How To Handle Mental Health Billing Denials Rejections And Appeals
Each denial or rejection can happen at one of two places, either at the Clearinghouse level or the insurance company level.
Use your EHR portal to determine if the claim has been denied at the clearinghouse for a missing enrollment, bad subscriber ID, or incorrectly submitted information. .
You can ensure your claim is not denied at the clearinghouse by calling the insurance company and asking if they have the claim on file. If they do, the claim made its way through your clearinghouse. If not, you need to resolve the problem at the clearinghouse level.
If the claim is on file with insurance and is denied, you need to understand the denial reason. Is it for timely filing, terminated coverage, a coordination of benefits issue, unauthorized sessions, needing updated provider information, to just name a few denial reasons?
Go claim by claim, date of service by date of service, and refile the claims as correct with insurance.
If your claims require appeal, speak to a customer support representative about obtaining the necessary forms to file your appeal. Use your reference ID from your eligibility and benefits verification phone call to fight your case.
Fighting denials and rejections is the hardest part of billing. This is yet one more reason why mental health providers choose billing services like TheraThink to help. This is a headache you dont deserve nor are your trained to handle. Consider outsourcing this work to experts.
What Medicare Covers For Inpatient Mental Health Services
Medicare Part A, your hospital insurance, covers mental health services that require your admission to a psychiatric or general hospital. If youre in a psychiatric hospital, youre covered for only up to 190 days of inpatient services over your lifetime. After that, youd need to receive mental health services in a general hospital to be covered.
Your costs will also be substantial: For long hospital stays, they could amount to $10,000 or more in total charges.
What Part Of Medicare Covers Mental Health Care
Medicare Part A covers mental health care in an inpatient setting. Part A mental health care is in a general hospital or a psychiatric hospital only for people with mental health concerns. If you get inpatient care in a psychiatric hospital, Part A will cover up to 190 days in a lifetime. There is no limit to the number of benefit periods you can have for mental health care in a general hospital.
Part A covers your room , meals, nursing care , therapy and treatment, lab tests, medications, and other services and supplies you need. Part A does not cover personal items or a phone or TV in your room.
Medicare Part B covers mental health care on an outpatient basis in these types of settings:
- A doctors or other health care providers office
- A hospital outpatient department
- A community mental health center
And from these types of providers :
- Psychiatrist or another doctor
- Clinical psychologist, social worker, or nurse specialist
- Nurse practitioner
- Physician assistant
Part B helps pay for these outpatient mental health services:
Part D helps cover self-administered prescribed drugs.
Medicare Advantage plans cover all services offered through Original Medicare Part A, Part B, and usually Part D. Copays and coinsurance amounts vary, depending on your plan. Providers and services must be in-network and typically require referrals and prior authorizations before you can receive services.
Also Check: When Can You Have Medicare
Preventive Care And Screening
Medicare makes a limited number of screening services available to beneficiaries at no cost.
- Depression screening: Medicare covers one depression screening per year if the screening is done in a primary care setting that can provide follow-up treatment and referrals. A psychologists office would not be considered a primary care setting in Medicare, but a primary care provider could refer a beneficiary screened for depression to a psychologist for treatment.
- Tobacco use cessation counseling: Medicare will cover up to eight face-to-face visits during a 12-month period for beneficiaries who use tobacco. These visits must be provided by a qualified doctor or other Medicare-recognized practitioner, which includes psychologists.
Medicare Part D Coverage
Your doctor may prescribe medications as part of your treatment. Keep in mind that Original Medicare, Part A and Part B, includes only limited prescription drug coverage, although Part B covers certain prescription drugs you get in an outpatient setting, such as medications you cant give yourself. For most other prescription needs, youll need to enroll in a stand-alone Medicare Part D Prescription Drug Plan if you have Original Medicare.
Another option is to sign up for a Medicare Advantage Prescription Drug plan, which includes both health and drug benefits. These plans must provide at least the same level of coverage as Medicare Part A and Part B, but may include additional coverage, including drug benefits, routine vision and dental, and more. You need to continue paying your Medicare Part B premium along with any plan premium. There are only certain times when you can enroll in a Medicare Advantage plan.
