What Is A Copay Deductible
Typical copay stage. Your deductible is the amount of money you must spend on covered drugs before your Medicare drug coverage starts paying its share of costs. In the deductible stage, youre responsible for the full cost of your prescription drugs. Some Medicare prescription drug plans have a $0 deductible.
Aarp Research Finds Brand
More than 2.6 million Medicare Part D enrollees took the blood thinner Eliquis in 2020 at a cost of nearly $10 billion to the program. AARP researchers also found that the prices of 75 of the 100 brand-name drugs Medicare spends the most on were raised in January. Eliquis list price rose 6 percent.
Brand-name drug prices have grown faster than general inflation for over a decade, causing an increasing number of patients to go without necessary medications, AARP researchers say in a new blog post. Medicare beneficiaries, who have a median annual income of just under $30,000, take an average of four to five prescription drugs every month, the report says, and public opinion surveys consistently have found that many skip doses or dont refill their prescriptions because of the cost.
Youre definitely looking at a meaningful impact on Medicare Part D spending, both on the program and the beneficiaries, says Leigh Purvis, AARP director of health care costs and access. Its indicative of the larger problem where weve left drug companies free to continue engaging in the type of pricing behavior thats been a problem for so long. AARPs new data shows that in January 2022, the average list price increase for the 75 top brand-name drugs was 5.2 percent. Price hikes ranged from 2 percent to 7.9 percent, and the prices of more than half increased by 5 percent or more.
Prescription Drug Coverage Key In Multiple Myeloma Therapy
A study shows prescription drug coverage leads to better survival among Medicare beneficiaries with multiple myeloma.
Multiple myeloma patients who had prescription drug coverage were more likely to receive active myeloma care and less likely to use parenteral treatments or other classic cytotoxic agents to treat their disease, according to the results of a study published in The Journal of Clinical Oncology.
As most patients with myeloma in the United States are covered by Medicare, our results have important implications both for the clinicians who care for these patients and for healthcare policy that tackles coverage or oral and parenteral anticancer therapy, wrote Adam J. Olszewski, MD, of the Warren Alpert Medical School of Brown University, Richmond, Rhode Island, and colleagues.
In the setting of myeloma, a cancer that can be treated using highly efficacious oral agents in addition to-or instead of-parenteral chemotherapy, patients with outpatient prescription drug coverage are more likely to receive active care and have longer survival than those without prescription drug coverage, the researchers wrote. Providing more equitable access to oral and parenteral chemotherapy options may thus enhance outcomes in myeloma and, hypothetically, other cancers that are treatable with oral targeted agents.
Four in 10 enrollees who did not have prescription coverage at diagnosis enrolled after the myeloma diagnosis.
Related Content:
Also Check: How Does Medicare For All Work
Patients With Commercial Insurance
The BMS Oncology Co-Pay Assistance Program helps commercially insured patients who have been prescribed select BMS medications with out-of-pocket deductibles, co-pays, or co-insurance requirements. Eligible patients may pay as little as $0 per one-month supply, up to a maximum of $15,000 per calendar year.
For more information, please call BMS Access Support® at , 8 am to 8 pm ET, Monday Friday.
Restrictions apply. Please for full Terms and Conditions, including complete eligibility requirements.
Patients Without Prescription Drug Coverage Or Who Are Underinsured
- For patients without prescription drug insurance or for patients who are underinsured, BMS Access Support can make a referral to independent charitable foundations that may be able to help.
- It is important to note that charitable foundations are independent from Bristol-Myers Squibb Company. Each foundation has its own eligibility criteria and evaluation process. Bristol Myers Squibb cannot guarantee that a patient will receive assistance.
The accurate completion of reimbursement- or coverage-related documentation is the responsibility of the healthcare provider and patient. Bristol Myers Squibb and its agents make no guarantee regarding reimbursement for any service or item.
Also Check: Does Medicare Pay For Tdap Vaccine
Have Questions About Our Program Or Possible Financial Support
If you have questions about coverage for a prescribed BMS medication, BMS Access Support may be able to help. Patients and their healthcare provider can complete an enrollment form to learn about programs that may be of assistance. Visit our website or contact BMS Access Support to learn more.
