Helping Your Client Apply For Extra Help With Medicare
Anyone who does not automatically get the LIS, should complete the Medicare Extra Help application if theres a chance they are eligible for it. If you think your client may qualify for this program, you can help them apply for it via the Social Security Administrations website. Clients can also call or visit their local Social Security office to apply. Individuals who need further assistance can contact their State Health Insurance Assistance Program .
â â â
Did you know that a 2010 study found that more than 2.3 million Medicare beneficiaries who werenât enrolled in the governmentâs Medicare Extra Help program may have qualified for it? Dont let your clients be a part of this statistic. Help them take advantage of the financial assistance theyre entitled to, but may not know about, starting today!
Check The Status Of A Claim
To check the status of
claims:
- Log into your secure Medicare account. Youll usually be able to see a claim within 24 hours after Medicare processes it.
- Check your Medicare Summary Notice . The MSN is a notice that people with Original Medicare get in the mail every 3 months. It shows:
- All your Part A and Part B-covered services or supplies billed to Medicare during a 3-month period
- What Medicare paid
- Use Medicare’s Blue Button by logging into your Medicare account to download and save your Part A and Part B claims information. Learn more about Medicares Blue Button.
Deductibles Copays And Coinsurance
Original Medicare has an annual deductible that in the calendar year 2020 was set at $1,408 for Part A and $198 for Part B. Each Medicare Advantage plan has its list of consumer paid expenses. They include deductibles, copays, coinsurance, and cost-sharing.
These expenses are part of the coverage provided by Medicare or Medicare Advantage.
Comparison shopping is a powerful tool for finding the best value in health insurance plans. Consumers can focus on particular features such as out-of-pocket expenses to find the best choice.
Read Also: Is Kaiser A Medicare Advantage Plan
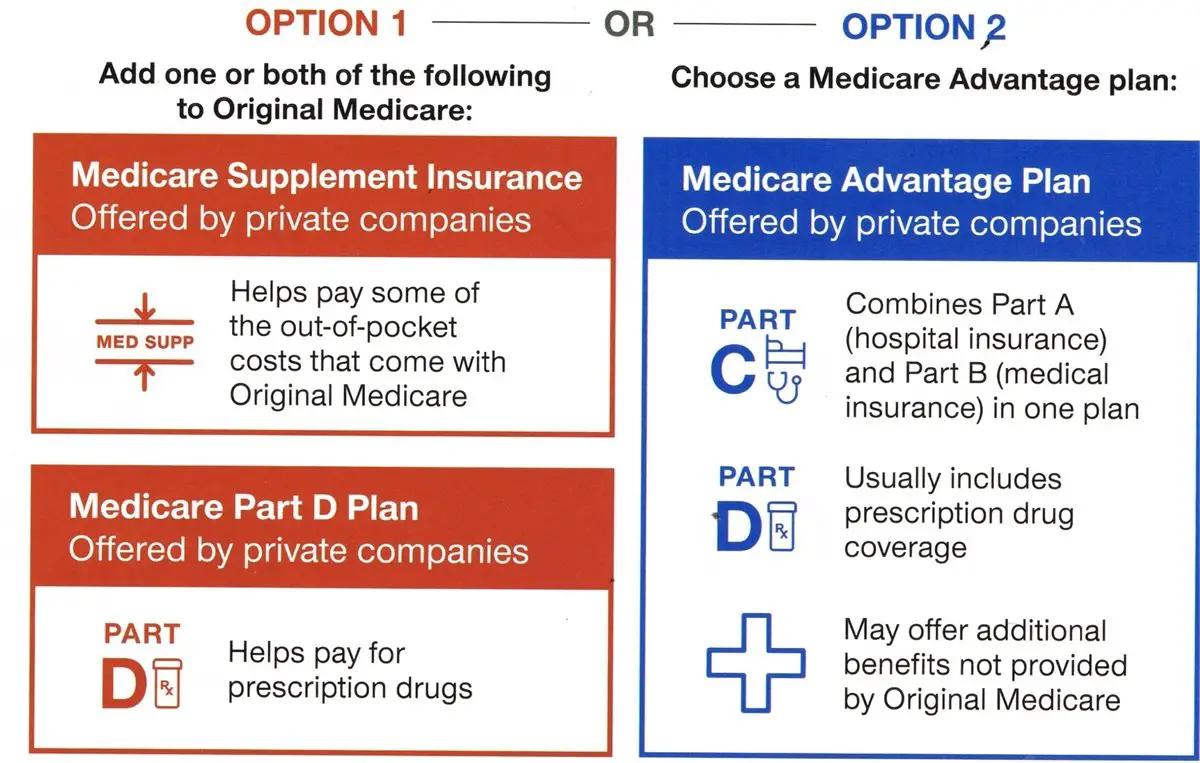
Medicare Offers Important Choices
Medicare has two paths that subscribers should consider at the outset. They can choose between Original Medicare and Medicare Advantage. They represent similar coverage, but one consists of private plans, and the other is government-run. Original Medicare is an open arrangement.Users can go to any doctor or medical care provider that accepts Medicare.