Keep in mind that prescription costs may vary by plan, even for the same medications. One way to minimize your costs is to compare plans and find a Medicare Part D Prescription Drug Plan that covers your prescriptions with low cost-sharing. Remember, costs to consider include not only premiums and copayments or coinsurance, but also deductibles and out-of-pocket maximum limits.
To browse plans in your area, simply enter your zip code where indicated on this page.
To learn about Medicare plans you may be eligible for, you can:
Also Check: Do You Have To Get Medicare When You Turn 65
Other Common Behavioral Health Cpt Codes:
- 90846 Family or couples psychotherapy, without patient present.
- 90847 Family or couples psychotherapy, with patient present.
- 90853 Group Psychotherapy .
- 90839 Psychotherapy for crisis, 60 minutes .
If you are struggling to translate specific aspects of your services to ICD10 diagnosis codes and CPT codes, we are experts at helping specifically and exclusively with our mental health billing and coding service, so consider reaching out.
What Does Cpt Code Modifier 25 Mean
Modifier -25 is used to indicate an Evaluation and Management service on the same day when another service was provided to the patient by the same physician. ASPS believes that providing medically necessary, distinct services on the same date allows physicians to provide efficient, high quality care.
You May Like: What Does Part A Of Medicare Pay For
What Medicare Covers For Outpatient Mental Health Services
Medicare Part B, which pays doctor bills and related health care expenses, covers many mental health services rendered to patients not admitted to a hospital. Covered costs include:
-
A Welcome to Medicare visit that includes a review of your risk factors for depression.
-
One depression screening per year, performed in the office of a primary care doctor or in a primary care clinic that provides follow-up treatment and referrals.
-
Psychiatric evaluation to diagnose mental illness and prepare a care plan.
-
Diagnostic testing.
-
Individual and group psychotherapy or counseling provided by physicians or certain other professionals licensed to do so in your state. Covered providers may include psychiatrists or other doctors, clinical psychologists or social workers, nurse practitioners and physician assistants.
-
Family counseling that aids in your mental health treatment.
-
Medication management and some prescription drugs that are not self-administered.
-
Partial hospitalization, which typically includes many hours of treatment per week without admission to a hospital.
-
Testing to find out if youre getting the services you need and if your current treatment is helping you.
-
An annual wellness visit with a doctor or other provider to discuss any mental health changes.
Who Can Provide Mental Health Services
One of the first regulations of mental health billing is the provider of service. This means that insurance will only cover mental health services if they are provided by a certain type of mental health provider.
For example, Medicare allows the following providers to bill for diagnostic and therapeutic treatment:
- Physicians,
These providers can only bill for mental, psychoneurotic, and personality disorders.
On the other hand, independent psychologists and non-clinical psychologists can only provide diagnostic services.
What this means is that Medicare will only pay an independent psychologist to diagnose a patient with a mental disorder, and not to continue treating the patient with the mental disorder. If you are a physician or psychiatrist, on the other hand, Medicare will pay for you to diagnose and treat the patient with the mental disorder.
Also Check: How To Prevent Medicare Fraud
Types Of Covered Mental Health Services
It’s important to know the types of covered mental health services for your patients who may have varying insurance or medical coverage. For example, some insurance will only cover mental health services by specific providers, such as physicians, psychiatrists, clinical psychologists and clinical social workers. Additionally, some independent mental healthcare providers can only diagnose the patient with a mental disorder because insurance will not cover the actual treatment.
If you are part of a private practice, then physicians’ and psychiatrists’ diagnosis and treatment of the mental disorder will most likely be covered by insurance. These services are often some method of counseling, including a general form of:
Guide To Mental Health Billing: How To Submit Claims
Unfortunately, this is the extremely annoying, hard part. There is no quick guide way of handling this process.
The cheapest option is to learn how to use PracticeMate by OfficeAlly to submit claims, even though it is made for hospitals.
You can try to use a purely software solution to input the data and create the forms. You can reach out to us for help: we do every part of the billing process for you. .
