What Steps Do I Need To Take To Move From Expanded Medicaid To Medicare
If youre enrolled in expanded Medicaid and youll soon be 65, youll want to familiarize yourself with the health coverage and assistance programs that might be available to you.
Understand that although your assets have not been taken into consideration to determine your eligibility for expanded Medicaid, that will likely change when you turn 65. Every state has an asset limit for full Medicaid eligibility if youre 65 or older, and most states also have asset limits for their MSPs.
But if you do qualify for an MSP particularly the Qualified Medicare Beneficiary program along with Extra Help for prescription drugs you may find that you still qualify for premium-free coverage and very limited out-of-pocket costs.
Youll want to reach out to your states Medicaid office prior to turning 65, to be sure you understand the specifics of 65+ Medicaid and MSP eligibility.
You can also reach out to the Medicare SHIP in your state, to see what resources and assistance are available to you.
You might also want to find a Medicare broker who can help you understand the available Medigap, Part D, and Medicare Advantage plans. Your limited income might make you a good candidate for a low-cost or zero-premium Medicare Advantage plan, leaving you with just the cost of Medicare Part B.
Heres more about choosing between Medigap and Medicare Advantage theres no single solution that works for everyone, so take your time and compare the options available to you.
Is There An Open Enrollment Period For Medicaid
- No. You can enroll in Medicaid at any time during the year. But in many states you have to update your enrollment information every year to make sure you still qualify. If you dont, you can lose your coverage. Jennifer Goldberg, directing attorney at Justice in Aging, says: We see people who dont know they dont have coverage until they get a bill or show up at the pharmacy and the prescription they used to pay $1 for is showing up as $100.
Also Check: How Do I Find Out My Medicare Number
If Youre Eligible For Both Medicaid And Private Insurance
There are a few upsides to being eligible for both Medicaid and private insurance. For services covered by both programs, private insurance will pay first, then Medicaid picks up the difference between your providers allowable charge and private insurance payment, up to your states Medicaid payment limit.
Private health insurance policies usually have copay and deductible requirements. If you qualify for both Medicaid and private insurance, Medicaid may cover these out-of-pocket expenses for you.
Besides collaborating with other payers on a third-party basis, Medicaid may also arrange for private insurance plans and other entities to pay health care providers for services covered by Medicaid. Most Medicaid beneficiaries receive some services through managed care plans that contract with states directly.
When enrolled in Medicare , generally, you wont get coverage through the health insurance marketplace. However, if you already have a marketplace plan but are not enrolled in Medicare, you can retain the marketplace plan even after your Medicare coverage kicks in. However, you can expect to lose the premium tax credits or savings youve been receiving on your marketplace plan.
Read Also: Iowa Dhs Medicaid Income Guidelines
Recommended Reading: Is Prolia Covered By Medicare Part B Or Part D
What Are My Costs With Dual Eligibility
Dual eligibility can limit individual costs for beneficiaries. For those with Medicare, state Medicaid programs will pay for many cost-sharing and out-of-pocket expenses for medical services. For any service you receive, Medicare pays first and covers all eligible costs. Any qualified costs not covered by Medicare will be covered by Medicaid.
What extra benefits and savings do you qualify for?
What Is The Medicare Savings Program
There are four types of Medicare Savings Programs:
- Qualified Medicare Beneficiary Program
- Specified Low-Income Medicare Beneficiary Program
- Qualifying Individual Program
- Qualified Disabled and Working Individuals Program
If you answer yes to these 3 questions, to see if you qualify for assistance in your state:
If you qualify for the QMB program, SLMB, or QI program, you automatically qualify to get Extra Help paying for Medicare drug coverage.
