What Are The Negative Effects Of Prior Authorization
- Perhaps the most significant negative effect is that prior authorization delays patient access to care. It adds a speed bump to the patient journey, and can lead some patients to forgo treatment.
- In fact, 75% of physicians participating in an AMA survey reported that issues related to the prior authorization process can cause patients to abandon their recommended course of treatment. In that same survey, 28% of physicians reported that preauthorization has led to a serious adverse event for a patient in their care.
- The administrative burden from prior authorization distracts clinicians from practicing medicine and contributes to the growing epidemic of physician burnout.
- The unstructured and unpredictable nature of preauthorizations can wreak havoc on the normal administrative workflow of a practice. In fact, many practices have to add or repurpose staff expressly to deal with prior auths. These inefficiencies and the additional overhead required to deal with them can strain already dwindling margins and overextend office personnel.
Sometimes prior authorization requirements are not determined until after treatment is complete. This results in payers withholding some or all of an expected reimbursement. If this is the case, providers will often have to pursue payment from patients directly, a strategy that often results in practices writing off uncollectible revenue as bad debt.
License For Use Of Physicians’ Current Procedural Terminology Fourth Edition
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials including but not limited to CGS fee schedules, general communications, Medicare Bulletin, and related materials internally within your organization within the United States for the sole use by yourself, employees, and agents. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services . You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized here in must be obtained through the AMA, CPT Intellectual Property Services, 515 N. State Street, Chicago, IL 60610. Applications are available at the AMA website.
Adhere To The Guideline Provided For Submission
Your prior authorization request may not get approved if you fail to follow the plans instruction. Accordingly, you must meet the criteria specified in the plans policy before attempting to submit the PA form. In that regard, check to see that you tick every box before they take the form for submission.
Recommended Reading: When Can I Change My Medicare Prescription Drug Plan
Are There Exceptions Where A Prior Authorization Request Can Be Disregarded
Yes. Certain providers are exempt from prior authorization.
Some providers with a track record of high prior authorization approval rates are given gold card status and do not need to adhere to the same prior auth rules required of others. The same goes for hospitals and healthcare systems with marquee brand names that health plans covet for their networks. Emergency rooms and other trauma-based care are also exempt from prior authorization since the stakes are too high to wait for payer approval.
Does Medicare Require Prior Authorizations
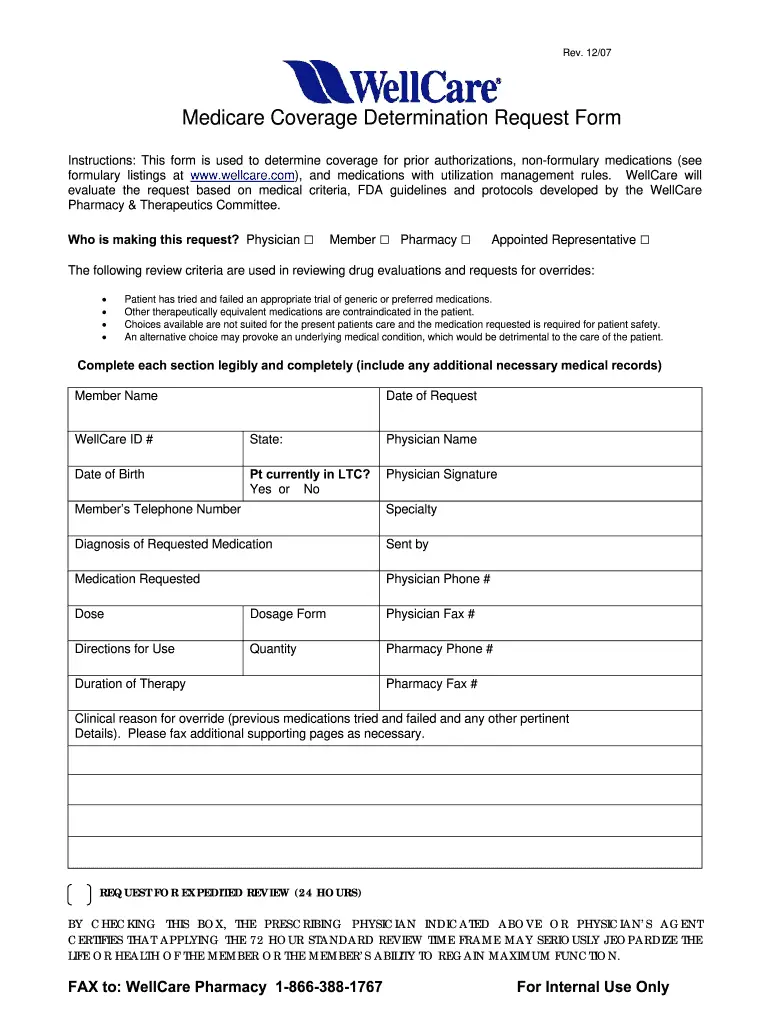
Beneficiaries with Original Medicare generally do not need to obtain a prior authorization form for most Medicare services, such as doctors visits, hospitalizations, diagnostic studies or treatments.
