Find A Home Health Care Provider
You can search for a provider by using the online home health care provider tool at Medicare.gov. Just enter your zip code and the tool will give you a list of home health care providers in your area. You can also ask your doctor, hospital social worker or discharge administrator to arrange for a home health provider in the event you need home care after a hospital stay.
Dont let an injury or illness prevent you from getting the help you may need. Talk to your doctor and ask if you qualify for home health care.
When Is Physical Occupational Or Speech Therapy Covered By Medicare
Physical therapy will be covered by Medicare when it will help the client regain strength or movement after an illness or injury. The same holds true for occupational therapy where the goal is to restore functionality, and for speech therapy to help patients relearn how to communicate.
The services will only be covered if they are expected to result in an improvement within a predictable period of time. Additionally, the frequency, duration, and number of services must be reasonable and provided by a qualified therapist. To be eligible for the services your condition must either:
- Be expected to improve,
- Require a maintenance program from a skilled therapist, or
- Require a skilled therapist for maintenance.
Professional therapists will restore or improve the clients ability to perform routine everyday tasks, speak or even walk following an illness or injury. They may also help prevent a condition from worsening and will only be covered if the services specifically, safely and effectively treat the clients condition.
When Does Medicare Not Cover In
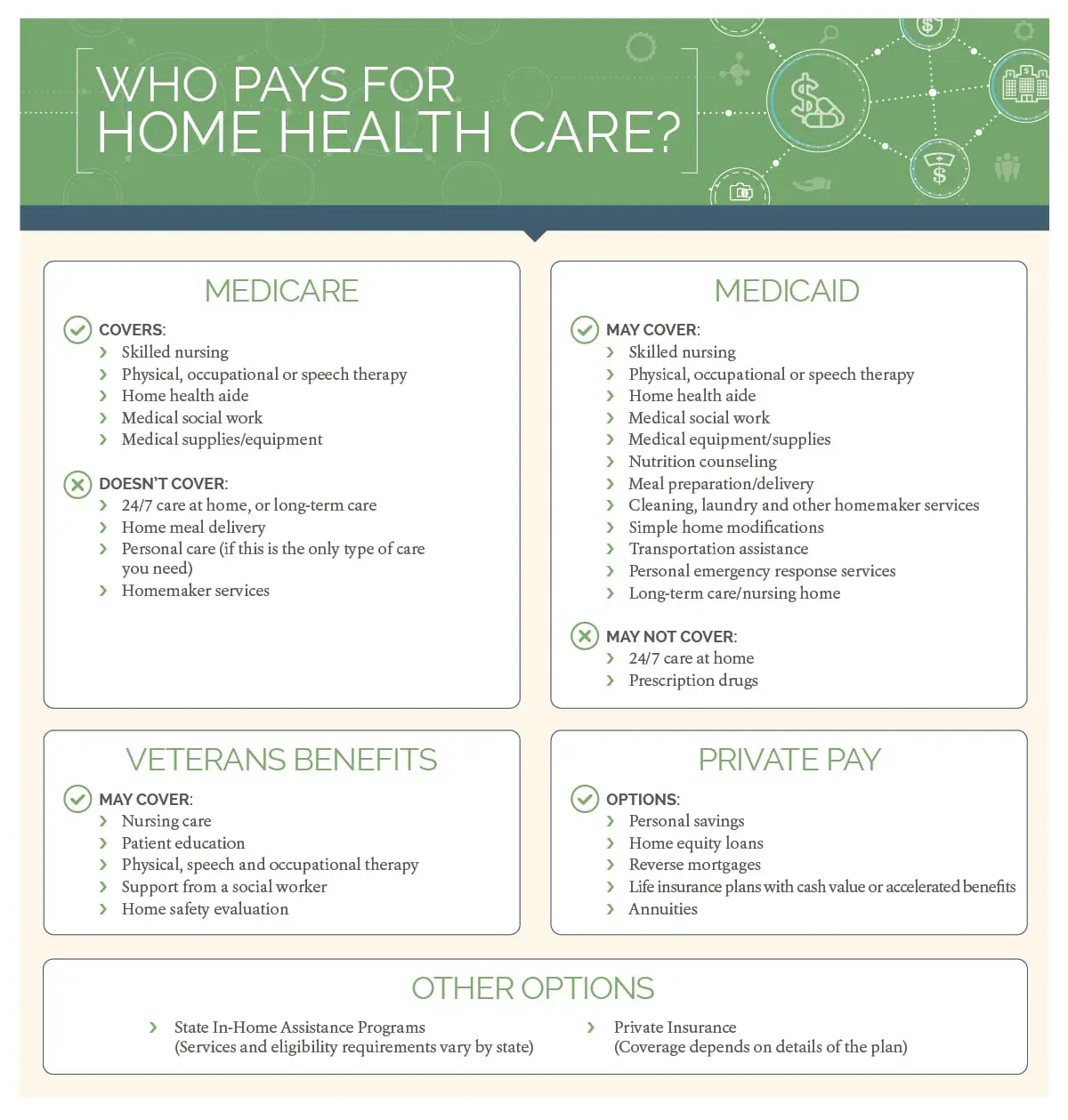
In most cases, Medicare doesnt cover these types of in-home health care.