Also Check: How To Call Medicare Gov
Find Cheap Medicare Plans In Your Area
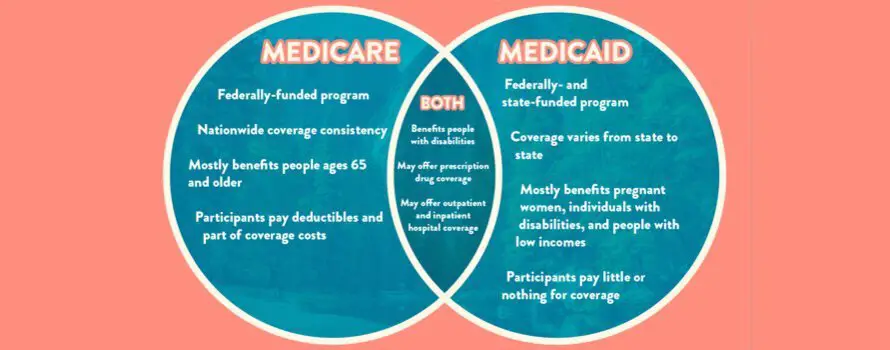
In the United States, there are currently two government-provided health insurance policies that citizens can enroll in: Medicare and Medicaid. While they both provide general health insurance benefits, there are differences in eligibility and coverage that are crucial to identify and be aware of the largest being that Medicare is available to adults who are over 65 years old whereas Medicaid is only available to low-income families.
You May Like: Infertility Clinic That Takes Medicaid
Can I Have A Medicare Advantage Plan With Medicaid
In a growing number of counties, there are Medicare Advantage plans specifically designed for by private insurance companies for Medicare beneficiaries who also qualify for Medicaid. They are called Medicare Advantage Special Needs Plans, or just SNP for short. These unique plans take into account the special needs of low-income seniors in the region they serve and do not have the same cost-sharing requirements as normal Medicare Advantage plansMedicare Advantage , also known as Medicare Part C, are health plans from private insurance companies that are available to people eligible for Original Medicare ..
Some smaller, rural counties may not have SNP plans but will have a local Medicaid plan. You will need to call your local Medicaid office to learn more. Typically Medicaid coverage offers many more benefits than Original Medicare alone.
Also Check: Do I Have To Get Part B Medicare
Dual Eligible Special Needs Plans
In some states, dual eligible beneficiaries may have the option of enrolling in a D-SNP, which is different from a traditional SNP or Special Needs Plan. These plans are specially designed to coordinate the care of dual eligible enrollees. Some plans may also be designed to focus on a specific chronic condition, such as chronic heart failure, diabetes, dementia, or End-Stage Renal Disease. These plans often include access to a network of providers who specialize in treating the specified condition. They may also include a prescription drug benefit that is tailored to the condition.
Income Tiers For Dual Eligibility
Each state sets its own income limits for Medicaid eligibility. Thus, the income tiers for dual eligibility will also vary from state to state.
A reasonable benchmark to use for Medicaid eligibility in 2021 is 138% of the federal poverty level. The federal poverty level is a measure of annual income issued every year by the Department of Health and Human Services to determine eligibility for Medicaid and certain other assistance programs.
For 2021, the federal poverty level for the continental 48 states and the District of Columbia is:
- $12,880 for individuals
- $17,420 for a family of 2
- $21,960 for a family of 3
- $26,500 for a family of 4
- $31,040 for a family of 5
- $35,580 for a family of 6
- $40,120 for a family of 7
- $44,660 for a family of 8
Federal poverty levels differ in Alaska and Hawaii.
Most states use an income of no more than 138% of the federal poverty level in order to be eligible for Medicaid. For example, a family of 3 in Arizona would need a household income of no more than $30,304.80 in order to be eligible for Medicaid.
If a member of that family is also eligible for Medicare because of their age or a disability, they would be dual eligible.
Some states have different income tiers for families and individuals. You can explore a complete online list of state income tiers for Medicaid eligibility.
Also Check: Does Medicare Cover Laser Therapy
You May Like: What Is Centers For Medicare And Medicaid Services
What It Means To Pay Primary/secondary
- The insurance that pays first pays up to the limits of its coverage.
- The one that pays second only pays if there are costs the primary insurer didn’t cover.
- The secondary payer may not pay all the remaining costs.
- If your group health plan or retiree coverage is the secondary payer, you may need to enroll in Medicare Part B before they’ll pay.
If the insurance company doesn’t pay the
promptly , your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should’ve made.
Medicare Advantage And Medicaid
You may be able to enroll in a Medicare Advantage plan when youre on Medicaid. For example, theres a type of Medicare Advantage plan called a Special Needs Plan, or SNP.
