Where Can I Find Out More
- Medicaid.gov has links to information explaining the program and to every states Medicaid office.
- Each state has a State Health Insurance Assistance Program that provides counseling and help for Medicare beneficiaries. SHIP counselors can answer some of your Medicaid questions and refer you to local Medicaid officials to help with others.
- The National Council on Aging has a benefits checkup website that has information on Medicare, Medicaid and other programs that help older Americans.
More on Medicare
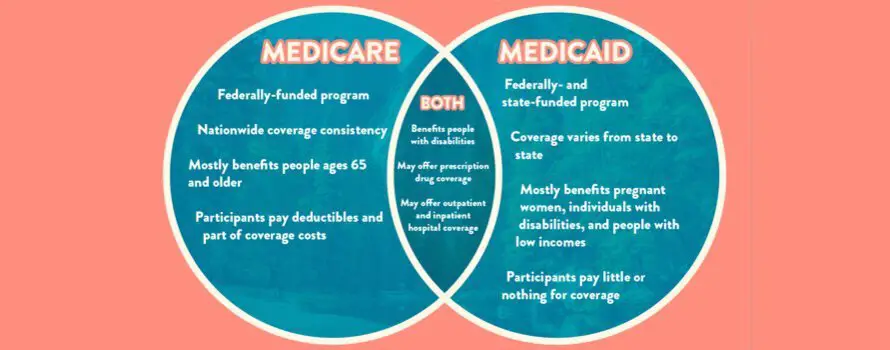
What Are The Differences Between Medicare & Medicaid
Medicare is a federal health insurance program available to individuals 65 years or older. Younger individuals with specific disabilities may also qualify for Medicare benefits.
Medicaid is a federal health care program jointly funded by the federal government and state governments for those who qualify due to income level. It provides partial or full health care coverage, which may help some eliminate medical costs altogether. While the program follows federal guidelines, each state sets its own eligibility requirements and requires annual recertification. Medicaid is typically reserved for low-income children, pregnant women, seniors, and disabled individuals.
Does Medicaid Pay Secondary To Medicare Advantage Plans
Medicaid is always the secondary payer when it comes to health insurance, says Watts.
Medicaid never pays first for services covered by Medicare. Instead, it pays for whatever isnt covered by Medicare. Medicaid may also cover some drugs and additional services that the Medicare Advantage plan doesnt cover fully or at all.
Medicaid is a great benefit for consumers who are eligible, says Watts. However, if you dont meet the criteria, he recommends looking into other avenues of help that may be available. For instance, if you dont qualify for Medicaid, you may qualify for a Low Income Subsidy . LIS helps cover prescription card costs, and pays for a portion of your drugs as well, says Watts.
Some states like New York may have pharmacy assistance programs, as well as additional help from private drug companies.
Recommended Reading: How To Qualify For Extra Help With Medicare Part D
Personal Support Is Part Of A Dual Plan
With many MSHO plans, youll choose a primary care physician to manage your care. Your doctor can also refer you to a specialist or get health plan approval for certain care, if needed.
The plan will have a network of doctors, clinics and hospitals. Check the provider list to make sure you get your care in-network. You may have to pay for services you get out of the network . For home and community-based services, MSHO plans use every provider that is enrolled with the State.
Youll also have a Care Coordinator to guide your health care. This person is usually a registered nurse or a licensed social worker. Heres the type of personal support a care coordinator provides when youre enrolled in an MSHO plan:
- Explains how your plan works
- Partners with you to understand your key health goals and collaborates with you to create a person-centered care plan then gives you support and tools to reach those goals
- Helps you refill prescriptions as needed
- Helps you navigate Medicare and Medicaid services you may qualify for, like home health care, a personal care assistant, homemaker and companion services, delivered meals, or home safety equipment
Can You Have Medicare And Medicaid At The Same Time
Medicare and Medicaid are both public health insurance programs. If you are dual eligible, you can have both Medicare and Medicaid coverage at the same time.