Call Bristol Myers Squibb Access Support at, 8 AM to 8 PM ET, MondayFriday
Visit www.BMSAccessSupport.com
The accurate completion of reimbursement- or coverage-related documentation is the responsibility of the healthcare provider and the patient. Bristol Myers Squibb and its agents make no guarantee regarding reimbursement for any service or item.
What Drug Company Makes Revlimid
Revlimid, also known as lenalidomide, is an oral cancer drug that is used for the treatment of multiple myeloma. It is part of a class of drugs called immunomodulatory drugs , which work against cancer cells partly by supporting the function of the immune system. Revlimid is manufactured by Celgene.
Recommended Reading: Is Enbrel Covered By Medicare
Bms Access Support Can Provide Patient Access And Reimbursement Assistance
Bristol Myers Squibb is committed to helping patients gain access to their prescribed BMS medications. Thats why we offer BMS Access Support. BMS Access Support provides resources to help patients understand their insurance coverage. In addition, we can share information on sources of financial support, including co-pay assistance for eligible commercially insured patients.
Does Medicare Cover Out
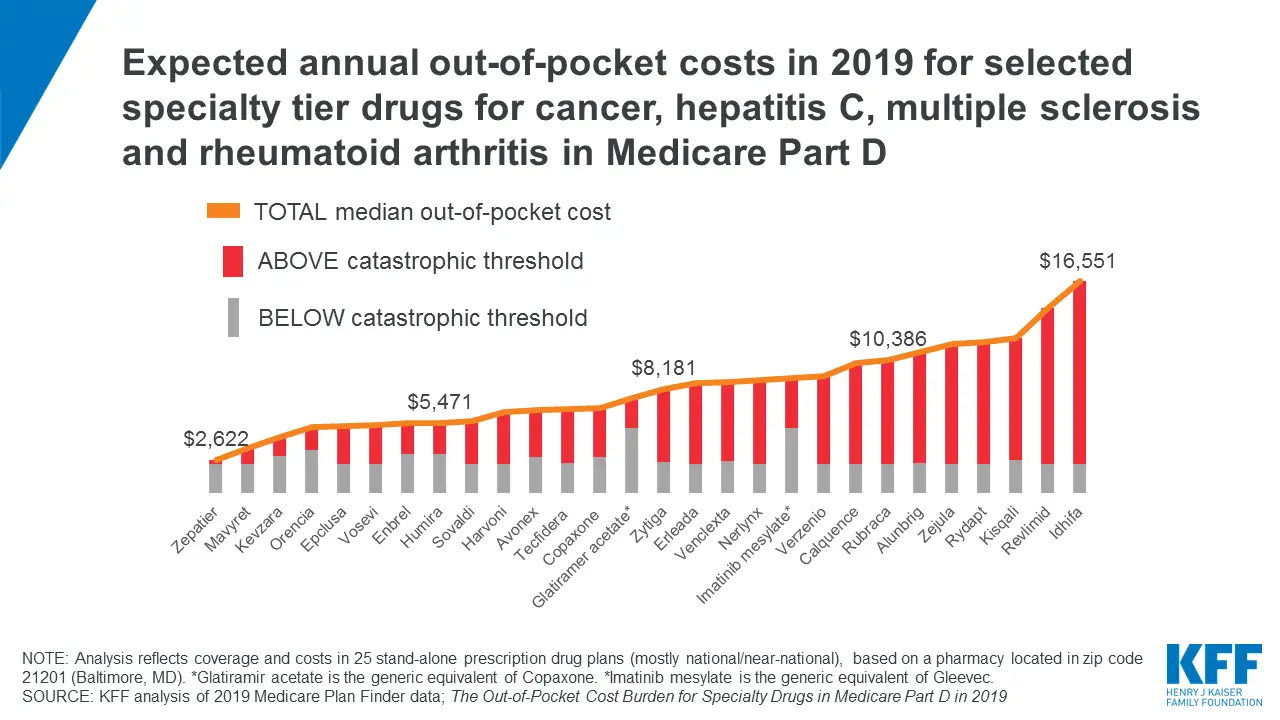
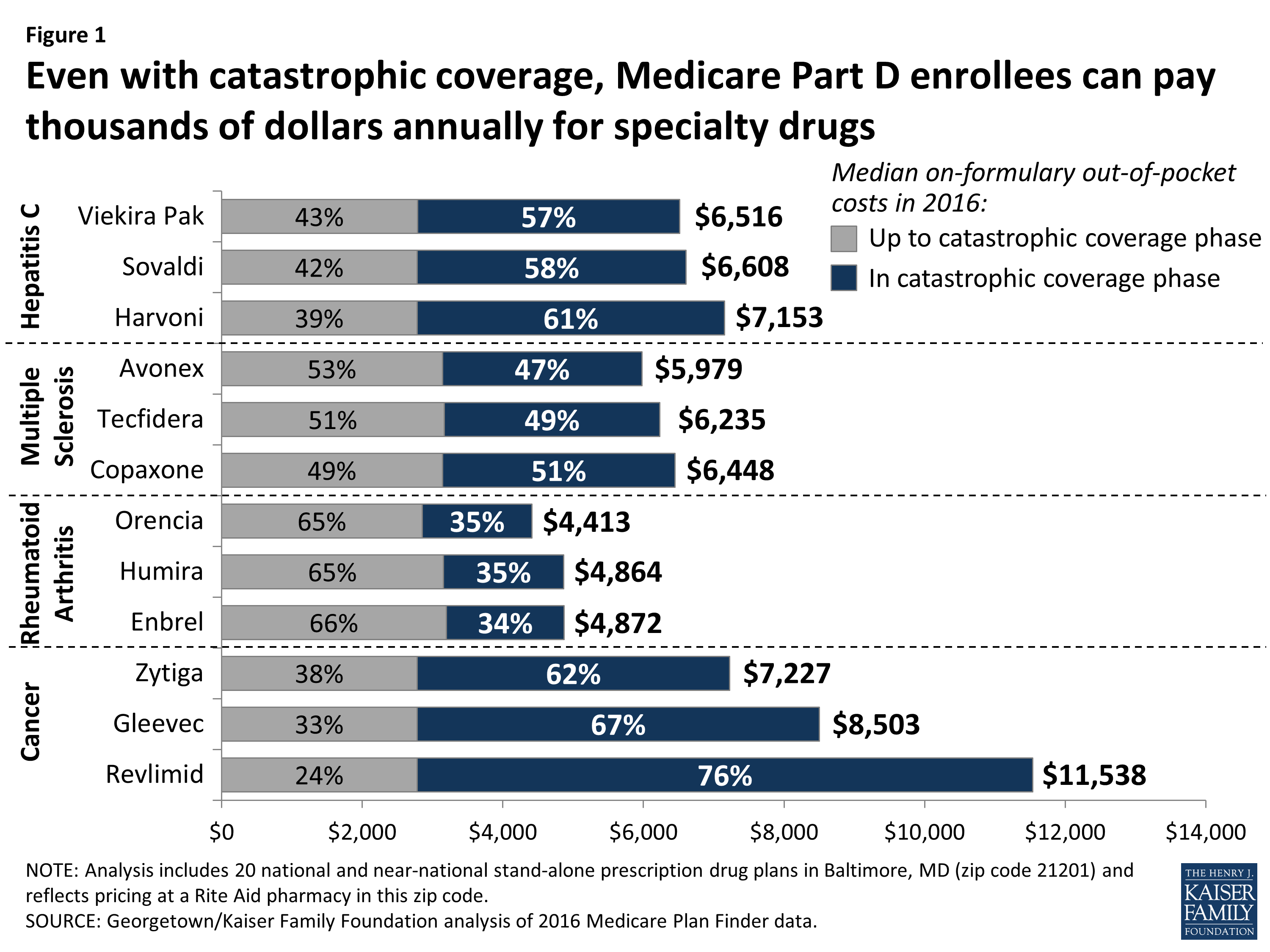
Although Part D offers catastrophic coverage for high drug costs, beneficiaries can still face substantial out-of-pocket costs for expensive medications, including many drugs for cancer, hepatitis C, multiple sclerosis, and rheumatoid arthritis, because there is no hard cap on spending in the Part D benefit. Part D enrollees who need specialty tier drugs that are not covered by their plan could be exposed to substantial costswhich would likely mean not filling a prescription for the off-formulary drug and instead taking a therapeutic substitute.
