Determining Eligibility For Medicare: Who Is Eligible For Medicare
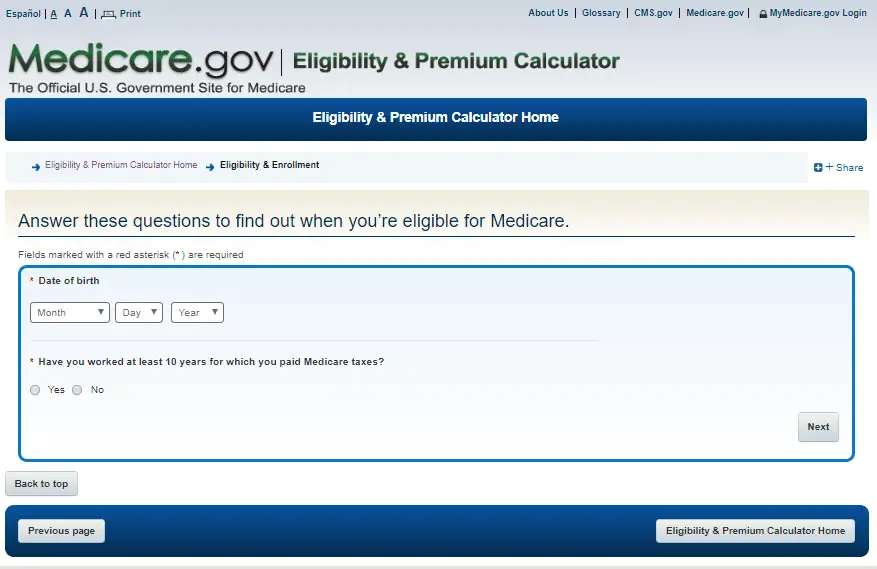
The Medicare website is a good place to start. A button will say Estimate my eligibility. This link will lead to a page that asks a few questions that can affect your eligibility. There is no need to make an account to use this tool.
It assesses factors of age, U.S. citizenship, and whether a person or their spouse has paid Medicare taxes while working for 10 years.
Based on your responses, this tool then answers the questions of whether Medicare enrollment will be done automatically or if one needs to apply for it themselves, as well as explaining the best time to apply.
If eligible, the same page has a link to help estimate the premium amount one needs to pay to get covered under Part A and Part B of Medicare.
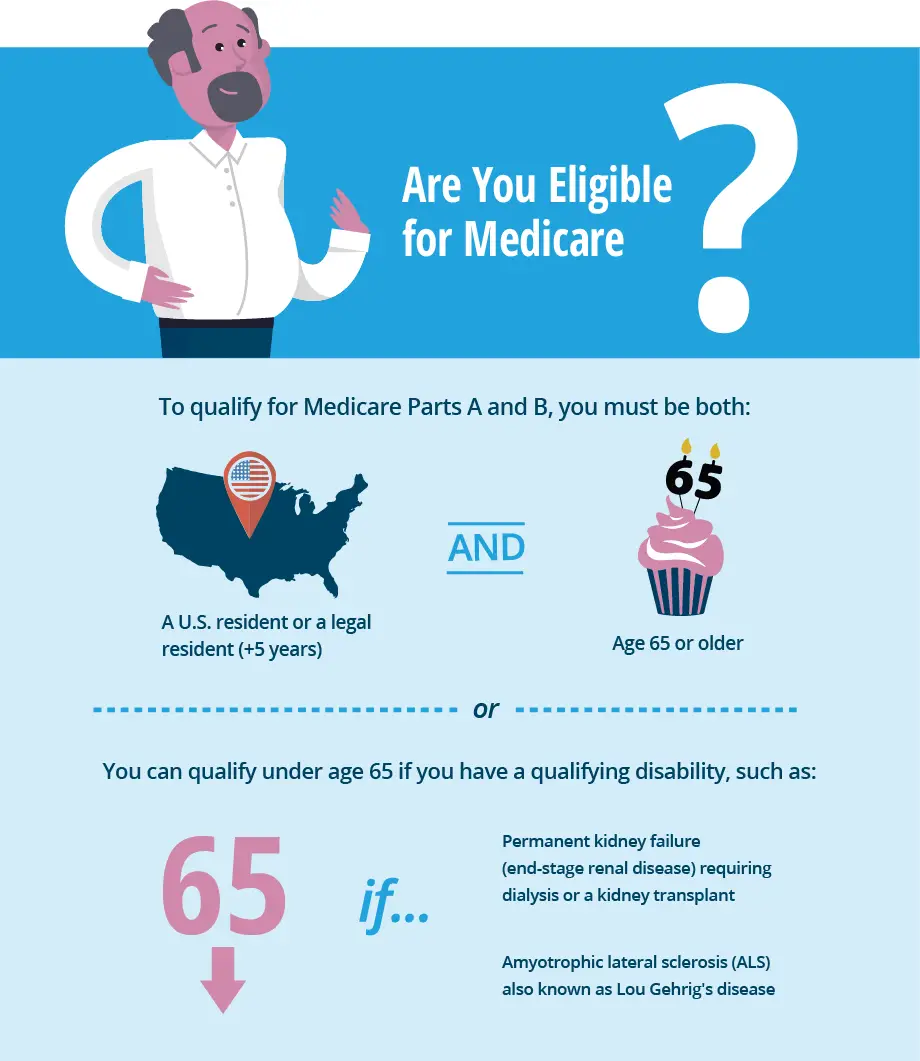
The below-listed items are the essential qualifications for Medicare.