Two of the key differences between Medicare vs. Medicaid include:
- Medicare is for people age 65 and over and for certain people under 65 who have a qualifying disability. Medicare eligibility is consistent for everyone across the U.S., no matter what state you live in.
- Medicaid is for people of any age who meet certain income qualifications. Medicaid is administered by state governments, and eligibility requirements can differ between states.
Read Also: Does Medicare Have Silver Sneakers
If I Have Medicaid Do I Need Medicare Part D
Those that have Medicare and Medicaid will automatically be enrolled in a Part D plan if they dont select one for themselves. Its in the enrollees best interest to select a policy to enroll in, instead of being dropped into a plan. But, either way, Medicaid will help cover the costs associated with premiums, copayments, or coinsurances.
Does Medicaid Pay What Medicare Doesn T
Both Medicare Part A and Part B copays and coinsurance. The Medicare Part D premium, deductibles and copays for prescription drugs. In some states, Medicaid will cover benefits that Medicare does not, such as dental care, transportation to and from doctor visits, eyeglasses, physical therapy and other services.
Also Check: Will Medicare Pay For Handicap Bathroom
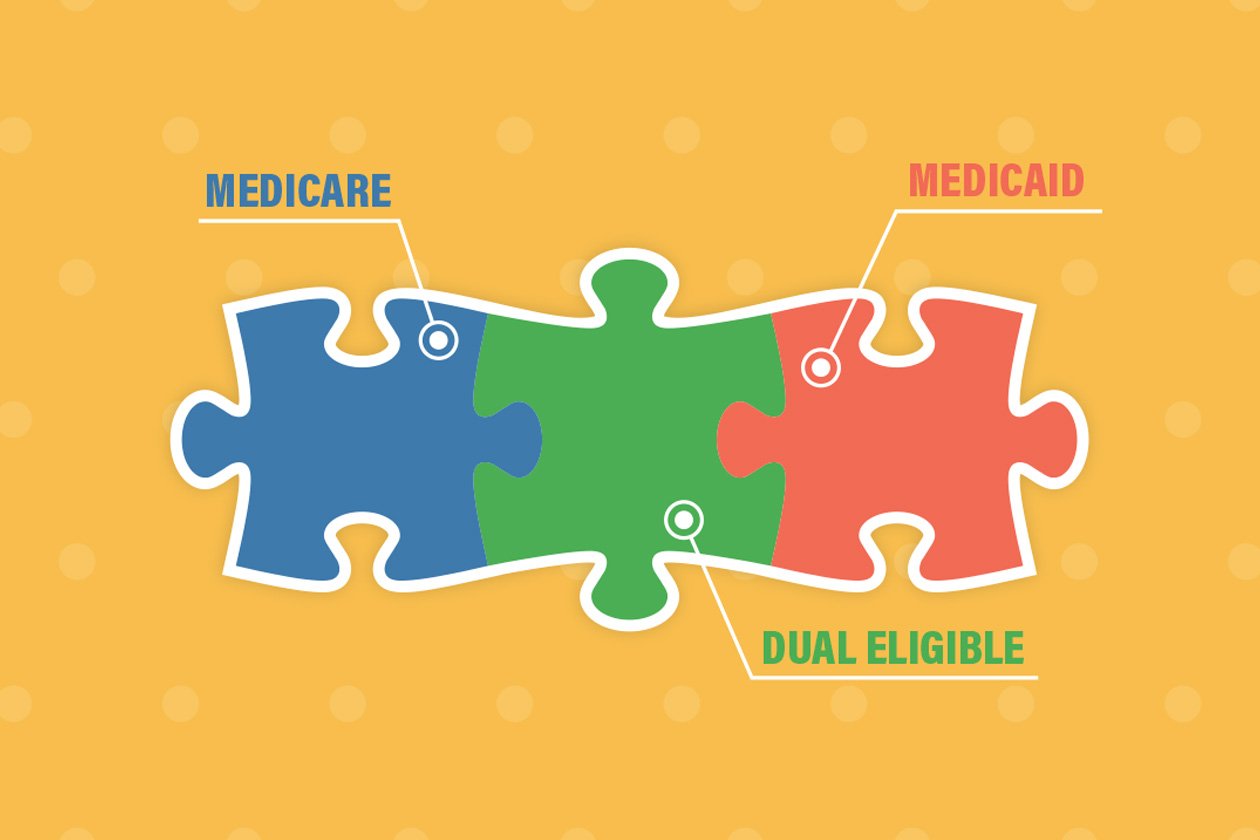
How Do You Qualify For Dual Eligibility
To be dual eligible means to be eligible for Medicare Part A and/or Part B along with full Medicaid benefits and/or assistance. Being dual eligible and enrolling in Medicare and Medicaid means you typically get assistance with Medicare costs such as premiums, coinsurance and deductibles through a Medicare Savings Program .