- Home health aides, when the only care you need is custodial. That means you need help bathing, dressing, and/or using the bathroom.
- Round-the-clock care
- Homemaker services, like cleaning, laundry, and shopping. If these services arent in your care plan, and theyre the only care you need, theyre generally not covered.
Its important to know that just because your doctor might recommend home health care, Medicare doesnt automatically cover it. It depends on your situation.
Read Also: Does Medicare Cover Aba Therapy
Your Home Health Plan Of Care Must Also Be Regularly Reviewed By Your Doctor
At least once every 60 days, your doctor must make an assessment of your progress toward health goals. Any changes to your health must be reported by the visiting nurse.
These routine measures ensure medical services received at home maintain or slow the decline of an illness or injury over a reasonable period of time, typically 60 days.
But what happens when your home medical needs are more than just short-term or part-time?
What Is A Medicare Home Health Doctor Care Plan
The doctors plan of care tells the Medicare home health nursing agency which services you need in order for your health condition to improve. Together the doctor and the Medicare home health nursing agency decide:
The services you require
Which type of skilled professional will work with you
How often you will receive these services
The types of equipment needed Any special foods
The outcomes expected from these treatments
You can feel confident knowing that both your doctor and the Medicare skilled nursing agency professionals will be working with you. They will continue to communicate regularly to review your plan of care & your doctor will make changes as needed to enable your recovery.
If you or a loved one are in need of information related to your Medicare Home Health Benefits, Contact Us today or call 561-989-0441 for your free consultation.
You May Like: Do Most Doctors Accept Medicare
Services Medicare Doesnt Cover
Though Medicare can be a huge help in covering home health care, it doesnt cover everything. Here are some of the services that arent included as part of these benefits:
- Around-the-clock care
- Personal care services if you dont also require skilled medical care or therapy
- Homemaking services if you dont also require skilled medical care or therapy.
Before your care starts, your Medicare-certified home health agency should present you with a breakdown of the charges and what Medicare will pay. This notice should also include how much youll be required to pay out of pocket.
Home Health Benefit Widely Misunderstood
Medicare rules state that if a beneficiary is considered homebound and requires skilled nursing, physical therapy, or speech language pathology services, he or she also can qualify for dependent services, including home health aides. Medicare law authorizes up to 28 to 35 hours per week of home health aide and nursing services combined, as well as therapies and medical social services. If a person continues to meet these criteria, there is no limit to the duration of services. In other words, contrary to what people are often told by providers, Medicare Advantage plans, 1-800-MEDICARE, and even the Centers for Medicare and Medicaid Services , home health coverage is not just a short-termbenefit to help people recover from an acute event.
The Center for Medicare Advocacy hears regularly from people who meet Medicare coverage criteria but are unable to access home health benefits or denied the appropriate amount of care. The legal standards that define who can obtain coverage and what services are available are often narrowly construed and misunderstood by providers and Medicare adjudicators.1 This is increasingly true for home health aide services, although help with activities of daily living is often what older and disabled people need to remain healthy and safe at home.
Recommended Reading: What Is Bernie Sanders Plan For Medicare For All
What Home Health Care Isnt Covered By Medicare
Medicare doesnât cover personal errands that arenât directly related to your care. These services include:
- Grocery shopping
- Cleaning the house
Medicare also doesnât cover many long-lasting supplies. Home health care agencies usually donât use these types of items for your treatment. These supplies include:
- Motorized stairway elevators
Medicare doesnât cover prescription drugs as part of home care.