Special Needs Plans are geared for people in specific situations. One type of SNP is specifically for dual eligibles people eligible for both Medicare and Medicaid. Please note:
- Medicare SNPs cover the same services and supplies that all Medicare Advantage plans are required to cover.
- Make sure your doctor accepts Medicaid to make sure youre covered. Of course, the doctor must also accept Medicare assignment. Your Medicare Advantage plan should be able to help you find doctors who accept both.
- You need to be enrolled in both Medicare Part A and Part B to qualify for a Medicare Advantage plan. You must also live within the plans service area.
- With any kind of Medicare Advantage plan, in most cases you must continue paying your Medicare Part B premium. However, the Medicaid program might pay your premium.
Also Check: What Is Medicare Ffs Program
Where Can I Find Out More
- Medicaid.gov has links to information explaining the program and to every states Medicaid office.
- Each state has a State Health Insurance Assistance Program that provides counseling and help for Medicare beneficiaries. SHIP counselors can answer some of your Medicaid questions and refer you to local Medicaid officials to help with others.
- The National Council on Aging has a benefits checkup website that has information on Medicare, Medicaid and other programs that help older Americans.
More on Medicare
I Have Been Receiving Health Care Through Medicaid Will I Lose This Coverage When I Become Eligible For Medicare

En español | You will not lose Medicaid eligibility just because you become entitled to Medicare. As long as your income falls under the limits for Medicaid eligibility in your state, you will receive both types of coverage. More than 8 million people have both Medicare and Medicaid.In this situation, Medicare becomes your primary insurance and settles your medical bills first and Medicaid become secondary, paying for services that Medicare doesnt cover and also paying most of your out-of-pocket expenses in Medicare .When you become eligible for Medicare, you must begin receiving your prescription drug coverage from Medicares Part D drug program, not from Medicaid. You will automatically qualify for the federal Extra Help program, which enables you to receive Part D drug coverage without paying premiums or deductibles and paying only low copays for your drugs. But to get this coverage, you still have to choose a Part D drug plan and enroll in it. To ensure that you pick a plan that gives you maximum coverage at the lowest cost, you may want to contact your state health insurance assistance program , which provides personal help from trained counselors on all Medicare and Medicaid issues free of charge. To find the main toll-free number of your SHIP , go to www.shiptacenter.org and select your state. For more information on the Extra Help program, see section 2 of AARPs consumer guide to the Part D program.
Also Check: Does Medicare Part D Cover Sildenafil
Dual Special Needs Insurance
Even better, some insurance companies offer Medicare insurance packages specifically designed to work with your Medicaid dual-eligible status.
How so? If you have certain chronic health conditions , you may be better served by one of the dual special needs Medicare insurance plans that have extra benefits to address those specific conditions.
Recommended Reading: Chiropractors That Accept Medicaid In Louisiana
What Is Medicare Vs Medicaid
Medicare and Medicaid are not the same. Many confuse the benefits of Medicare vs. Medicaid as they are both government-run health insurance programs in the United States. However, Medicare is federal, and Medicaid differs by state.
Medicare benefits are the same across all states and U.S. territories. Typically, Medicare benefits are available to those 65 and over or receiving Social Security Disability benefits under 65. Medicare offers standardized premiums that are consistent for those in the same income bracket.
On the other hand, each states government operates Medicaid. Every state has different qualifications and requirements for enrollment in Medicaid. While there is no age requirement for Medicaid, there is a financial requirement. Your income and resources may not exceed state-specific thresholds to be eligible for Medicaid coverage. Medicaid coverage typically comes at no cost to the beneficiary.
Get A Free Quote
Find the most affordable Medicare Plan in your area
To differentiate the two, with Medi-care, think of care for those 65 and over or those with disabilities. Then, Medic-aid is an aid to those with a low income.
Also Check: What Does Medicare Cover Australia
Seek Help With Medicaid Application And Spend
Medicaid is a very complex government program. Just because a seniors assets exceed the general limits listed above does not mean they are automatically ineligible for coverage. Different states implement slightly different rules and resource limits, and an elder can devise a personalized asset spend-down strategy to meet their states eligibility criteria.