Income Tiers For Dual Eligibility
Each state sets its own income limits for Medicaid eligibility. Thus, the income tiers for dual eligibility will also vary from state to state.
A reasonable benchmark to use for Medicaid eligibility in 2021 is 138% of the federal poverty level. The federal poverty level is a measure of annual income issued every year by the Department of Health and Human Services to determine eligibility for Medicaid and certain other assistance programs.
For 2021, the federal poverty level for the continental 48 states and the District of Columbia is:
- $12,880 for individuals
- $17,420 for a family of 2
- $21,960 for a family of 3
- $26,500 for a family of 4
- $31,040 for a family of 5
- $35,580 for a family of 6
- $40,120 for a family of 7
- $44,660 for a family of 8
Federal poverty levels differ in Alaska and Hawaii.
Most states use an income of no more than 138% of the federal poverty level in order to be eligible for Medicaid. For example, a family of 3 in Arizona would need a household income of no more than $30,304.80 in order to be eligible for Medicaid.
If a member of that family is also eligible for Medicare because of their age or a disability, they would be dual eligible.
Some states have different income tiers for families and individuals. You can explore a complete online list of state income tiers for Medicaid eligibility.
Also Check: Does Medicare Cover Laser Therapy
What Steps Do I Need To Take To Move From Expanded Medicaid To Medicare
If youre enrolled in expanded Medicaid and youll soon be 65, youll want to familiarize yourself with the health coverage and assistance programs that might be available to you.
Understand that although your assets have not been taken into consideration to determine your eligibility for expanded Medicaid, that will likely change when you turn 65. Every state has an asset limit for full Medicaid eligibility if youre 65 or older, and most states also have asset limits for their MSPs.
But if you do qualify for an MSP particularly the Qualified Medicare Beneficiary program along with Extra Help for prescription drugs you may find that you still qualify for premium-free coverage and very limited out-of-pocket costs.
Youll want to reach out to your states Medicaid office prior to turning 65, to be sure you understand the specifics of 65+ Medicaid and MSP eligibility.
You can also reach out to the Medicare SHIP in your state, to see what resources and assistance are available to you.
You might also want to find a Medicare broker who can help you understand the available Medigap, Part D, and Medicare Advantage plans. Your limited income might make you a good candidate for a low-cost or zero-premium Medicare Advantage plan, leaving you with just the cost of Medicare Part B.
Heres more about choosing between Medigap and Medicare Advantage theres no single solution that works for everyone, so take your time and compare the options available to you.
Can I Be Covered By Both Medicare And Medicaid
It is possible to be eligible and covered by both Medicare and Medicaid. Within health care, it is known as being “dual eligible.” Typically, these individuals will be enrolled in Original Medicare but receive subsidized Medicaid benefits through Medicare Savings Programs such as the:
- Qualified Medicare Beneficiary Program
- Specified Low-Income Medicare Beneficiary Program
- Qualified Disabled Working Individual Program
All of these programs would provide extra help for covering premiums, deductibles and coinsurance for Medicare.