Medicare Plans That May Assist With Nursing Home Expenses
Although Medicare would generally not cover health services that are not regarded as medically necessary, there are several aspects of Nursing health facilities services that are very important to the prognosis of both the elderly and individuals with disabilities.
If Medicare approves this service to be worth it, the individual might receive conditional healthcare coverage under the following categories.
Medicare Part A:
The Medicare Part A plan is known widely for its coverage of medical expenses within the Medicare network. However, it can also extend to Special Nursing Facilities in times when Medicare has approved the funding of Nursing Facilities.
Although Medicare Part A would only offer short coverage, this coverage might even include medications and drug descriptions depending on the persons plan.
Medicare Part B:
Usually, Medicare Part B mostly covers healthcare services outside the Medicare network. Hence, it doesnt offer healthcare coverage for nursing facilities.
However, there are certain special cases where Medicare Part B plans would provide the funds for Nursing home services. Nevertheless, this is very rare and depends on specific health insurance companies.
Medicare Part C:
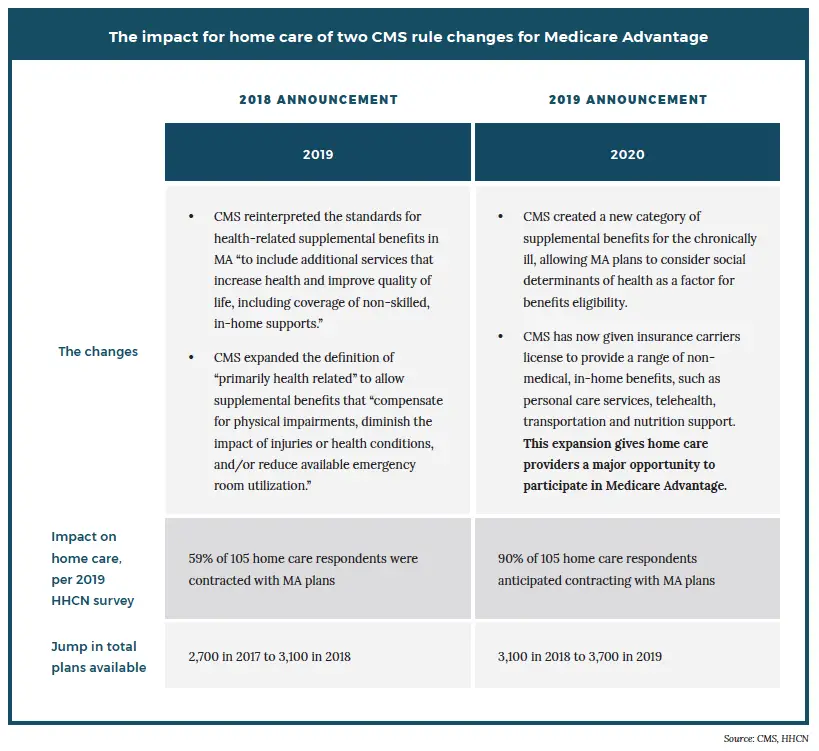
Medicare Part C, also called the Medicare Advantage plan, is a government-sponsored private plan that offers coverage to additional health benefits that are not found in either of the Medicare Part A or Part B plans.
Medicare Part D:
Medicare Supplement:
Also Check: How Long Does Medicare Pay For Home Health Care
When Medicare Will Cover Home Health Care
For your home heath care to be covered by Medicare, your situation must meet this list of requirements.
- Your doctor must have prescribed home health care for you.
- You must require part-time skilled nursing care or physical, speech, or occupational therapy.
- The home health care must be provided by a Medicare-approved agency.
- You must be confined to your home by an injury, illness, or other medical condition.
- Your doctor must help set up a care plan in cooperation with the home health care agency.
Medicare sometimes used to also require that your condition be expected to improve with home health care, but a recent change allows you to qualify for home health care just to maintain your condition or to slow deterioration of your condition.
If you require full-time nursing care, Medicare will not approve home health care, but it could cover a skilled nursing facility. For more information, see our article on Medicare coverage for skilled nursing care.