- Age 65 U.S citizens or permanent residents who have lived in the U.S. for 5+ years consecutively.
- Age 64 or less, after receiving disability for twenty-four months
- Those diagnosed with End Stage Renal Disease
Those ages 65 and above with 10 years time working while paying Medicare taxes get Medicare Part A without any premium cost.
Run Medicare Patient Eligibility Batches In Real
pVerify now offers a Self-Batch Eligibility Feature for all Premium clients. Created to report extensive Medicare patient benefits, all information available in a single patient verification is available in the batch processing. With no volume limit, verify Medicare patients in mass and view in the color-coded Excel file. Reports full details on Medicare including Hospice and SNF Dates and eligibility on 54 Preventive Services.
*Included with Premium Portal at no extra cost.
New York Medicaid Eligibility
New Yorkers who apply for Medicaid benefits must have income that is determined at or below poverty level. In addition, the state will consider your application if you have high medical bills or receive Supplemental Security Income.
Which Medicaid plan is best in New York?
In many cases, Medicaid will cover most of the costs of your healthcare, though in New York, the program may require you to pay co-payments for some services. You will also be required to select a Managed Care Health Plan that includes doctors in your region or offices you already visit regularly.
You can apply for New York Medicaid benefits through several state agencies.
New York Medicaid Application:
You May Like: How To Qualify For Medicare And Medicaid
Who Is Eligible For Medicare
Medicare is available to United States citizens and legal residents who have lived in the United States for at least 5 years in a row. Medicare is individual insurance. It doesn’t cover spouses or dependents.
You may become eligible to receive Medicare benefits based on any one of the following:
- You are age 65 or older.
- You are younger than 65 with a qualifying disability. Medicare eligibility begins after 24 months of receiving Social Security disability benefits.
- Any age with a diagnosis of End-Stage Renal Disease or Amyotrophic Lateral Sclerosis
To qualify as a legal resident, you must have lived in the United States for at least 5 years in a row before applying for Medicare.
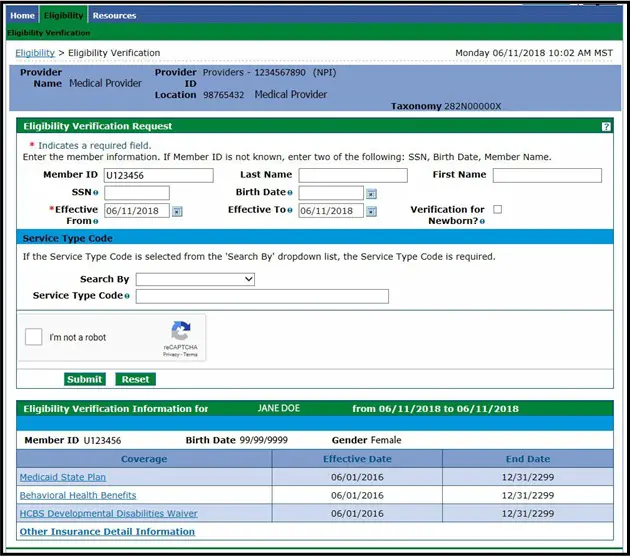
Its Time To Verify Your Patients Eligibility
Important member ID card changes for those with Medicare Advantage plans
The following changes begin on January 1, 2022:
- All Aetna Medicare Advantage plan members will have 12-digit member ID numbers beginning with 10. We will no longer use the ME prefix for Medicare Advantage plans after that date. Consol Energy will transition from ID numbers beginning with ME to those beginning with 10 on April 1, 2022.