Also Check: Does Medicare Pay For Stem Cell Knee Replacement
Revlimid Coupons Copay Cards And Rebates
Revlimid offers may be in the form of a printable coupon, rebate, savings or copay card, trial offer, or free samples.Some offers may be printed right from a website, others require registration, completing a questionnaire,or obtaining a sample from the doctor’s office.
Revlimid BMS Oncology Co-Pay Assistance Program: Eligible commercially insured patients may pay no more than $10 per 30-day supply with savings of up to $15,000 per calendar year for additional information contact the program at 800-861-0048.
- Applies to:
Applicable drugs:
More information please phone:800-675-8416Visit Website
Re: Humana Charge For Pomalyst
by Multibilly on Fri Apr 29, 2016 7:19 pm
by Castaway on Sat Apr 30, 2016 1:34 am
by Castaway on Tue May 03, 2016 12:07 pm
by NStewart on Tue May 03, 2016 1:35 pm
by Castaway on Tue May 03, 2016 11:49 pm
Don’t Miss: Do Any Medicare Supplement Plans Cover Dental
Patient Assistance Charities To The Rescue
A lot of Americans with insurance have to turn to charity to pay their drug copays. Some of the charities are affiliated with the drug companies and some are independent. Eight of the largest independent charities paid out over $1 billion in 2017, according to a study published in the Journal of American Medical Association.
Paying patient copays is good business for the drug companies, said David Mitchell. A cancer survivor himself, Mitchell founded the advocacy group Patients For Affordable Drugs after he had to pay for Revlimid.
The pharmaceutical company makes available an amount of money to pay a small portion of the total price, 10 or 20% lets say, Mitchell said, and then bills the insurer or the government the balance of 80 or 90%.
Those grants are a lifeline to patients. But they also shield consumers from price hikes, so a company can charge whatever it wants.
It can jack up the price to more than cover that little that its having to contribute, Mitchell said, because it collects so much on the balance of the payments, and a lot of this is coming right from Medicare.
Internal documents from the drug company Teva show it anticipated a return worth 4 1/2 times its donations for copays for commercial insurance, according to congressional investigators. And companies can earn up to $21 million for every million they donate for Medicare copays, according to a document from the financial services firm Citi, which Mitchell uncovered.
Re: Medicare Coverage Of Revlimid
Thank you Dr. V! If docs are advocating / lobbying for Medicare change on the oral chemotherapy drug issue, I hope you’ll tap into families and patients for support. I know that we were totally shocked and outraged. Celgene is being helpful just seems silly to take “charity” when she has a perfectly good insurance policy ….
Also Check: Does Medicare Cover New Patient Visit
Does Medicare Cover Chemotherapy
Medicare covers prescribed chemotherapy drugs. How and where a person receives chemotherapy helps determine which Medicare part provides the coverage.
When a person receives a cancer diagnosis, their doctor may prescribe chemotherapy drugs. People can take these by mouth or through an intravenous line. Medicare helps pay for chemotherapy deemed medically necessary.
Medicare is a federal health insurance plan for people aged 65 and older. Younger people with a disability may also be eligible for coverage. Medicare has several parts that provide different benefits:
- Part A covers in-hospital care.
- Part B covers outpatient services, including doctor visits, preventive care, and durable medical equipment.
- Part D covers many prescribed medications.
How a person receives the treatment and in what setting determines which Medicare parts cover the costs and which out-of-pocket expenses apply.
In this article, we discuss how Medicare covers chemotherapy and how a person might fill gaps in coverage.
When a doctor who accepts Medicare insurance prescribes cancer treatment, Medicare covers some of the costs. Each part of Medicare can cover different aspects of chemotherapy.
Revlimid Prices Coupons And Patient Assistance Programs
A generic version of Revlimid has been approved by the FDA. However we either do not have pricing information for it, or it is not commercially available. See generic Revlimid availability
Revlimid is a member of the miscellaneous antineoplastics drug class and is commonly used forAnemia, Follicular Lymphoma, Lymphoma, and others.
Don’t Miss: Who Can Get Medicare Before Age 65
Significant Concerns When Taking Revlimid
Because Revlimid affects cell growth, it should not be taken by anyone who is pregnant or breastfeeding. Revlimid can cause severe birth defects in a developing fetus and can cause embryo or fetal death. Two negative pregnancy tests are required before administration of Revlimid, and individuals on Revlimid should use two forms of contraception for 4 weeks before starting this drug, throughout the course of treatment and for 4 weeks after stopping this drug.