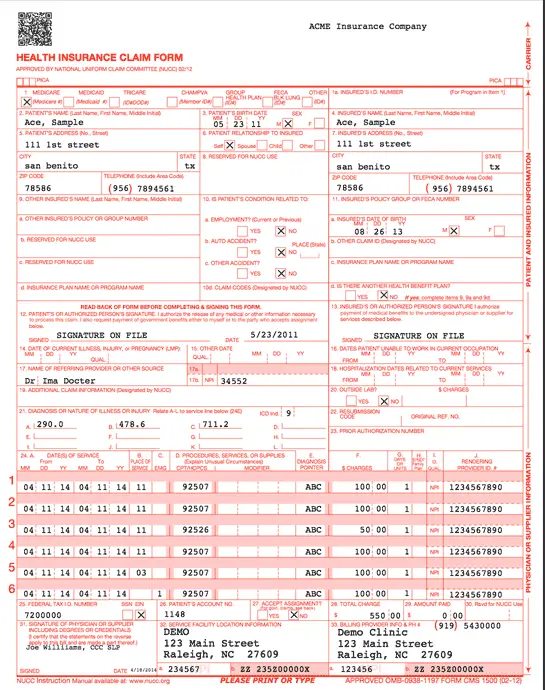
However you end up doing them, you need to transcribe this information onto a CMS1500 form and send it electronically or physically to the insurance company.
Once youve done that..
Read Also: How Old To Get Medicare Part B
A Guide To Medicare Mental Health Billing Codes
Navigating the requirements of Medicare can be a challenge. But heres some good news CPT codes are the same for all payers, whether they are a private insurer or a government program, like Medicare. Once you know the appropriate codes to use for each of the services you provide to clients, that piece of the puzzle is solved.
The rules around timed and untimed codes, however, are more complex. Medicare has strict specifications for calculating how to bill for time increments, and youll want to be sure you follow their guidelines. Heres what you need to know about CPT billing codes for mental health and Medicares 8-Minute Rule.
Does Medicare Cover Mental Health Services
Many or all of the products featured here are from our partners who compensate us. This may influence which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list ofour partnersandhere’s how we make money.
Medicare pays much of the cost of a wide range of mental health services, whether provided on an outpatient basis or for inpatients in a psychiatric or general hospital. But you need to be aware of limits on these benefits, including substantial copays, coinsurance and a lifetime maximum.
Mental health issues are common among older adults: Thirty-one percent of Original Medicare beneficiaries are living with mental illness, according to a July 2020 report by the Commonwealth Fund, a private foundation focused on health care. And in a July 2020 survey by the Kaiser Family Foundation, 46% of Americans ages 65 and up said that pandemic-related stress and worry were detrimental to their mental health.
Recommended Reading: How Much Does Medicare Cover For Knee Replacement
Billing Coding And Coverage
| Annual depression screening 15 mins |
- Includes patient form completion, recording by medical assistant and physician discussion with patient
- Coinsurance and deductible waived
- Furnished by Psychiatrist or Psychologist only with clinical staff-assisted depression care supports in place
- Primary care settings only:
- 11 , 19 or 22 or 71
Alcohol Screening and Behavioral Counseling
| CPT Code | |
|---|---|
| Annual alcohol misuse screening 15 minutes | |
| G0443 | Face-to-face behavioral counseling for alcohol misuse, 15 minutes |
- Competent women older than 65
- Competent men 65 years and younger
- If screening positive, then up to four brief face-to-face counseling sessions
- Must have at least three of the following dependence
- Withdrawal symptoms, impaired control, tolerance, acquisition preoccupation, unsuccessful efforts to quit, continue use despite consequences, can sustain social, occupational or recreational)
| PDE with medical services add medical assessment |
Psychotherapy and Evaluation and Management
Medicaid Billing To Remain Available For Licensed Professional Counselors
UPDATE: The Louisiana Department of Health said Monday it received the requested guidance from the Centers for Medicare and Medicare Services that it was seeking. Based on the feedback of CMS, LDH says its able to allow Federally Qualified Health Centers to bill for services provided by Licensed Professional Counselors. The state says it plans to notify the Medicaid health plans so they can resume working with LPCs in the FQHCs.
BATON ROUGE Theres been a change to Medicaid and it could be affecting your school-aged children.
Earlier this year, the Louisiana Department of Health says it was made aware of a change effective July 1, 2019, affecting Licensed Professional Counselors working for a Federally Qualified Health Center . The state is citing a federal requirement ) from 2014 and says its waiting on guidance about what to do next.
LPCs have been working in schools state-wide for years. They were brought in to help fill a need and assist counselors already in schools. Certain parishes do not employ guidance counselors and fully rely on non-profit agencies to provide behavioral health services. Some schools dont have enough counselors to fill the need.