- Group # will be known as Plan #.Please use the plan number in the way that you have previously used the group number in your transactions.
When checking your patients eligibility and benefits, use our provider portal on Availity or another vendor or clearinghouse on our list. Vendor fees may apply.
Note when services were performed:
- For services performed on or before December 31, 2021, use the members prior ID number.
- For services performed on or after January 1, 2022 , use the members 2022 MA plan ID number. You can use this number to verify coverage, request an authorization/precertification, issue referrals and submit claims.
Ask your patients for their current member ID card. If they dont have one, you can verify their eligibility using their full first and last name and date of birth. In addition, you can print an electronic copy of a patients ID card, if needed. Make sure that eligibility details match the patients information.
A new year means new plans
Recommended Reading: How To Apply For Medicare In Ga
Contact Us To Create Your Account Today
Meet with a pVerify Representative to access your current Medicare Patient Eligibility Verification Solution to determine the best combination of pVerifys Eligibility Solutions for your needs.
Effortless, automatic outbound/inbound connection from your EMR/Practice Management System to pVerify
Automated verification of your entire appointment calendar with First-Class Batch Processing
Complete and concise Batch Report supporting multiple specialties verified on your requested schedule
White-label pVerify’s secure cloud-based portal with location management, unlimited users, and NPIs
Build pVerify’s APIs directly into your own software with our robust APIs providing Easy Eligibility Endpoints
Verify instantly, estimate the patient responsibility powered by the eligibility results, and collect payment all in one portal
New Mexico Medicaid Eligibility
In New Mexico, Medicaid eligibility is partially based on your household income, as well as other medical needs you may have . You must be a resident of the state to qualify for Medicaid.
Which Medicaid plan is best in New Mexico?
Many adults who receive Medicaid benefits are entitled to the New Mexico Alternative Benefit Plan . Though other recipients with special needs such as disabilities or serious medical conditions qualify for the states Standard Medicare plan. How you and your family qualify depends on your particular needs and financial situation.
You can submit an application through the YesNM website.
New Mexico Medicaid Application:
You May Like: How To Change From Medicare Advantage To Original Medicare
Medicaid Eligibility For Persons With Disabilities
Individuals that are unable to work due to a disability may receive cash assistance through the Supplemental Security Income program. Qualifying for SSI automatically qualifies you for Medicaid in most states, but not all. The federal government requires all states to offer Medicaid to low-income disabled individuals. However, states are still allowed to set their own income eligibility requirements. Ten states, referred to as the 209 states have set income requirements that are more restrictive than SSI requirements. This means that individuals receiving SSI are not guaranteed Medicaid. They have to apply separately and be approved. These ten states are Connecticut, Hawaii, Illinois, Minnesota, Missouri, New Hampshire, North Dakota, Ohio, Oklahoma, and Virginia.
For individuals with a disability that have not been qualified for SSI, there are still options to qualify for Medicaid. Most states allow individuals with an impairment to prove that their impairment has prevented them from being able to work for at least one year. Once this is proven, the individual will be able to apply under the income and asset requirements for people with disabilities.
Medicare Eligibility Verification Made Easy
The success of your healthcare organizations Medicare claims begins with eligibility verification. Trust Waystar, the Medicare experts, to prevent eligibility-related rejections and denials.
Thanks to Waystars real-time unique connection to Medicare, healthcare providers get comprehensive patient data in one quick step and within seconds. This includes patient personal information like name, birth date, gender and Medicare Beneficiary Identifier .
Youll also get Medicare coverage data, like type of coverage, Medicare Advantage plan details, deductible, preventative services, days information, Medicare Secondary Payer insurance, home health sessions and hospice periods.
Our Medicare Eligibility solution automates, simplifies and integrates Medicare eligibility directly into your daily workflow.
Fill out the form to learn more about Medicare Eligibility from Waystar.