If you don’t qualify for Medicaid when you are enrolled in Medicare, there are still options to help provide financial aid for Part A, B and D deductibles. This would include enrolling in a supplemental Medigap policy such as Medicare Part F, which is offered by private health insurance companies.
Editorial Note: The content of this article is based on the authors opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.
Also Check: Which Cpap Machines Are Covered By Medicare
Transitioning From Expanded Medicaid To Medigap
The more expensive way to cover the gaps in traditional Medicare is to buy a Medigap policy, which generally costs anywhere from a minimum of $25/month to more than $200/month to cover out-of-pocket costs for Parts A and B. Thats on top of premiums for Medicare Parts B and D .
The payoff is maintaining unlimited access to all healthcare providers who accept Medicare which almost all providers do. Heres more about choosing between Medigap and Medicare Advantage.
Who Is Eligible For Both Medicare And Medicaid
To qualify for Medicare, individuals generally need to be 65 or older or have a qualifying disability. There are several levels of assistance an individual can receive as a dual eligible beneficiary. The term full dual eligible refers to individuals who are enrolled in Medicare and receive full Medicaid benefits.
Don’t Miss: Does Social Security Disability Include Medicare
The Problem: Medicare Alone Will Cost You Money
Medicare is a great health insurance program, but it does have costs. You must pay your monthly Part B premium to stay enrolled in Medicare, plus premiums, out-of-pocket costs, etc. Copayments for medical services and prescriptions can add up beyond what many people can afford.
You could even wind up paying more than other folks for the same basic Medicare coverage, simply because extra coverage add-ons are out of reach.
What Is The Difference Between Medicare And Medicaid
If youve ever been confused about the differences between Medicare and Medicaid, you are not alone. Simply put, both Medicare and Medicaid are government-regulated health insurance programs that help to provide healthcare service and treatment to millions of Americans, but each program has slightly different rules of eligibility and provides different coverage to different groups of people.
Recommended Reading: Which Medicare Plans Cover Silver Sneakers
Can I Select An Insurance Plan For My Medicare And Medicaid Benefits
If you are dual eligible, you are can enroll in a dual eligible special needs plan that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid dont over individually, including over-the-counter items, hearing aids, and vision or dental care.
Beneficiaries who are dual eligible can change between Original Medicare and Medicare Advantage or switch Part D plans at each quarter.
Read more about the Medicaid benefits available to Medicare enrollees.
Josh Schultz has a strong background in Medicare and the Affordable Care Act. He coordinated a Medicare ombudsman contract at the Medicare Rights Center in New York City, and represented clients in extensive Medicare claims and appeals. In addition to advocacy work, Josh helped implement health insurance exchanges at the technology firm hCentive. He also has held consulting roles, including at Sachs Policy Group, where he worked with insurer, hospital and technology clients.
Unitedhealthcare Dual Complete Plans
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. This information is not a complete description of benefits. Call TTY 711 for more information. Limitations, co-payments, and restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
Don’t Miss: Is Ed Medication Covered By Medicare
Can I Have Both At The Same Time
If you qualify for both Medicare and Medicaid, you can have them both simultaneously. When you have both it means that you are unlikely to have any out-of-pocket medical expenses. Around 20 percent of Medicare beneficiaries are also eligible for Medicaid. They are called dual-eligibleDual-eligible beneficiaries are those who receive both Medicare and Medicaid benefits. It includes beneficiaries enrolled in Medicare Part A and/or Part B while receiving full Medicaid and/or financial assistance through a Medicare Savings Program….. You would need to apply for each one separately to determine if you can qualify for both.
Dual-eligibles are categorized based on whether they receive full or partial Medicaid benefits. Full benefit dual-eligibles receive comprehensive Medicaid coverage, while partial benefit dual-eligibles receive help with their Medicare premiums and cost-sharing through one of four Medicare Savings Programs.