Recommended Reading: Does Medicare Cover Rotator Cuff Surgery
Home Health Services Patients Sue Hhs Secretary Over Medicare Policy
A lawsuit filed against Health and Human Services Secretary Xavier Becerra alleges the policies maintained by his department are restricting access to home health aide services for Medicare beneficiaries who are disabled or live with chronic conditions.
The suit was filed by a group of Medicare beneficiaries across multiple states as well as some health care advocacy groups earlier this month.
The plaintiffs alleged that Becerra has adopted policies and practices that impede and restrict the availability and accessibility of Medicare-covered home health aide services for eligible beneficiaries with chronic, disabling conditions.
Under Medicare coverage, beneficiaries are eligible to receive up to 28 hours of home health services a week or even 35 hours a week in certain circumstances. While the eligibility to receive these services has remained unchanged, the lawsuit alleges that the actual services that are made available to beneficiaries have continued to drop over the years.
One of the plaintiffs, Catherine Johnson of Missouri, suffers from multiple sclerosis and complete quadriplegia. In January 2021, a Medicare-certified home health agency terminated the services it was providing to Johnson.
Although this decision was later deemed improper, Johnson has since experienced erratic and unpredictable care, at one point being admitted to a hospital where her condition is alleged to have deteriorated further.
Also Check: What Is The Difference In Medicare And Medicare Advantage
How Do You Qualify For Medicare Home Health Care
Medicare has rules for whose home health care it can cover. You must meet all of the following standards for how to get home health care under Medicare.
You have a doctorâs approval. A doctor needs to be managing your care. They need to sign a form saying that your home health care is medically necessary. The doctor creates and checks your home health care plan, which could include:
- Which services you need
- Your treatment schedule
- Your health goal
Youâll need to meet with the doctor at least 90 days before your home health care treatment begins or 30 days afterward. Your doctor must meet with you at least every 60 days to review your care plan. They can decide whether to renew or end your treatment after every 60-day period.
You are homebound. A doctor can approve you for home health care if you are homebound. This means:
- You need another personâs help to leave the house, such as helping to carry your wheelchair
- Your health could get worse if you spend time outside your home
- You leave your home for adult day care or religious services
- Leaving your home takes a lot of effort
You need at least one type of skilled care. Your care plan needs to include at least one type of skilled treatment in order for Medicare to cover it. For example, you might need physical therapy to regain movement after an injury.
You may need more home health care than what Medicare will cover. In this case, Medicare may be able to pay for short-term stays in a nursing home or hospital.
What Types Of In
If your situation meets Medicare criteria, Medicare may cover in-home health care such as:
- Skilled nursing care
- Part-time home health aides
- Medical social services
Medicare benefits might also cover:
- Durable medical equipment
- Medical supplies
- Injectable osteoporosis drugs
If you qualify for home health care under Medicare, you generally dont have to pay any coinsurance or copayment. If you need durable medical equipment, youll typically pay 20% of the Medicare-approved amount as coinsurance. Read more about Medicare and durable medical equipment.
Read Also: Do You Automatically Get Medicare When You Turn 65
Medicare Supplement Plans Or Medigap
If you have original Medicare , you may be able to purchase a Medicare supplement plan, also called Medigap.
Some Medigap plans pay for the coinsurance costs for Part B, which may help you pay for home health services. However, these plans dont offer expanded home health service coverage.
Some people choose to purchase separate long-term care insurance, which isnt a part of Medicare. These policies may help to cover more home health care services and for longer time periods than Medicare. However, the policies vary and do represent an extra cost to seniors.
Does Medicare Cover In
According to the U.S. Department of Health and Human Services, someone turning 65 today has about a 70% chance of needing some type of long-term care in the future. And withover 75% of Americans 50 and older saying theyd like to live in their current community as long as possible, more and more families are beginning to consider in-home care for their aging loved ones.
In-home care can be an appealing option for many seniors and their families because it enables them to age in place while still receiving the care and support they need. But, in-home care can be expensive. As of 2020, the national average cost of in-home care ranges from $25-$26 per hour. The expense can add up quickly, and many families seek outside sources of financial assistance to pay for in-home care.
In many cases, the first place seniors turn is Medicare. While Medicare covers in-home care services in some circumstances, it doesnt offer assistance for everyone and all types of home care. If youre unsure if Medicare will cover in-home care for yourself or a loved one, this guide is for you.