In addition to asset limits, there are many other guidelines for calculating countable income and determining ones medical need for care and assistance. Furthermore, different financial rules apply for married couples. It is recommended to familiarize yourself with these eligibility requirements early on in case you ever need to help an aging loved one apply for Medicaid .
Working with a certified elder law attorney who has extensive knowledge of the unique Medicaid program in your state and is well versed in legal and financial Medicaid planning strategies is crucial. In most cases, handling the application process without any professional assistance can result in a determination of ineligibility and even a costly Medicaid penalty period.
You May Like: How To Switch Providers On Medicaid
Full Benefit Vs Partial Benefit: The Different Levels Of Medicaid Help
As long as youre entitled to Medicare Part A and B, and are eligible for some form of Medicaid benefit, then youre dual-eligible. However, not all dual-eligible benefits are the same.
If you are awarded Medicaid, your benefits will fall into one of the following categories of financial assistance. Medicaid can even pay for your Medicare Part D drug plan in some circumstances. Heres a brief overview of how each program works.
You May Like: How To Qualify For Medicare Disability
Who Is Eligible For Medicaid
You may qualify for free or low-cost care through Medicaid based on income and family size.
In all states, Medicaid provides health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities. In some states the program covers all low-income adults below a certain income level.
- First, find out if your state is expanding Medicaid and learn what that means for you.
- If your state is expanding Medicaid, use this chart to see what you may qualify for based on your income and family size.
Even if you were told you didn’t qualify for Medicaid in the past, you may qualify under the new rules. You can see if you qualify for Medicaid 2 ways:
- Visit your state’s Medicaid website. Use the drop-down menu at the top of this page to pick your state. You can apply right now and find out if you qualify. If you qualify, coverage can begin immediately.
- Fill out an application in the Health Insurance Marketplace. When you finish the application, we’ll tell you which programs you and your family qualify for. If it looks like anyone is eligible for Medicaid and/or CHIP, we’ll let the state agency know so you can enroll.
Unitedhealthcare Connected Benefit Disclaimer
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the Member Handbook. Limitations, copays and restrictions may apply. For more information, call UnitedHealthcare Connected® Member Services or read the UnitedHealthcare Connected® Member Handbook. Benefits, List of Covered Drugs, pharmacy and provider networks and/or copayments may change from time to time throughout the year and on January 1 of each year.
You can get this document for free in other formats, such as large print, braille, or audio. Call , TTY 711, 8 a.m. – 8 p.m., local time, Monday – Friday . The call is free.
You can call Member Services and ask us to make a note in our system that you would like materials in Spanish, large print, braille, or audio now and in the future.
Language Line is available for all in-network providers.
Puede obtener este documento de forma gratuita en otros formatos, como letra de imprenta grande, braille o audio. Llame al , TTY 711, de 08:00 a. m. a 08:00 p. m., hora local, de lunes a viernes correo de voz disponible las 24 horas del día,/los 7 días de la semana). La llamada es gratuita.
Puede llamar a Servicios para Miembros y pedirnos que registremos en nuestro sistema que le gustaría recibir documentos en español, en letra de imprenta grande, braille o audio, ahora y en el futuro.
Los servicios Language Line están disponibles para todos los proveedores dentro de la red.
Don’t Miss: How Do I Bill Medicare For Home Health Services
Get Medicare And Medicaid In One Plan If Youre Dual Eligible
Combine the services of two programs and get personal support.
When I hear the expression get more for less, Im ready to listen. But I also want to trust that the offer is true. When it comes to health insurance, people are often surprised when I tell them you can have both Medicare and Medicaid in one plan at the same time and get more benefits for less cost.
Its a plan for people age 65 or older who are dual eligible, which means theyre eligible for both Medicare and Medicaid. Here are basic definitions of the two programs:
- Medicare is a federal program that helps pay for hospital costs and medical costs .
- Medicaid is a federal and state program for people with limited income and assets. It helps pay for health care, home and community-based services, and nursing home care.
In Minnesota, the plan name for dual eligible enrollees is Minnesota Senior Health Options . Private, not-for-profit health insurance companies or county-based purchasers contract with the State to offer MSHO plans.
