How Much Skilled Nursing Does Medicare Pay For
Many of my clients will call when faced with the possibility of going into a skilled nursing facility. Illness is scary enough. You dont want to worry about overwhelming medical bills. My people want to know theyre covered. They want to know how much skilled nursing does Medicare pay for. Do Medicare Advantage plans cover skilled nursing facilities? Do Medicare Supplements cover skilled nursing facilities? So, the big question is: who pays?
How Can I Find A Medicare
You can call Medicare to find out about Medicare-certified skilled nursing facilities in your area. Call Medicare at 1-800-MEDICARE and speak with a counselor they answer the phones 24 hours a day, seven days a week, except on certain federal holidays. Or you can visit Medicares web site at Medicare.gov to search and compare skilled nursing facilities. At this web site you may also want to read the guide to choosing a nursing home and/or the checklist of questions to ask when you are visiting skilled nursing facilities.
Can I help you further with your questions about skilled nursing facilities or your options when it comes to Medicare coverage? You can use the links below to schedule a phone appointment or have me email personalized information to you. If you would like to compare plans on your own, you can use the Compare Plans or Find Plans buttons on this page.
New To Medicare?
Becoming eligible for Medicare can be daunting. But don’t worry, we’re here to help you understand Medicare in 15 minutes or less.
Skilled Nursing Facilitys Legal Obligations
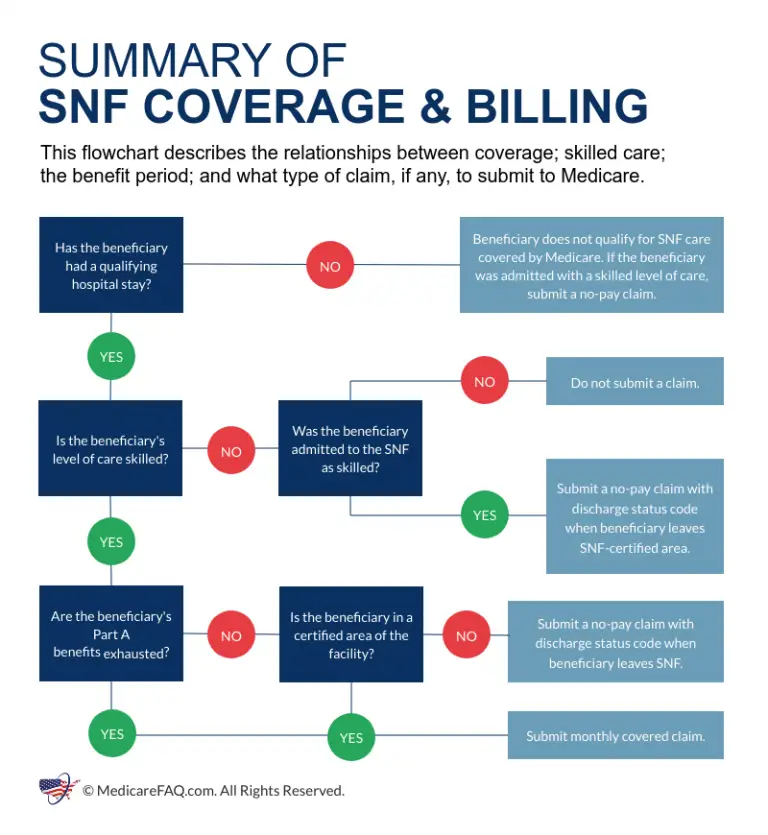
When a patient leaves a hospital and moves to a nursing home that provides Medicare coverage, the nursing home must give the patient written notice of whether the nursing home believes that the patient requires a skilled level of care and thus merits Medicare coverage. Even in cases where the SNF initially treats the patient as a Medicare recipient, after two or more weeks, often, the SNF will determine that the patient no longer needs a skilled level of care and will issue a Notice of Non-Coverage terminating the Medicare coverage.
Whether the non-coverage determination is made on entering the SNF or after a period of treatment, the patient can submit or not to Medicare. The patient should always ask for the bill to be submitted. This requires the nursing home to submit the patients medical records for review to the fiscal intermediary, an insurance company hired by Medicare, which reviews the facilitys determination. The review costs the patient nothing and may result in more Medicare coverage. While the review is being conducted, the patient is not obligated to pay the nursing home. However, if the appeal is denied, the patient will owe the facility retroactively for the period under review.
Read Also: Which Insulin Pumps Are Covered By Medicare
Skilled Nursing Facilities Rules More Complex
The rules involving Medicare and nursing homes or skilled nursing facilities are more complex.