“We couldnt believe what wed been missing out on all this time! Waystars eligibility verification has been a great resource for us. Its slashed the time spent checking eligibility in half.” Kim Kuebler // Medicare Billing Supervisor/Manager // Hospice of Cincinnati
Recommended Reading: Does Medicare Pay For Visiting Nurses
What Is Medicare Advantage Plan
Medicare Advantage Plan A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
North Dakota Medicaid Eligibility
The North Dakota Department of Human Services provides assistance with Medicaid enrollment. You must be a North Dakota resident and U.S. citizen. While the state requires you to meet certain financial guidelines, assets such as your home or vehicle will not be counted against your application.
Which Medicaid plan is best in North Dakota?
North Dakota provides a range of Medicaid-related services that you may qualify for based on your health or financial needs. In some cases, you may be required to pay a co-payment for any medical services you receive, though there are exceptions .
You can apply for benefits online, through the mail, or in person.
North Dakota Medicaid Application:
You May Like: Does Medicare Cover End Of Life Care
Important Member Id Card Changes For Those With Aetna Medicare Advantage Plans
The following changes begin on January 1, 2022:
- All Aetna Medicare Advantage plan members will have 12-digit member ID numbers beginning with 10. We will no longer use the ME prefix for Medicare Advantage plans after that date.
- Consol Energy will transition from ID numbers beginning with ME to those beginning with 10 on April 1, 2022.
- Group # will be known as Plan #.Please use the plan number in the way that you have previously used the group number in your transactions.
District Of Columbia Medicaid Eligibility
Residents of Washington DC can apply for DC Medicaid, which covers healthcare costs for qualifying people who have disabilities or reduced incomes. Many services covered include vision care, doctor visits, hospice services, medical supplies, and organ transplants.
Which Medicaid plan is best in Washington DC?
Medicaid benefits in Washington DC vary based on your personal situation and health needs. In most cases, you will still be able to visit your doctor of choice, so long as they accept Medicaid payments. DC Medicaid also provides additional programs for people with developmental and physical disabilities, as well as seniors.
Applying for DC Medicaid requires you to make an in-person visit to an Income Maintenance Administration Service Center. You can find your nearest center here.
District of Columbia Medicaid Application:
Don’t Miss: Does Costco Take Medicare For Hearing Aids
Ihcp Provider Healthcare Portal
The IHCP Provider Healthcare Portal is a secure website that allows you to perform multiple functions including obtaining eligibility information and filing fee-for-service claims. The Portal is fast and easy to use, and online help is available through the eligibility verification process. For more information, see the provider reference module.
Also Check: Are Hearing Aids Covered By Medicare Part B
Medicaid Eligibility Information By State
Medicaid is a government-funded program designed to provide health care coverage for low-income households. This program receives funding from both the state and federal government. The federal government designed the program and maintains program regulations that states are required to follow. States, in turn, are allowed to make decisions regarding eligibility and benefits within the state. Each state maintains its own Medicaid website, which is used as a resource and portal for those applying for and receiving Medicaid.
Don’t Miss: Does Medicare Pay For Multifocal Lens
Medicaid For Different Groups
While Medicaid programs vary by state, they also can vary with the amount of aid and program benefits provided to different groups. Here we have listed some of the most common groups and different types of medical needs that Medicaid looks to support.
- Medicaid For Dogs
- Medicaid For Pregnancy and Pregnant Mothers
- Medicaid For Providers
- Medicaid For Nursing Home Residents
- Medicaid For College Students
- Medicaid For Adults
- Medicaid For Children
Kansas provides Medicaid benefits through its Medical Assistance Program. Eligibility is determined by income level and health needs, such as childhood care, pregnancy or disability.
Which Medicaid plan is best in Kansas?Your plan choices depend on your eligibility level for Medicaid assistance. Kansas provides plans for children through its Childrens Health Insurance Program that are available to families for no to limited cost. Pregnant women, parents and caregivers, seniors, and people with disabilities also may face additional eligibility requirements that impact their level of benefits.
Read Also: Do I Need Medicare Part C
Pverifys Medicare Patient Eligibility Verification Solutions Features:
pVerify provides verified Medicare Eligibility Checks benefits at a deeper level with information separated and highlighted for easier review and understanding
- Confirm Active or Inactive Status, with Medicare A, B, & D details.
- Find out the primary insurance information if Medicare is the secondary payer.
Also Check: Does Medicare Cover Incontinence Supplies 2020
Is Medicare Paid For By Original Medicare
Medicare services arent paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. or other. Medicare Health Plan. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan.
Understanding Medicare Based On Disability
Persons entitled to monthly Social Security or Railroad Retirement Board benefits are automatically entitled to Medicare Part A after twenty-four months of disability benefits.