Medicare Advantage plans also provide comprehensive coverage but achieves it in different ways. They have management styles that can help patients, for example, some provide a primary care doctor. They offer a network that can have lower pricing than similar benefits on Original Medicare. Advantage plans can cost less than Medicare Part B and add prescription drug benefits for an all-in-one combination.
Users can go to any doctor or medical care provider that accepts Medicare. Medicare Advantage plans also provide comprehensive coverage but achieves it in different ways. They have management styles that can help patients, for example, some provide a primary care doctor. They offer a network that can have lower pricing than similar benefits on Original Medicare. Advantage plans can cost less than Medicare Part B and add prescription drug benefits for an all-in-one combination.
Ihcp Provider Healthcare Portal
The IHCP Provider Healthcare Portal is a secure website that allows you to perform multiple functions including obtaining eligibility information and filing fee-for-service claims. The Portal is fast and easy to use, and online help is available through the eligibility verification process. For more information, see the provider reference module.
Also Check: Are Hearing Aids Covered By Medicare Part B
I’m On Disability When Will I Be Eligible For Medicare
You may be eligible for Medicare before age 65 if you have a qualifying disability. Eligibility usually starts after you’ve received disability benefits for 24 months. You will be automatically enrolled in Medicare Parts A and B. You may make other coverage choices during your IEP. Your 7-month IEP includes the month you receive your 25th disability check plus the 3 months before and the 3 months after.
What Is The Medicare Extra Help Program
The Extra Help program is a joint effort by the Centers for Medicare & Medicaid Services and the Social Security Administration to provide financial assistance to those who need it to pay for their Medicare prescription drug coverage and prescription drugs. This program is also called the Medicare Low-Income Subsidy program.
Don’t Miss: What Are The Four Different Parts Of Medicare
District Of Columbia Medicaid Eligibility
Residents of Washington DC can apply for DC Medicaid, which covers healthcare costs for qualifying people who have disabilities or reduced incomes. Many services covered include vision care, doctor visits, hospice services, medical supplies, and organ transplants.
Which Medicaid plan is best in Washington DC?
Medicaid benefits in Washington DC vary based on your personal situation and health needs. In most cases, you will still be able to visit your doctor of choice, so long as they accept Medicaid payments. DC Medicaid also provides additional programs for people with developmental and physical disabilities, as well as seniors.
Applying for DC Medicaid requires you to make an in-person visit to an Income Maintenance Administration Service Center. You can find your nearest center here.
District of Columbia Medicaid Application:
North Carolina Medicaid Eligibility
Beyond the standard financial requirement, North Carolina looks at several factors in determining whether your application for benefits will be accepted. These include family size, need for long-term care, ability level, and if you receive Medicare.
Which Medicaid plan is best in North Carolina?
North Carolina provides different levels of coverage based on the above-mentioned factors, as well as other benefits for children and pregnant women. What coverage you qualify for depends on your level of medical and financial need.
Youll need to submit an online application to the Department of Health and Human Services.
North Carolina Medicaid Application:
Read Also: Is Everyone Eligible For Medicare
Medicare Has Four Parts
Medicare is split into parts, each identified by a letter: A, B, C, and D.
When a person has both Parts A and B, this is called having Original Medicare.Part D covers prescription drugs only.
Part C is slightly different it combines the coverage of Parts A, B, and D under a type of plan called Medicare Advantage.
We explore all of these parts of Medicare below.
Medicare Part A: Hospital Insurance covers for inpatient services when admitted to the hospital, as well as home health care, skilled nursing care and Hospice. Part A may require a premium depending on work history while paying taxes, but typically beneficiaries are entitled to it at no cost. Individuals receiving at least four months of Railroad Retirement Board Benefits or Social Security benefits before they turned 65 will be automatically enrolled. Others must contact Social Security to enroll in Part A of Medicare.
Medicare Part B: Medical Insurance is outpatient physician care that includes doctors visits and other medical services as well as durable medical equipment for home use. Part B requires a premium in most cases. In 2021, this monthly premium is $148.50.
You can start here and now Medicare costs and insurance options at no cost!
How To Get Premium
The system of eligibility for Medicare measures the working years in which the individual paid the Federal Insurance Contributions Act tax, or FICA tax.
With the exceptions of self-employment and certain government positions, most people have this included in the payroll taxes deducted from each paycheck.