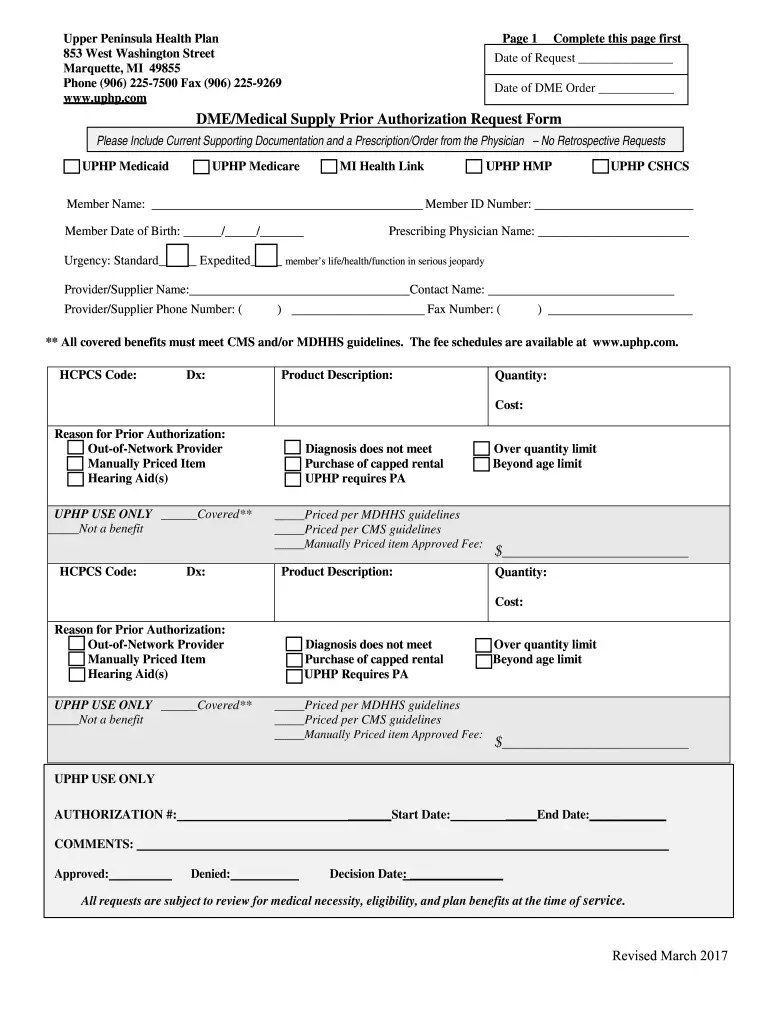
Original Medicare beneficiaries may sometimes need to seek prior authorization for durable medical equipment and certain types of Medicare outpatient services.
Its not uncommon, however, for beneficiaries of Medicare Advantage plans and Medicare Part D Prescription Drug plans to need prior authorization before receiving some types of care.
Prior authorization is most common for getting certain prescription drugs covered by your plan. You may also need a prior authorization form if youre seeking care from an out-of-network provider.
Also Check: When Can You Start Collecting Medicare
Submit Thorough And Accurate Info
When you submit a prior authorization request, make sure the information you submit is totally accurate and is thorough. Prior authorization requests can be denied or delayed because of seemingly mundane mistakes.
A simple mistake could be having the request submitted for a patient named John Appleseed when the health plan members health insurance card lists the members name as Jonathan Q. Appleseed, Jr.
A computer may be the first person processing your request. If the computer is unable to find a health plan member matching the information you submit, you could be sunk before youve even started.
Likewise, it may be a computer that compares the ICD-10 diagnosis codes with the procedure CPT codes your healthcare provider submits in the prior authorization request, looking for pairs that it can approve automatically using a software algorithm.
If those codes are inaccurate, a request that might have been quickly approved by the computer will instead be sent to a long queue for a human reviewer to analyze. Youll wait another few days before you can get your mental health services, your prescription drug, or your MRI scan.
