generally covered under Medicare.
- Medicare doesnât cover meals delivered to your house.
- If you need round-the-clock care at home, Medicare generally doesnât cover it.
Don’t Miss: Is Medicare Solutions A Legitimate Company
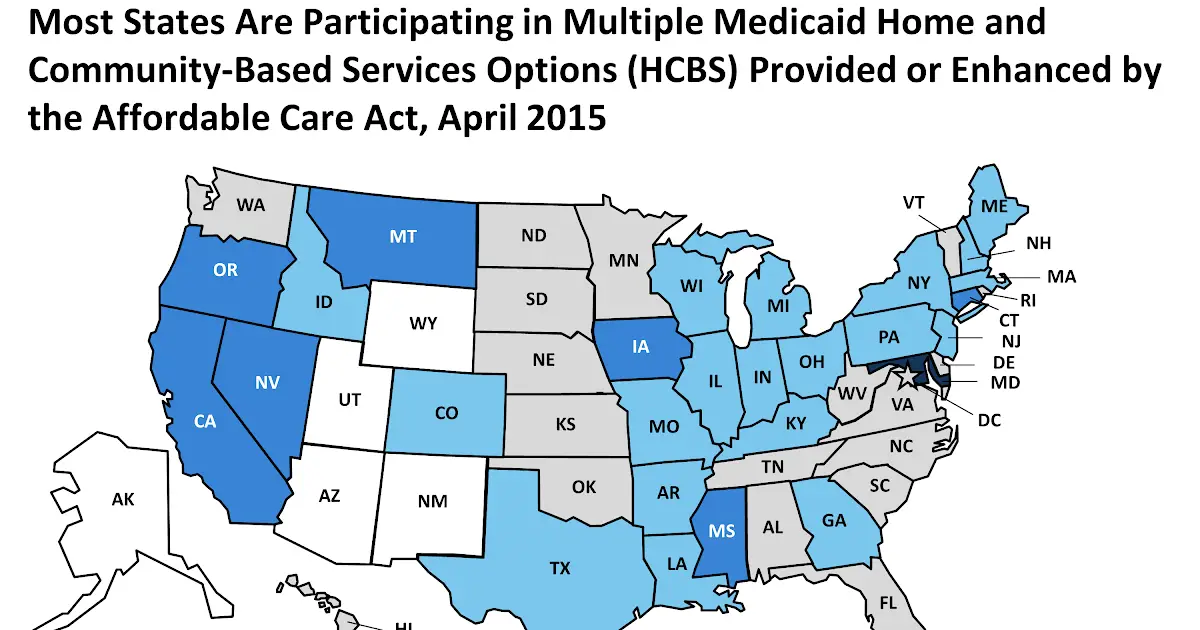
Getting Home Health Services In Certain States
If you live in Massachusetts, Michigan, Florida, Illinois, or Texas, a Medicare demonstration program might apply. Under the program, you can request a pre-claim review. This review can tell you early on whether Medicare is likely to cover your home health services. If youâre a resident of one of these states, you might want to request a pre-claim review as soon as your doctor orders home health care for you, so youâll know whether youâll have to pay anything.
Medicare information is everywhere. What is hard is knowing which information to trust. Because eHealthâs Medicare related content is compliant with CMS regulations, you can rest assured youâre getting accurate information so you can make the right decisions for your coverage.Read more to learn about our Compliance Program.
When You Need Part
Updated By Bethany K. Laurence, Attorney
Progressive health care professionals often encourage people to get out of hospitals and nursing facilities and into their own or family members’ homes while recovering from injury or illness. With less honorable motives, insurance companies also pressure hospitals to release patients earlier so that if they continue to receive care, it will be a less costly variety at home.
In response to both these movements, many new home health care agencies have sprung up. You’re increasingly likely to find such an agency in your local area. Most are able to provide care for patients who no longer need high-level care in a hospital but who still require part-time nursing or rehabilitative therapy.