Original Medicare and Medicare Advantage will pay for the cost of skilled nursing, including the custodial care provided in the skilled nursing home for a limited time, provided 1) the care is for recovery from illness or injury not for a chronic condition and 2) it is preceded by a hospital stay of at least three days.
For the first 20 days, Medicare will pay for 100% of the cost. For the next 80 days, Medicare pays 80% of the cost. Skilled nursing beyond 100 days is not covered by Original Medicare.
Individuals who have a Medicare Advantage plan have at least the same coverage as mentioned above, and perhaps, have additional coverage. In addition, persons with certain types of Medicare supplemental insurance can get additional assistance towards defraying the cost of nursing home/skilled nursing care. Some plans will cover 100% of the coinsurance payment required by Medicare. This means that between Medicare and the Medigap plan, 100% of the cost of skilled nursing for 100 days will be covered.
Skilled Nursing Care Vs Custodial Care
An important aspect to understand about Medicare nursing home coverage is the difference between skilled nursing care and custodial care.
- Skilled nursing care refers to the duties that can only be performed by a licensed professional, such as physical therapy, medicine shots, medical evaluations and other types of treatment. Skilled care provided in a skilled nursing facility is covered by Medicare. Custodial care may also be covered is a Medicare, but only if the beneficiary is also receiving skilled nursing care.
- Custodial care, or personal care, refers to assisted living tasks such as bathing, dressing, eating, toileting and moving from a bed to a chair or to other parts of a room or home. If you stay in an assisted living center or a nursing home and custodial care is the only type of care you need, Medicare wont cover the costs of your care. Many nursing home stays may involve custodial care, and those services not covered by Original Medicare .
Its important to note that some Medicare Advantage plans may cover more services than Original Medicare covers. If you have a Medicare Advantage plan, be sure to check with your plan carrier directly to find out if your plan offers any nursing home care coverage or assisted living benefits.
You May Like: Is Shingrix Vaccine Covered By Medicare
A Premiums Deductibles & Coinsurance
The chart below lists the Part A premiums, deductibles and coinsurance for inpatient hospital and skilled nursing facility care for Original fee-for-service Medicare. For a comprehensive list of Part A and B costs, see our summary chart, Medicare Benefits & Cost-Sharing for 2022
Part A Hospital Insurance Premiums, Deductibles & Coinsurance
| If You Have |
|---|
What Skilled Nursing Services Will Medicare Cover
The nursing facility care and services covered by Medicare are similar to what is covered for hospital care. They include:
- a semiprivate room , or a private room if medically necessary
- all meals, including special, medically required diets
- regular nursing services
- special care units, such as coronary care
- drugs, medical supplies, treatments, and appliances provided by the facility, such as casts, splints, wheelchair, and
- rehabilitation services, such as physical therapy, occupational therapy, and speech pathology, provided while you are in the nursing facility.
Costs for staying in a skilled nursing facility for the first twenty days are covered 100% after that, there is a co-pay .
You May Like: How Much Is Medicare B
Getting Help With Long
In addition to Medicare Advantage and Medigap plans, there are a number of public and private programs to help pay for skilled nursing costs. A few examples include:
- PACE , a Medicare/Medicaid program that helps people meet healthcare needs within their community.
- Medicare savings programs, which offer help from your state to pay your Medicare premiums.
- Medicares Extra Help program, which can be used to offset medication costs.
- Medicaid, which may be used to help fund long-term care needs, if youre eligible.
A few last tips
- If you think you may need skilled nursing care after a hospital stay, talk to your doctor early.
- Make sure you are listed as an inpatient, not an observation patient, during your admission.
- Ask the doctor to document any information that would prove skilled nursing care is necessary for your illness or condition.
- Consider hiring a
How Does Skilled Nursing Care Work
Medicare will pay for inpatient care at a Medicare-certified skilled nursing facility if you meet all these criteria:5
- You have Medicare Part A and days left in your benefit period .
- You were admitted as an inpatient at a hospital and stayed for three or more qualifying calendar days. Outpatient and observation days do not count. The three days start the day the hospital admits you as an inpatient the discharge day does not count.
- You enter the skilled nursing facility within 30 days of being discharged from the hospital.
- A doctor ordered skilled nursing care for you that requires qualified personnel to administer or supervise it.
- You need specialized daily care you can only receive at a skilled nursing facility as an inpatient.
- You need follow-up care for a medical condition treated during your hospital stay. The condition can differ from the original reason for admission.
- The skilled services your doctor prescribed are reasonable and necessary for the diagnosis or treatment of your condition.
Some common reasons why a beneficiary may go to a nursing facility and not meet all criteria for Medicare payment are:
- they were not formally admitted in the hospital as an inpatient, but were there under observation, which does not count towards a qualifying hospital stay
- they counted their discharge date as one of the three days required for the hospital stay or
- they waited longer than 30 days from their hospital discharge to enter the nursing facility.