If disabled government employees are not otherwise eligible for Social Security Benefits through their history of work or contribution to payroll taxes, they get automatic eligibility for Part A after twenty-nine months of receiving disability benefits.
There is a special rule for People with Lou Gehrigs disease. They get eligibility with no waiting period upon the first month of RRB or SSA benefits.
Child disability eligibility begins the month of the 20th birthday except for ALS which is set for age 18.
Those diagnosed with End-Stage Renal Disease are typically eligible to begin Medicare on the first day of the fourth month they receive dialysis treatments.
In addition, to get Part A premium-free, those with End-Stage Renal Disease must also meet one of three below-stated conditions:
Don’t Miss: What Does Medicare Do For You
Coba Trading Partner Contact Information
The Coordination of Benefits Agreement Program establishes a nationally standard contract between CMS and other health insurance organizations that defines the criteria for transmitting enrollee eligibility data and Medicare adjudicated claim data. CMS has provided a COBA Trading Partners customer service contact list as an avenue for providers to contact the trading partners. The COBA Trading Partners document in the Download section below provides a list of automatic crossover trading partners in production, their identification number, and customer contact name and number. For additional information, click the COBA Trading Partners link.
Who Is Not Eligible For Medicare Part A
Why might a person not be eligible for Medicare Part A? A person must be 65 or older to qualify for Medicare Part A. Unless they meet other requirements, such as a qualifying disability, they cannot get Medicare Part A benefits before this age. Some people may be 65 but ineligible for premium-free Medicare Part A.
Read Also: How Do You Qualify For Medicare In Texas
What Is Pecos Medicare Provider Enrollment
What is PECOS? PECOS is the Medicare Provider, Enrollment, Chain and Ownership System. The PECOS system is a database of providers who have registered with CMS. A NPI number is necessary to register in PECOS. Providers must enroll in PECOS to avoid denied claims. This tool is made available based on a CMS data file from 11-08-2021. The information is not warranted or guaranteed.
General Eligibility For Medicare: When Am I Eligible For Medicare
Medicare eligibility goes hand-in-hand with Social Security eligibility.
Individuals in the below-listed categories can get Medicare coverage.
- Persons age 65 or older eligibility begins four months before their 65th birthday
- Disabled persons 64 and under can qualify if receiving disability benefits from Social Security or the RRB for 24 months
- Persons with end-stage renal disease can get premium-free Medicare Part A. Eligibility based on End-Stage Renal Disease requires current dialysis treatment, a kidney transplant, and filing an application for Medicare.
You May Like: Does Medicare Cover 24 Hour Care
North Carolina Medicaid Eligibility
Beyond the standard financial requirement, North Carolina looks at several factors in determining whether your application for benefits will be accepted. These include family size, need for long-term care, ability level, and if you receive Medicare.
Which Medicaid plan is best in North Carolina?
North Carolina provides different levels of coverage based on the above-mentioned factors, as well as other benefits for children and pregnant women. What coverage you qualify for depends on your level of medical and financial need.
Youll need to submit an online application to the Department of Health and Human Services.
North Carolina Medicaid Application:
How To Get Premium
The system of eligibility for Medicare measures the working years in which the individual paid the Federal Insurance Contributions Act tax, or FICA tax.
With the exceptions of self-employment and certain government positions, most people have this included in the payroll taxes deducted from each paycheck.
These working years accrue what is known as Quarters of Coverage.
Quarters of Coverage each represent a three-month period of work while paying the FICA tax about 4 Quarters of Coverage are earned in a single year.
The Quarters of Coverage are units of measuring eligibility for Medicare coverage and Social Security benefits. This measurement determines both the level of monthly Social Security income benefits and whether Part A is premium-free.
To get Part A premium-free, one typically must have earned 40 quarters of coverage, or about 10 years of employment while paying payroll taxes. The 40 total Quarters of Coverage do not have to be earned over 10 consecutive years.
These quarters of coverage can be earned through ones own work history or the work history of a spouse, parent, or child.
Those who have not quite accrued 40 Quarters of Coverage can still join Medicare Part A at age 65, but it will require paying a premium.
Earning 30-39 credits sets the monthly premium for Part A in 2021 at $259, and having earned less than 30 credits sets the Part A premium at $471.
In 2021, the Medicare Part B premium for most people is $148.50.
Read Also: How Much Is Medicare B Cost