Read Also: Does Medicare Pay For Tdap Shot
Does Medicare Ever Pay For In Home Care
A healthcare provider certified by Medicare must be in order to provide the services covered, and one of the over 11,000 agencies certified by Medicare covering the area is essential for offering the services. This means the Medicare program can pay for home health care at a rate up to 60 days in advance.
How Medicare Pays For Home Health Care
Before you start care, your home health care agency should tell you:
- How much Medicare will pay
- How much youâll pay out-of-pocket if any service or item isnât covered.
Original Medicare will pay the full approved cost of all covered home health care visits. You could be charged 20% of the cost of any medical equipment.
To figure out what your Medicare health plan will pay, youâll need to contact your insurer. All plans are different, so âread those co-pays,â Fassieux says.
Your doctor and home health care agency will review your care at least every 60 days. The type of services you get or equipment you need may change, based on how youâre doing, but Medicare should pay for as long as youâre eligible.
If Medicare denies your request for help or wonât pay for something that you think they should, you can file an appeal.
Recommended Reading: Does Medicare Cover Whooping Cough Vaccine
There Are 2 Ways To Get Medicare Drug Coverage:
1. Medicare drug plans. These plans add drug coverage to Original Medicare, some Medicare Cost Plans, some Private FeeforService plans, and Medical Savings Account plans. You must have
and/or
to join a separate Medicare drug plan.
or other
with drug coverage. You get all of your Part A, Part B, and drug coverage, through these plans. Remember, you must have Part A and Part B to join a Medicare Advantage Plan, and not all of these plans offer drug coverage.
To join a Medicare drug plan, Medicare Advantage Plan, or other Medicare health plan with drug coverage, you must be a United States citizen or lawfully present in the United States.
Visit Medicare.gov/plan-compare to get specific Medicare drug plan and Medicare Advantage Plan costs, and call the plans youre interested in to get more details. For help comparing plan costs, contact your State Health Insurance Assistance Program .
Where To Look For Home Health Care Options
Start by asking your primary care physician for a recommendation, suggests Prather. Theyll likely have good resources and referrals for you. From there, broaden the conversation and ask trusted friends and family members for their recommendations. Finally, look up potential providers online and read other patients reviews.
Recommended Reading: Can I Use Medicare For Dental
Also Check: Is Medicare A Social Security Benefit
Does Medicare Cover Home Instead
Home instead is a private company that provides senior care services to help with a variety of issues. The costs for Home Instead care vary some insurance covers home care, Medicare doesnt.
However, if there is a medical need for care, Medicare will pay for services at home. Medicare wont cover things like live-in caregivers, visiting angels, or other custodial services.
Does Medicare Cover Unskilled Home Care Services
Medicare will not pay for unskilled home care if those are the only services needed. Personal home care services or homemaker services will only be covered if they are part of the skilled services detailed in the care plan. Medicare does not cover around-the-clock home care of any kind or meals delivered to the home.
Don’t Miss: How Many Parts Medicare Has
Original Medicare Does Not Include Prescription Drug Coverage For Self
Generally speaking, Original Medicare, which refers to Parts A and B, does not cover prescription drugs. However, Medicare will usually cover prescription drugs if they are part of a hospital stay, or if they are administered by your healthcare provider.
In addition to this, there is a distinct part of Medicare that specifically covers prescription drugs, and prescription drug coverage is also part of many Medicare Advantage plans. Well take a look at all of the details as well as which options you have.
Recommended Reading: What Is The Monthly Premium For Medicare Plan G
Will Medicare Cover Physical Occupational And Speech Therapy
Medicare will pay for physical therapy when its required to help patients regain movement or strength following an injury or illness. Similarly, it will pay for occupational therapy to restore functionality and speech pathology to help patients regain the ability to communicate.
However, Medicare will only pay for these services if the patients condition is expected to improve in a reasonable, predictable amount of time, and if the patient truly needs a skilled therapist to administer a maintenance program to treat the injury or illness at hand.
Also Check: What Age Do You Apply For Medicare