LPCs working for FQHCs have been able to bill Medicaid and receive reimbursement for their services but not anymore. With this change, dozens of LPCs and thousands of students seeking counseling services at school are left wondering whats next.
Trending News
Also Check: Does Medicare Part D Cover Shingrix
Read Also: Does Medicare Cover Home Health Care Costs
What Original Medicare Doesnt Cover
Your health care provider may recommend you receive services more frequently than Medicare covers, or services that Medicare doesnt cover, and you may end up paying some or all of these costs. Ask your provider why they are recommending such services and whether Medicare will cover them.
You will have to pay for private duty nursing or a private room, unless its medically necessary. Other limits may apply.
Does Medicare Pay For Therapy Services
As part of Medicares mental health care benefits, therapy, or counseling is typically covered under Part B as an outpatient service with Original Medicare. MA plans provide the same benefits as Part B does. Therapy generally can be for an individual or a group. Family therapy is covered if it is to support the Medicare beneficiarys mental health treatment goals.
As with all mental health services, you must receive therapy from a provider that accepts assignment for Original Medicare or is in-network with your MA plan. The provider must be licensed in your state. Copay or coinsurance and deductibles apply.
In 2022, for instance, for outpatient mental health care through a UnitedHealthcare MA HMO plan, you pay $25 copay for each Medicare-covered individual therapy session and $15 copay for group therapy. For a similar type of plan with Humana, you pay a $20 copay for mental health services received from a specialist, an outpatient hospital, or intensive therapy that is part of the day program in a hospital. For a similar plan with BCBS/Anthem, you pay $40 for each Medicare-covered visit, group, or individual.
Your copays vary depending on your MA plan. To find out what your out-of-pocket costs will be and precisely what your plan will cover based on Medicare rules, talk with your plans administrator, review your EOC, and talk with your healthcare provider. Allow for the time it takes to get a referral and prior authorization.
You May Like: How To Apply For Medicare In Michigan Online
Medicare Outpatient Mental Health Services
Medicare Part B covers outpatient mental health services, such as care youd get in a health clinic or doctors office. Youll generally pay 20% of the Medicare-approved cost for outpatient care delivered by providers that accept Medicare assignment.
Medicare covers the following types of psychotherapy :
- Psychiatric assessment
- Family counseling, when the primary goal is to treat your condition
- Alcohol misuse counseling, up to four sessions
You may need to meet other criteria to be eligible for therapy coverage, and the doctor, psychologist, or other health-care professional must accept Medicare assignment. Medicare doesnt cover certain types of therapy, such as pastoral counseling or marriage counseling.
If you need more structured or frequent treatment, Medicare Part B also covers partial hospitalization programs, which are outpatient mental health programs where treatment is provided throughout the day and doesnt require an overnight, inpatient stay. The programs are usually run through a community mental health center or a hospitals outpatient department. Services may include therapy with a mental health professional, diagnostic services, and occupational therapy . These programs dont cover meals or transportation to the facility.
Mental Health Billing: 10 Common Questions And Answers
If you are a mental health professional working in private or group practice, you have your work cut out for you. Serving your clients well, and finding the time to handle all of the administrative tasks of your practice can become quite stressful.
Mental health professionals have billing needs that differ from other medical professionals. It is commonplace for many types of medical doctors to have large office staffs, with many administrators handling the billing and claims.
However, many mental health practices run on much thinner financial margins than their medical counterparts, and therefore the burden of mental health billing often falls on the counselor, or a small office staff. Perhaps because of this, sadly, many practices collect less than 85% of the money they are owed from insurance companies.
You can do much better than this! With some perseverance, and a strong working knowledge of billing, you can expect to collect 96%, to as high as 99% of your claims. Here are some quick questions and answers that will save you time and money.
1. Is the reimbursement pay from the insurance company worth it?
Being a mental health professional can be difficult, and you want to be rewarded appropriately for your service. Is it worth it to bother with reimbursements from insurance companies? Should counselors just stick to a cash-only approach?
Answer:
2. Can I bill the same client for multiple sessions in one day?
3. How long do insurance payouts normally take?
Answer:
Don’t Miss: How To Apply For Medicare Without Claiming Social Security