These working years accrue what is known as Quarters of Coverage.
Quarters of Coverage each represent a three-month period of work while paying the FICA tax about 4 Quarters of Coverage are earned in a single year.
The Quarters of Coverage are units of measuring eligibility for Medicare coverage and Social Security benefits. This measurement determines both the level of monthly Social Security income benefits and whether Part A is premium-free.
To get Part A premium-free, one typically must have earned 40 quarters of coverage, or about 10 years of employment while paying payroll taxes. The 40 total Quarters of Coverage do not have to be earned over 10 consecutive years.
These quarters of coverage can be earned through ones own work history or the work history of a spouse, parent, or child.
Those who have not quite accrued 40 Quarters of Coverage can still join Medicare Part A at age 65, but it will require paying a premium.
Earning 30-39 credits sets the monthly premium for Part A in 2021 at $259, and having earned less than 30 credits sets the Part A premium at $471.
In 2021, the Medicare Part B premium for most people is $148.50.
Recommended Reading: Does Medicare Cover Oxygen At Home
New Mexico Medicaid Eligibility
In New Mexico, Medicaid eligibility is partially based on your household income, as well as other medical needs you may have . You must be a resident of the state to qualify for Medicaid.
Which Medicaid plan is best in New Mexico?
Many adults who receive Medicaid benefits are entitled to the New Mexico Alternative Benefit Plan . Though other recipients with special needs such as disabilities or serious medical conditions qualify for the states Standard Medicare plan. How you and your family qualify depends on your particular needs and financial situation.
You can submit an application through the YesNM website.
New Mexico Medicaid Application:
Medicaid For Different Groups

While Medicaid programs vary by state, they also can vary with the amount of aid and program benefits provided to different groups. Here we have listed some of the most common groups and different types of medical needs that Medicaid looks to support.
- Medicaid For Dogs
- Medicaid For Pregnancy and Pregnant Mothers
- Medicaid For Providers
- Medicaid For Nursing Home Residents
- Medicaid For College Students
- Medicaid For Adults
- Medicaid For Children
Kansas provides Medicaid benefits through its Medical Assistance Program. Eligibility is determined by income level and health needs, such as childhood care, pregnancy or disability.
Which Medicaid plan is best in Kansas?Your plan choices depend on your eligibility level for Medicaid assistance. Kansas provides plans for children through its Childrens Health Insurance Program that are available to families for no to limited cost. Pregnant women, parents and caregivers, seniors, and people with disabilities also may face additional eligibility requirements that impact their level of benefits.
To apply for Kansas Medicaid benefits, visit the KanCare website.
Read Also: Do I Need Medicare Part C
Important Terms For Medicaid Qualification
Modified Adjusted Gross Income is your total gross income. This includes income from employment, other benefits, child support, alimony, interest, foreign income, etc. All your income sources are included.
Federal Poverty Level is the line designated by the Department of Health and Human Services to determine who is living in poverty.
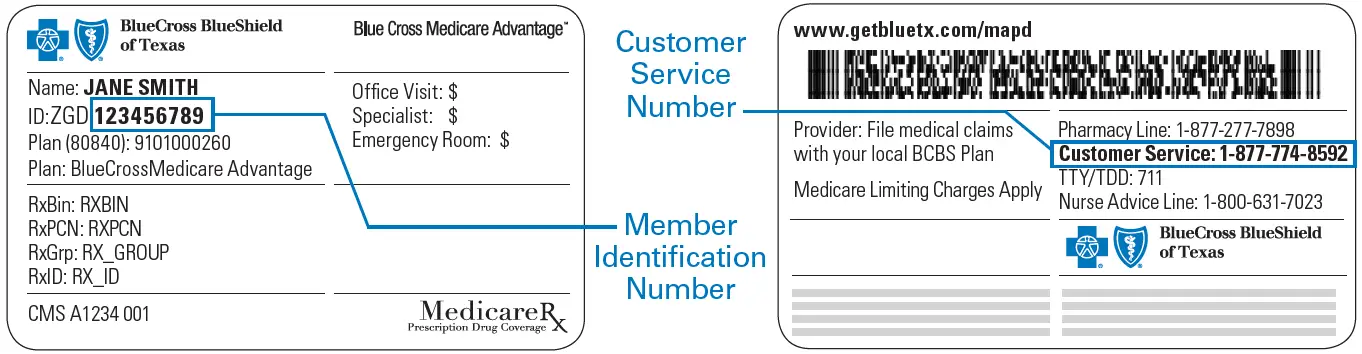
Medicare Eligibility Summary Dashboard
Make easy and informed actions based on a quick-glance overhead view of a patients Part A, Part B, Home Health, Medicare Secondary Payer, HMO, Medicare Advantage Plan, Hospice Dates, and Deductible Remaining details. Labeled with a green check or a red exclamation, scan patients and make actionable decisions without toggling pages.