Recommended Reading: Are Chemotherapy Drugs Covered By Medicare
Ensuring Medicare Will Pay For Senior Rehab
There is so much room for interpretation surrounding the rules for Medicare coverage that it is easy for families to become confused on how to pay for care in SNFs. The bottom line is that vigilance and advocacy are necessary to ensure that aging loved ones receive the skilled care they need and the coverage they are entitled to.
Family caregivers must make sure that the hospital staff and SNF staff give detailed orders and reasons for the skilled services that are needed to promote their loved ones health and safety. Carefully tracking the days within a benefit period can be confusing, but this is essential to prevent surprises regarding non-coverage.
Hiring a geriatric care manager to track the nursing home chart and timeline and accompany you to care plan meetings may be a wise investment. GCMs have a great deal of experience with seniors, various types of elder care providers and Medicare. Even if your loved one has run out of Medicare coverage during their benefit period, a GCM can help you find and access other sources of financial assistance and alternative types of care.
Read:Geriatric Care Managers Can Help Busy Caregivers
Medicare Part A Covers
- Certain care in a skilled nursing facility
- Certain home health services
- Certain hospice care
You will not pay a Part A monthly premium if you are eligible for Social Security retirement benefits or Railroad Retirement benefits. If you have 30-39 quarters of Social Security credits, you may buy Part A coverage and pay a monthly premium of $274 in 2022. If you have 0-29 quarters of Social Security credits, you may buy Part A coverage and pay a monthly premium of $499 in 2022.
Recommended Reading: How Do I Apply For Medicare At Age 65
Does Medicaid Cover Nursing Homes
Medicaid is a means-tested program, which people must meet strict financial eligibility requirements to qualify. If your income drops below the qualifying mark and you are accepted into the program, Medicaid will cover 100% of your nursing home expenses at a Medicaid-approved facility.
Although there are some exceptions to the rule to protect the livelihood of a spouse, Medicaid generally begins paying for nursing home care once your assets fall below $2,000. Individual eligibility requirements vary based on your age, marital status and home state, so check with your local Medicaid office to learn more and apply for benefits.
What Is A Skilled Nursing Facility
Skilled care is nursing or therapy services that must be performed by or supervised by a professional. This may include wound care, physical therapy, giving IV medication, and more.
Skilled nursing facilities can be located within hospital units, but these are the minority. Most skilled nursing facilities are stand-alone, private, for-profit businesses. They usually provide many types of services, such as short-term medical care, rehabilitation, and long-term care.
Tip
Medicare offers an online tool to help you find approved skilled nursing facilities. Case managers and social workers can also help you with coverage for your hospital or skilled nursing facility stay.
You May Like: Does Medicare Cover Nerve Blocks
How Much Will Medicare Cover
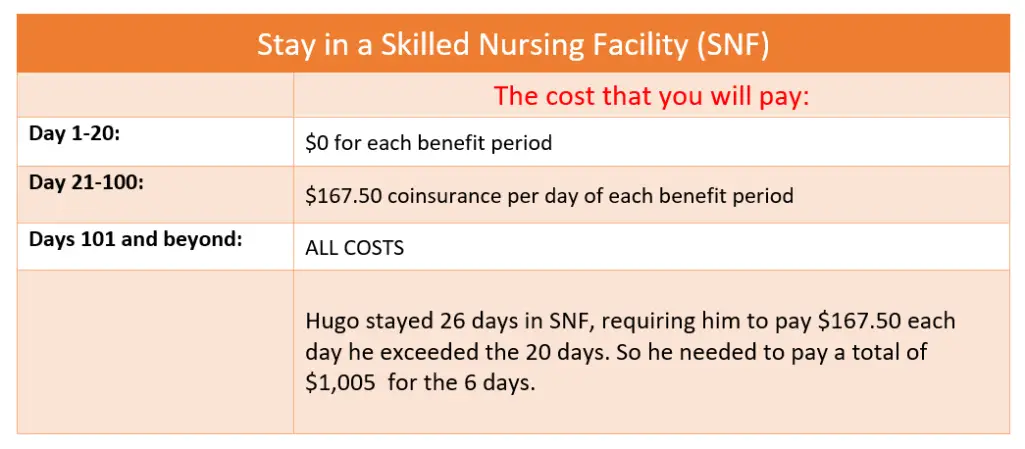
Medicares coverage for skilled nursing facilities is broken down into benefit periods. A benefit period begins the day you are admitted as an inpatient to the hospital or skilled nursing facility.