Who Is Eligible For Medicare
Medicare is a federally-run health insurance program for people age 65 and over and people under the age of 65 who have a qualifying disability. Original Medicare, which is proved by the federal government, consists of Medicare Part A hospital insurance and Medicare Part B medical insurance.
To be eligible for Medicare, you must meet the following Medicare eligibility requirements:
You may also be eligible for Medicare if you or your spouse is a current or former government employee who has paid Medicare taxes while working.
If you do not qualify for retirement or disability benefits, you may still be eligible for Medicare at age 65, but you may have to pay a monthly premium for Medicare Part A.
You May Like: Will Medicare Pay For Alcohol Rehab
Unitedhealthcare Connected For Mycare Ohio
UnitedHealthcare Connected® for MyCare Ohio is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees. If you have any problem reading or understanding this or any other UnitedHealthcare Connected® for MyCare Ohio information, please contact our Member Services at from 7 a.m. to 8 p.m. Monday through Friday for help at no cost to you.
Si tiene problemas para leer o comprender esta o cualquier otra documentación de UnitedHealthcare Connected® de MyCare Ohio , comuníquese con nuestro Departamento de Servicio al Cliente para obtener información adicional sin costo para usted al de lunes a viernes de 7 a.m. a 8 p.m. .
Is There An Open Enrollment Period For Medicaid
- No. You can enroll in Medicaid at any time during the year. But in many states you have to update your enrollment information every year to make sure you still qualify. If you dont, you can lose your coverage. Jennifer Goldberg, directing attorney at Justice in Aging, says: We see people who dont know they dont have coverage until they get a bill or show up at the pharmacy and the prescription they used to pay $1 for is showing up as $100.”
Also Check: How Do I Find Out My Medicare Number
How Do I Know If I Qualify For Medicaid And Medicare
Twelve million individuals are currently enrolled in both Medicaid and Medicare.1 These individuals are known as dual eligible beneficiaries because they qualify for both programs. As long as you meet the federal qualifications for Medicare eligibility and the state-specific qualifications for Medicaid eligibility, you will qualify as a dual eligible. To qualify for Medicare, individuals generally need to be 65 or older or have a qualifying disability.
There are several levels of assistance an individual can receive as a dual eligible beneficiary. The term full dual eligible refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as partial dual eligible.
*Cost sharing is the amount of your health care that you pay out of your own pocket. Typically, this includes deductibles, coinsurance, and copayments.
What Is Pace For Medicare And Medicaid
Another Medicare and Medicaid program is PACE, or Programs of All-Inclusive Care for the Elderly.
PACE helps older Medicare beneficiaries to seek health care within their community, in their home and at PACE facilities.
Some of the things that can be covered by PACE include:
- Adult day primary care
- Caregiver training
- Transportation to a PACE facility when medically necessary
PACE is not strictly restricted to Medicare dual eligible beneficiaries. You may be eligible for PACE with only Medicare or only Medicaid .
However, you must meet all of the following conditions:
- Be at least 55 years old
- Live in the service area of a PACE organization
- Require a nursing home-level of care
- Be able to live safely in the community with help from PACE
Don’t Miss: Does Medicare Cover Chronic Pain Management
How A Dually Eligible Beneficiarys Medical Bills Are Paid
Medicare continues to be a dually eligible beneficiarys primary payer. They are free to seek care from any provider that accepts Medicare. However, Original Medicare offers coverage that is limited in scope. For this reason, many beneficiaries who can afford it choose to purchase a Prescription Drug Coverage Plan , a Medicare Supplement Insurance Policy or a Medicare Advantage Plan to fill these gaps in coverage.
For example, if a full-benefit dual-eligible beneficiary has Original Medicare and a Medigap Plan, then Medigap will function as the secondary payer. Essentially, Original Medicare will pay up to the limits of its coverage and then the secondary payer will pay the remaining costs up to its coverage. Medicaid would then function as the tertiary payer and cover any qualifying expenses that Medicare and Medigap do not.