If youre having trouble getting prior authorization or have had a prior authorization request denied, ask to see exactly what information was submitted with the request.
With clinical information that doesnt match your request, youre unlikely to have your prior authorization request approved.
Medicare Part D Prior Authorization
Often, even top Part D prescription drug plans need prior authorization for coverage on specific drugs. Different policies have varying rules, so youll need to contact the carrier directly to confirm coverage.
Most Part D plans have forms you can download online. The online option is a useful way to print the documents and take them to your doctor. Your doctor can help you correctly complete the form.
Also, recipients may directly contact their Part D plan and ask for a mail-in form. You can find the number for Member Services on your plans member ID card.
Don’t Miss: What Is A 5 Star Medicare Plan
When Claims Are Denied For No Authorization
Even as billers work diligently to reduce claims denials, payers are expanding the number of visit types and procedures that require prior authorizationleading to an upswing in denials for some practices. It is estimated that 80% of denied claims have to do with no authorization being obtained, or authorizations being requested improperly.
Still, there are types of medicine, such as emergency medicine, that routinely see claims denied for lack of prior approval. So, in the case where no authorization was filed, what is the next step?
Many payers require authorization for services prior to or within fourteen calendar days of services rendered. Requests for approval filed after the fact are referred to as retroactive authorization, and occur typically under extenuating circumstances and where provider reconsideration requests are required by the payer. Similarly, personal injury and hospital billers routinely file incomplete claims to meet timely filing, knowing they will be denied, and knowing they will appeal them later.
Submit New Prior Authorization Request
Part A users may submit a request for a new Prior Authorization request by completing and uploading the Prior Authorization coversheet. As of June 17, 2020, Prior Authorizations are only required for certain Hospital Outpatient Department services.
| Services | |
|---|---|
| Blepharoplasty, Eyelid Surgery, Brow Life and related services | 15820 – 15823, 6790 – 67904, 67906, 67908, 67911 |
| Botulinum Toxin Injection | |
| Cervical Fusion with Disc Removal | 22551, 22552 |
| Panniculectomy, Excision of Excess Skin and Subcutaneous Tissue and related services | 15830, 15847, 15877 |
| 20912, 21210, 30400, 30410, 30420, 30430, 30435, 30450, 30460, 30462, 30465, 30520 | |
| Vein Ablation and related services | 36473 – 36476, 36478, 36479, 36482, 36483 |
Choose Prior Authorizations from the Main Menu and then the Submit New Prior Auth Tab.
- Select the Provider/Supplier Details
Once the request has been submitted, a Reference Number will be provided. Additional supporting documentation may be uploaded after 15 minutes to allow the initial request to process.
You May Like: Which Medicare Plans Cover Silver Sneakers
Revise And Finalize Proposed Rule
As a result of the administrative and clinical difficulties caused by inefficient prior authorization processes, hospitals and other providers were pleased that CMS took action to streamline prior authorization through the Reducing Provider and Patient Burden by Improving Prior Authorization Processes and the Promoting Patients Electronic Access to Health Information notice of proposed rulemaking released in December 2020. If finalized, the regulation would create a standardized method to identify whether a procedure was subject to prior authorization, submit prior authorization and supporting documentation, and receive a determination from the health plan. Additionally, the regulation recognized the need to reduce the amount of time that prior authorizations take to process.
The proposed rule would place new requirements on Medicaid and Children’s Health Insurance Program managed care plans, state Medicaid and CHIP fee-forservice programs, and Qualified Health Plan issuers on the Federally-facilitated Exchanges , while also indicating that Medicare fee-for-service will be adhering to the requirements. The notable exclusion of MAOs is extremely troubling and significantly reduces the potential impact of the regulation.
Ama Disclaimer Of Warranties And Liabilities
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CGS or the CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Also Check: Can You Apply For Medicare After 65
The Way To Fill Out The Coventry Prior Authorization Phone Number Form On The Web:
By utilizing SignNow’s complete platform, you’re able to carry out any essential edits to Coventry prior authorization phone number form, generate your personalized digital signature in a couple quick actions, and streamline your workflow without the need of leaving your browser.
Create this form in 5 minutes or less
Why Is Prior Authorization So Complex
The prior authorization process is often complicated by a combination of factors, including:
- Lots of required steps, each introducing the potential for delays and errors.
- Participation by both payers and providers, each of whom have different motivations, workflows, and infrastructure.