Don’t Miss: How To Apply For Medicare Through Social Security
Terms Of Use For 1 To 10 Individual Documents Upload
I have elected to upload a group of individual files by identifying and attaching up to 10 individual files. I understand that the files will be named based on the information I enter for each file and that the file name will identify the member that the care coordination document is/are associated with. Additionally, I understand the importance of ensuring that the file is/are named correctly. I certify that the files will be carefully audited and confirmed to be accurately named before confirming my upload. By confirming my upload, I am representing that the file is/are named accurately.
What If I Work Past Age 65
You still have a Medicare enrollment decision to make.
If you plan to keep working or you have employer health coverage through a spouse, you have some options to consider when signing up for Medicare. Depending on your situation, you may or may not be able to delay Medicare enrollment.
Your Initial Enrollment Period happens when you’re turning 65 whether you’re still going to work or not. Be sure to know your IEP dates and plan ahead.
Recommended Reading: How To Order Another Medicare Card
Who Are Aetnas Providers For Medicare Advantage Plans
If you are enrolled in a Medicare Advantage plan with Aetna, you may be required to get your health care from doctors and other providers who are in Aetnas provider network and contracted with Aetna to treat their members. Aetnas Medicare Advantage providers include primary care doctors, specialists, hospitals, surgical centers, laboratories, imaging centers, dentists, pharmacists, and other health-care professionals.
Aetnas network providers have agreed under contract to provide care for its members, usually at lower rates than they would otherwise charge you for the same services if you were not covered by Medicare Advantage plan through Aetna. These providers agree to accept your copayment or allowable coinsurance amount as payment in full for Medicare-covered services.
Depending on the plan you choose, you may be required to get all your care from providers in your Aetna Medicare Advantage plan network you may have to pay in full for out-of-network care.
License For Use Of Current Dental Terminology
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING ABOVE ON THE BUTTON LABELED “ACCEPT”, YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED “DO NOT ACCEPT” AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, “YOU” AND “YOUR” REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
Recommended Reading: What Does Bcbs Medicare Supplement Cover
Comprehensive Long Term Care
Sunshine Health is responsible for providing LTC services once the Florida Department of Elderly Affairs determines an enrollee meets the medical requirements for nursing home level of care and the enrollee formally selects the Sunshine Health Comprehensive plan through AHCAs Choice Counseling. Following that selection, the Department of Children and Family Services determines if the member meets the financial criteria. Once AHCA receives confirmation of a members eligibility, AHCA notifies Sunshine Health of the members effective enrollment date. Coverage typically lasts for a year until DCF recertifies the member. During the annual recertification process, Comprehensive members may receive a 60-day extension of coverage and their benefit category is changed to SIXT on the secure provider portal of AHCAs website.
Who Can Use Find A Patient
You can use an individual PRODA account to access Find a Patient if either:
- you have a Medicare provider number
- youre delegated access by someone with a Medicare provider number.
Hospitals or approved Indigenous and Remote Health Services with a Medicare claiming need, and pharmacies can set up an organisation PRODA account to access Find a Patient.
Your organisations administrator will need to link HPOS to your organisation in PRODA and then add you as a member of the organisation PRODA account. If youre a pharmacy, youll need to link HPOS using your pharmacy approval number. You can then log in to your individual PRODA account to access Find a Patient.
You May Like: Does Medicare Pay For Maintenance Chiropractic Care
New York Medicaid Eligibility
New Yorkers who apply for Medicaid benefits must have income that is determined at or below poverty level. In addition, the state will consider your application if you have high medical bills or receive Supplemental Security Income.
Which Medicaid plan is best in New York?
In many cases, Medicaid will cover most of the costs of your healthcare, though in New York, the program may require you to pay co-payments for some services. You will also be required to select a Managed Care Health Plan that includes doctors in your region or offices you already visit regularly.
You can apply for New York Medicaid benefits through several state agencies.
New York Medicaid Application:
Prescription Drugs With Medicaid
States are permitted to assign out-of-pocket copayments to prescription drugs they deem as non-preferred. Non-preferred drugs are expensive name brand drugs that have a generic counterpart, while preferred drugs are the less expensive generic versions. Each state may create a list of preferred and non-referred drugs. They are allowed to charge up to a 20% copay on non-preferred drugs for people whose income is more than 150% FPL. You can obtain copies of the preferred and non-preferred prescription lists through your state Medicaid office.
You May Like: How To Get Medical Equipment Through Medicare