Different amounts are paid throughout the benefit period. The benefit period ends when 60 days in a row have passed without a need for hospital or skilled nursing care. If you go back to the hospital after that 60-day window, a new benefit period begins.
Here are the costs that apply throughout the benefit period:
- Days 1 through 20: Medicare covers the entire cost of your care for the first 20 days. You will pay nothing.
- Days 21 through 100: Medicare covers the majority of the cost, but you will owe a daily copayment. In 2020, this copayment is $176 per day.
- Day 100 and on: Medicare does not cover skilled nursing facility costs beyond day 100. At this point, you are responsible for the entire cost of care.
While you are in a skilled nursing facility, there are some exceptions on what is covered, even within the first 20-day window.
There are some additional rules about Medicare coverage that you should know, including:
Does Medicare Advantage Cover Nursing Homes
Medicare Advantage plans partially cover Skilled Nursing facility care but leave you with a daily coinsurance, and, possibly, a hospital deductible. Good news with Medicare Advantage is some plans dont require a 3-day inpatient qualifying stay. Medicare Advantage does not cover Long Term Care.
Remember Medicare Advantage plans are not standardized, so you will have to research all plans to learn what your SNF coinsurance and deductible would be.
For further questions please call to speak to a Senior65 agent at 800-930-7956.
Related Articles:
- Medigap Under 65 State Rules Americans under 65 are able to enroll in Medicare due to disability or ESRD . Some states require that you need to receive disability benefits for at least two years before you can enroll in Medicare. If you qualify for Medicare then you MAY also be
- Part D Overview If you are already familiar with how Medicare works, you know that it does not cover prescription drugs. Throughout this article we will explain how to get this sorted out easily.
- Medicare and Your Situation Original Medicare is our countrys health insurance program for people aged 65 or older. Medicare is also available to people under 65 with certain disabilities, and people of any age with End-Stage Renal Disease . The program helps with the cost of health care, but it does not cover all medical
Also Check: How Much Copay For Medicare
Medicare Coverage For Inpatient Rehabilitation
Medicare Part A covers medically necessary inpatient rehab care, which can help when youre recovering from serious injuries, surgery or an illness. Inpatient rehab care may be provided in of the following facilities:
- An inpatient rehabilitation facility
- Acute care rehabilitation center
- Rehabilitation hospital
For inpatient rehab care to be covered, your doctor needs to affirm the following are true for your medical condition:
1. It requires intensive rehab
2. It needs continued medical supervision
3. It needs coordinated care from your doctors and therapists working together
Medicare will cover your rehab services , a semi-private room, your meals, nursing services, medications and other hospital services and supplies received during your stay. Medicare wont cover private duty nursing, a phone or TV, personal items or a private room .
When Will Medicare Pay For Skilled Nursing Care
Medicare Part A covers the cost of a skilled nursing facility for conditions that begin with a hospital stay and require ongoing care after discharge. While this seems simple, there are a few specifics conditions that apply, including:
- Your illness or injury must require a hospital stay. Some examples of these events are a fall, stroke, heart attack, pneumonia, worsening heart failure or chronic obstructive pulmonary disease , or surgery.
- There is a required length of stay. The initial hospital stay must last a minimum of 3 days.
- While in the hospital, you must be considered an inpatient. Being in the hospital under observation is not considered a qualifying hospital stay. Time spent in the emergency department, under observation, and the day of discharge cannot be counted toward Medicares 3-day rule.
- When discharged, your doctor must order ongoing care. This means that you require 24-hour care at a skilled nursing facility for the condition for which you were hospitalized.
- You are covered for any conditions you develop while at a skilled nursing facility. An example of this could be if you get an infection while receiving rehab services after joint replacement surgery.
You May Like: Does Medicare Cover Knee Injections
How Many Days Does Medicare Pay For A Skilled Nursing Facility
100 days
Keeping this in consideration, what does CMS stand for in nursing?
circulation, motion, sensation
What does CMS stand for in healthcare?
Health Care
What does CSM stand for in nursing?
| CSM | Candice Selesha And Monica Miscellaneous » Unclassified |
|---|---|
| CSM | Carroll Shelby Motors Miscellaneous » Unclassified |
| CSM | Circulation, Sensation, and Movement Medical » Nursing |
| CSM | Congestion State Machine Miscellaneous » Unclassified |
| CSM | Circulation Sensation Movement Miscellaneous » Unclassified |
Readmission Within 30 Days
When the beneficiary is discharged from a skilled nursing facility, and then readmitted within 30 days, this is considered readmission. Another instance of readmission is if a beneficiary were to be in the care of a Skilled Nursing Facility and then ended up needing new care within 30 days post the first noncoverage day.
Don’t Miss: Does Medicare Pay For Insulin Pumps