- Lack of standards, particularly when it comes to payer rules.
- Fluctuating payer rules which need to be constantly monitored and revised.
- Thousands of payers and health plans.
- Manual review of prior auth requests and medical charts by clinicians.
Don’t Miss: Will Medicare Pay For Drug Rehab
Is The Occurrence Of Prior Authorization Increasing
Yes.
The volume of medical procedures and prescribed medications requiring prior authorization is increasing significantly. This is driven largely by insurance companies searching for ways to control spiraling healthcare costs, especially those associated with innovative new specialty drugs or emerging technologies. While these medications or services can demonstrably improve patient outcomes, they usually come with outsized costs and are often too new to have a proven track record. This is especially true of specialty pharmacy drugs that are patent protected.
The American Medical Association has projected that use of prior authorization for prescription drugs will increase 20% per year.
End User Point And Click Agreement
You, your employees, and agents are authorized to use CPT only as contained in the following authorized materials internally within your organization within the United States for the sole use by yourself, employees, and agents. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services . You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized herein must be obtained through the AMA, CPT Intellectual Property Services, 515 N. State Street, Chicago, IL 60610. Applications are available at the AMA Web site, .
Applicable FARS/DFARS restrictions apply to government use.
U.S. Government Rights
Also Check: Does Medicare Pay For Breast Reconstruction
Minimize The Administrative Burden
In order to manage prior authorizations, physicians andinstitutions can initiate certain steps to lessen the burden. Providers shouldalways keep up with the ever-changing clinical guidelines on every diseasestate since insurance companies also update the need for prior authorizationsbased on these guidelines. Ordering prescriptions outside of normal practiceoften results in the need to submit a prior authorization to the patients plan.It can also be beneficial to create lists of medications and procedures thatare covered by each plan. Furthermore, these lists can be incorporated into theelectronic health record to alert physicians when they order something thatrequires a prior authorization. Being familiar and keeping up to date withinsurers policies and formularies can reduce patient delay of care.
If possible, designating and educating certain members of the staff to handle prior authorizations requests may be beneficial to reduce time physicians spend on the phone with insurers. These designated staff members will become more knowledgeable and efficient in handling prior authorizations over time. There are great benefits to having a Prior Authorization Certified Specialist on staff to help with the administrative process.
The prior authorization process can be navigated easily andefficiently with the right resources and staff to help in the process. Trainedprofessionals can make the process seamless, especially when they document and maintainrecords.
How Does Prior Authorization Work
The process of getting prior authorization begins with the patients and ends with the health insurance companies. However, the physicians come in between, and they play a critical role in the approval of a PA.
Prior authorization can be prescription, medical, or alternative services that patients health plans do not cover. In that case, it becomes necessary to inform the insurance companies for proper processing.
It begins with a medical prescription to a patient by the health practitioner. On getting to the pharmacy, you call the pharmacists attention to the prior authorization status of the medication. The doctor will receive notification of the PA status to initiate the procedures.
In terms of medical service not covered by health plans, it begins with a conversation between two parties. The doctor will start a conversation with the insurance company. This is to notify them of the prior authorization clause on the medication. This notification will proceed to the filling of forms to reach an agreement for the prior authorization.
Recommendation of close substitute drugs or medical devices within the health plans also follows the same process. Sometimes, your insurance company suggests you begin with an inexpensive medical service. The reason is to determine if your health condition will improve without having to overspend.
Don’t Miss: Who Is Eligible For Medicare In Georgia
Do I Need Prior Authorization
You might be thinking, How will a prior authorization affect me? Does that mean my surgery wont be covered if my plan doesnt think it is necessary?
If your healthcare provider does not correctly code your service bill or file necessary prior authorizations on why you need this procedure, your plan will likely not provide coverage. There are physicians out there who have recognized this crisis.
According to a report conducted by Beckers Hospital CFO, out of 1,000 practicing physicians:
- 94% stated the prior authorization process delays patients access to the necessary care they need
- 39% stated prior authorizations often delay access to essential care, and 15% stated that it ALWAYS does
- 90% said prior authorizations have a negative effect on patients clinical outcomes
It is important to note that prior authorizations are not necessary during an emergency. Procedures during an emergency will often be viewed as medically necessary which drops the need for this request.
The need for prior authorization with Medicare will ultimately come down to the question of necessity. Is your procedure or service very clearly medically necessary under Medicares standards? You may not need a prior authorization. Is there any gray area on whether Medicare or the insurance carrier would question the medical necessity? You likely need prior authorization.