Blood clots are another concern for those taking Revlimid. There is a risk of increased arterial and venous blood clots, stroke, myocardial infarction and pulmonary embolism in those taking Revlimid. Signs of blood clotting include shortness of breath, swelling of the arms or legs and chest pain. Someone on Revlimid who experiences these symptoms should seek out medical attention immediately. Talk to your doctor about whether you should take medication to reduce the risk of blood clots while on Revlimid.
Revlimid may also cause neutropenia, a severe and sudden decrease in white blood cells. Neutropenia may be treated through dosage reductions or additional medication.
Prescription Drugs Were Not Covered For Medicare Beneficiaries Before 2006 Now The Top
February 25, 2022 – All Medicare plans must cover a wide range of prescription drugs, including most drugs in certain protected classes. But Medicare Part D plans must cover all or substantially all drugs in six categories: antidepressants, antipsychotics, anticonvulsants, antiretrovirals, immunosuppressants, and anticancer.
Prescription drugs were not covered for Medicare beneficiaries before 2006. But the passage of the Medicare Prescription Drug, Improvement, and Modernization Act developed Medicare Part D.
Medicare Part D plan enrollment has doubled since the start of the program, covering 48 million out of the 62 million people covered by Medicare, according to the Kaiser Family Foundation.
Dig Deeper
In 2022, beneficiaries in each state will have the option to enroll in a Part D plan participating in an Innovation Center model. The models enhanced drug plans cover insulin products at a monthly copayment of $35 in the Part D benefits deductible, initial coverage, and coverage gap phases.
A total of 2,159 Part D plans will participate in this model, a 32 percent increase from last year.
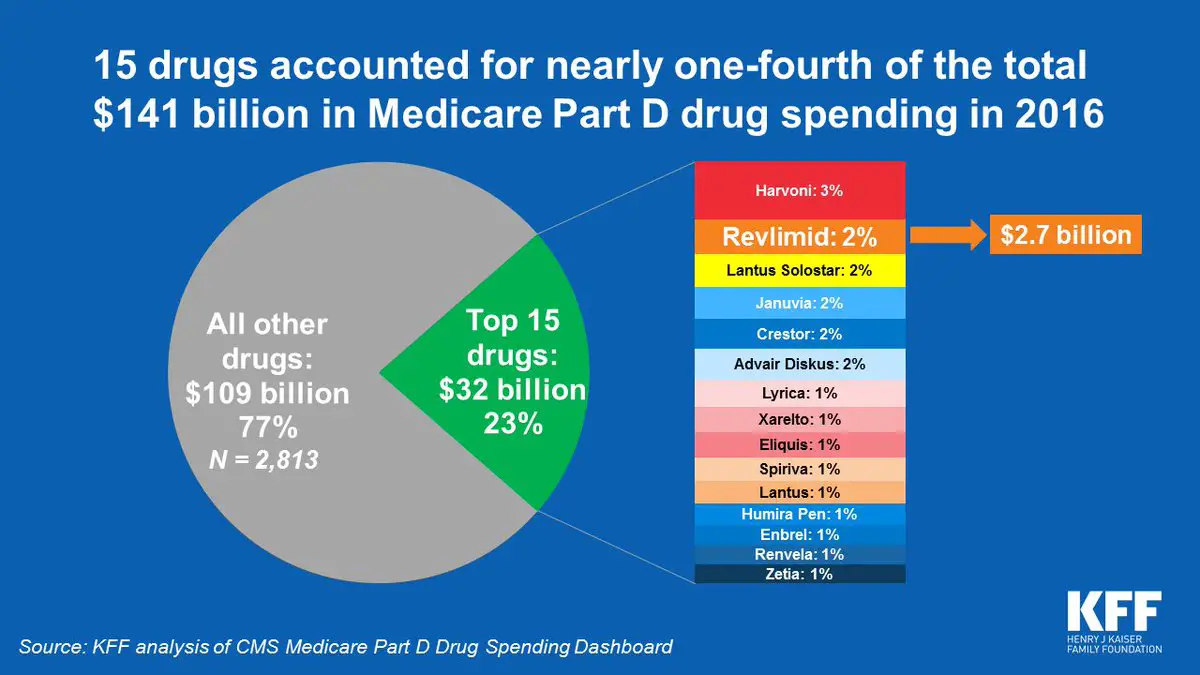
The top-selling Medicare Part D drugs of all time include Revlimid, Eliquis, Xarelto, Januvia, Imbruvica, Trulicity, Ibrance, and Humira.