Does Medicare Cover In-Home Care?
You May Like: What Is The Age Of Medicare
Home Health Care Covered By Medicare
If you are eligible for home healthcare, Medicare will cover the cost of the following services:
- Skilled nursing care: Medicare will pay for skilled nursing care when your condition requires it. However, Medicare only covers it up to a maximum of 8 hours per day.
- Physical therapy and occupational therapy: If your condition is deemed to require the skills of a licensed physical therapist or occupational therapist, Medicare will cover the cost of these services. You will also be covered for speech or language therapy if your doctor has deemed it effective and necessary for your condition.
- Part-time or intermittent home health aide care: Medicare will cover home health aide care such as help dressing and bathing. However, these services are only covered if you are getting other skilled care such as nursing care or physical therapy.
- Medical supplies and equipment: Under your Medicare part B, some medical equipment may be covered, including wheelchairs, wound dressings, walkers, nebulizer equipment, and blood sugar monitors, among others.
- Medical social services: Medicare also covers the cost of receiving counseling or social work services at home.
Does Medicare Part A Cover 100 Percent
Medicare Part A is hospital insurance. Part A covers inpatient hospital care, limited time in a skilled nursing care facility, limited home health care services, and hospice care. Medicare will then pay 100% of your costs for up to 60 days in a hospital or up to 20 days in a skilled nursing facility.
You May Like: Does Medicare Cover Bone Marrow Transplant
Who May Be Eligible For Home Health Aides Under Medicare
Medicare has coverage rules about home health aides. Here are some of them :
You must be under a doctorâs care with a care plan that your doctor reviews regularly.
You must be homebound, as certified by your doctor. Medicare considers homebound to mean you canât leave your home without help, or your health condition generally requires you to stay at home. You can still qualify as âhomebound if you go to religious services, doctor appointments, or adult day care.
Your doctor must certify that you need at least one of these:
- Intermittent skilled nursing care
- Physical therapy, speech-language pathology, or continued occupational therapy services. You may want to check with Medicare about the specific rules about these types of therapy and how much is covered.
What Is The Eligibility For Medicare Advantage Plans
Most people arent eligible for supplemental Medicare plans, or Medicare Part C, unless theyve already been approved for traditional Medicare. Also, applicants must be under the care of a physician and receive services that are regularly reviewed by the doctor. Those applying for supplemental Medicare must also be receiving physical or occupational therapy and be certified as homebound.
Eligibility for a Medicare Advantage Plan depends on the requirements for each plan. Coverage varies according to the provider and the state. Even within a state, different areas may have different types of eligibility requirements.
For questions, call Medicare at 1-800-MEDICARE or TTY at 1-877-486-2048.
Don’t Miss: How To Lower Medicare Premiums
Does Medicare Pay For Home Health Care
There is an important distinction between medically necessary home health care and personal care services provided by an unskilled caregiver. Understanding the difference between these two levels of care is key to determining who is eligible for Medicare-covered in-home services. For more information on this topic, read The Difference Between Home Health Care and Non-Medical Home Care Services.
Only home health care services prescribed by a doctor and provided by skilled caregivers are covered by Medicare, but patients must meet specific eligibility requirements.
Medicare Nursing Home Coverage 2022

Health insurance policies over the years have made progress in the provision of quality healthcare around the world. With healthcare policies, individuals can have access to better quality healthcare. However, there are, of course, various factors involved in getting these healthcare insurance policies.
One of the major progress made in the healthcare sector is making a lot of special healthcare plans available for individuals that need assistance, especially plans like Medicare plans.
Medicare gives health insurance access to adult individuals that are 65 years old or older as well as qualified individuals with cases of disability. These sets of individuals have certain challenges that would normally prevent them from getting the most suitable health insurance plans normally.
Elders above the age of 65 are more susceptible to diseases because of old age hence theyd require closer medical attention and treatments.
Also, most of the seniors in question would have retired from employment and would be living on pensions or whatever source of income that would not allow for much financial responsibility. And as a result, they might not be able to afford the healthcare services required for their health.
People generally need so many health services to ensure that they enjoy the maximum standard of healthcare. So, in this article, we will be talking about the nursing home coverage you can get with Medicare health insurance policies.
Recommended Reading: What Is Medicare For All