According to an analysis from Xtelligent Healthcare Medias Research Team, Eliquis, Revlimid, and Xarelto remained the top-three-selling Medicare Part D drugs from 2018 to 2020.
Also Check: Is Suboxone Covered By Medicare
The High Cost Of Brand
It’s all part of the reason American pharmaceutical prices are 2 1/2 times those in other wealthy countries, and thats because of brand-name drugs like Revlimid, said Harvard Medical School professor Dr. Aaron Kesselheim.
Our drug pricing problem is a brand-name pricing problem because brand-name drugs make up about 10% of the prescriptions that are filled in the United States, but they make up about 75 or 80% of the spending, Kesselheim said.
In other wealthy countries, like Germany and France, scientists assess each drugs benefits and price them accordingly. Companies that come up with novel cures can charge more. They get less if theres an alternative treatment.
A system like that would be a step up from what we currently have, Kesselheim said.
What we currently have in the United States is a system in which we allow pharmaceutical companies to charge whatever they want for the drug, no matter how clinically valuable or not valuable it is, Kesselheim said.
And companies take advantage by manipulating the patent system. A patent gives a monopoly for 20 years, theoretically to give companies time to recoup the costs of research and development. But many companies try to extend that time by coming up with a lot of secondary patents on similar products.
It might be a tablet instead of a capsule, a 23-milligram version instead of a 20-milligram version, Kesselheim said.
We do make a profit on the drug in the aggregate European Union, Alles said.
Can Medicare Patients Get Financial Assistance
Private insurance patients usually qualify for financial assistance through the manufacturer. Medicare and Medicare Advantage patients usually qualify for a grant through a foundation. Another benefit of a medically-integrated dispenser is that youll have a real person to talk to and who knows your medical history.
Read Also: What Time Can I Call Medicare
Does Medicare Cover Revlimid
Yes! 100% of Medicare Advantage plans and Medicare Part D plans cover Revlimid.1
- Medicare Advantage plans that offer prescription drug coverage are called Medicare Advantage Prescription Drug Plans . Most Medicare Advantage beneficiaries are enrolled in MA-PDs.2
- Medicare prescription drugs plans each have their own formulary, or drug list, that details what prescription drugs are covered by the plan and how they are covered.
Drug coverage may vary based on plan availability. You may be able to find Medicare Advantage plan options in your area that cover Revlimid.
Find Medicare Advantage plans with drug coverage
Or call 1-800-557-6059TTY Users: 711 24/7 to speak with a licensed insurance agent.
You can also compare Part D prescription drug plans available where you live and enroll in a Medicare prescription drug plan online when you visit MyRxPlans.com.
Medicare Part D Spending On Pricey Specialty Drugs Has Tripled
People with lower incomes can qualify for Part D subsidies 2.6 million who reached catastrophic coverage received these subsidies in 2016 that put a ceiling on their drug costs. But Holt and other middle class seniors, particularly those with chronic conditions, face high and growing out-of-pocket spending on prescription drugs year after year.
The catastrophic phase of Part D is frequently an afterthought in discussions of Medicare because the co-insurance seems so modest. But in a study we recently published in the journal Health Affairs, we found that rapidly increasing list prices for drugs helped drive the catastrophic proportion of total Part D spending from 18 percent in 2007 to 38 percent in 2016. The number of Medicare beneficiaries who arent eligible for subsidies who needed catastrophic coverage, such as Holt, doubled in number in that period, and the proportion of their total spending that occurred in catastrophic coverage increased threefold. Though co-insurance is only 5 percent in that phase, the considerable growth in catastrophic spending exposes beneficiaries to higher out-of-pocket costs.
So why is there no action? Despite the general agreement, a Part D cap is a low priority in Washington. It is caught in the broader debate over health care and entitlement reform, which is fraught with political drama.
Don’t Miss: Does Medicare Pay For Mental Health Services
