The Major Challenges Of Chronic Care Management
Research has shown, however, that patients who are very sick tend to be less engaged in their care. A lack of engagement prevents patients from being able to manage their health. Therefore, a focus on self-care and self-management is more appropriate when a persons conditions and circumstances allow them to self-manage their health.
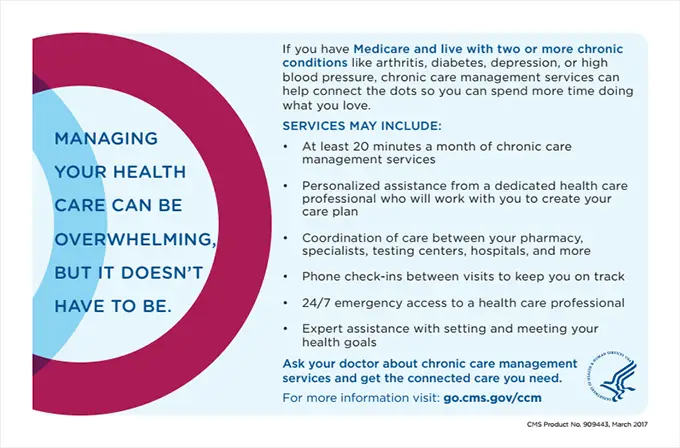
Both patient and medical care provider face many challenges in chronic care management. As the number of chronic conditions increases in a person, the risk of mortality, hospitalization, and medication interaction increases. Multiple chronic conditions directly contribute to disability. Patients with multiple chronic conditions usually require more extended, more in-depth, and more frequent doctors visits than is typical for acute care. Careful coordination of medical professionals is needed as well, or else fragmentation of care is a risk. Patients with multiple chronic conditions have a higher chance of receiving conflicting advice from their health care providers. Frequently, treatments for chronic conditions and diseases are complicated, making it difficult for patients to comply with the treatment protocol.
Increased spending on chronic disease among Medicare beneficiaries is a key factor in driving the overall increase in spending in the Medicare program.
Humana Telephonic Case And Care Management Programs
Humana offers a variety of programs for patients who need care for complex medical situations or support for chronic conditions. Through these programs, care managers collaborate with physicians and other healthcare professionals to help patients manage their healthcare needs while addressing their physical, behavioral, cognitive, social and financial needs.
Benefits Of Chronic Care Management Program
People who participate in the Chronic Care Management program were 2.3% less likely to need emergency room or observation care in the hospital, according to one evaluation. Their risk for inpatient hospitalization decreased by 4.7%.
Specifically, hospitalizations related to congestive heart failure, dehydration, diabetes, and urinary tract infections were statistically reduced. People also reported being more satisfied with their care.
Overall, the Chronic Care Management program saves Medicare $74 per patient per month or $888 per patient per year. These savings were attributed to the decreased need for more expensive services and improved efficiencies in care.
With more than 61.2 million people on Medicare in 2020 , and half of them having two or more chronic conditions, there are billions of dollars in potential savings for Medicare. More importantly, the improvements in care have a real impact on quality of life.
You May Like: Does Medicare Cover Skin Removal
How Do I Get Paid What Is The Coding & Billing Process
Detailed documentation has always been important for coding and billing, but its critical if you want to obtain CCM reimbursement.
You must:
- A document that clinical staff spent 20 minutes of non-face-to-face time in a given month.
- Record the date, time spent, name of the provider, and the services provided.
- Bill Medicare using CPT code 99490. This should be billed only once per month per participating patient.
- In addition to billing 99490, the CPT codes for the chronic conditions should also be included.
The non-face-to-face time should never be rounded up. Documentation should note the time spent in total minutes. For example, clinical staff would document four minutes and not 10:04 to 10:08.
Also, be mindful of not falling into recording the same number of minutes every time. While it may be easier to document in 5-minute intervals, precision and accuracy is crucial. Every service recorded as 5 minutes is not realistic. In the event of an audit, this type of documentation would not be favorable. Record the actual time spent.
CPT Code 99490 is subject to cost-sharing, including the patients deductible, co-pay, and co-insurance. That should be clearly explained in the patient consent as well.
Some medical practices have found that the creation of an internal log may be helpful in tracking the time spent with CCM patients.
Should You Enroll In Chronic Care Management
The CCM program has a lot to offer, but it is not free. The time your healthcare professional spends coordinating care each month and reviewing your records will be billed to Medicare.
The time spent on these services must be a minimum of 20 minutes, which is, on average, the amount of time they would normally spend with you in a face-to-face office visit.
Chronic Care Management services cost approximately $42 per month, though prices may vary based on where you live. Medicare reimburses the physician 80%, and you will pay a Part B 20% coinsurance. On average, that would be $8.40 each month.
Your provider may charge more if they spend more time on your care, up to an hour, or if the care is more complicated.
Many Medicare beneficiaries are on fixed incomes and may not be able to afford this monthly charge. Whats important to know in these and all cases is that your healthcare professional cannot sign you up for these services without your permission.
If you have a Medicare supplement plan, also known as a Medigap plan, it may pay your Part B coinsurance for you. Likewise, if you are eligible for certain Medicare Savings Programs, you will not need to pay out of pocket for these services.
You May Like: How Many Parts Medicare Has
What Are Chronic Conditions
The Centers for Disease Control and Prevention defines a chronic condition as any condition that has been ongoing for more than one year and requires prolonged medical care. Chronic conditions are also defined as those that limit the patients ability to perform basic activities of daily living . Activities of daily living include eating , bathing, dressing, toileting , transferring , and the ability to maintain continence .
The Center for Medicare and Medicaid Services has identified the list below as chronic conditions. Along with these medical conditions, Urologic chronic conditions include Benign Prostatic Hyperplasia , overactive bladder , bladder cancer, renal cancer, prostate cancer, ureter cancer and renal pelvis cancer.
CMS list of chronic conditions
- Alzheimers disease/Dementia
- Chronic obstructive pulmonary disease
- Depression
- Hyperlipidemia
- Hypertension
- Ischemic heart disease reduced blood flow due to plaque build-up in the arteries
- Osteoporosis
- Schizophrenia and other psychotic disorders
- Stroke
What Is The Research About
People with diabetes often have other health problems such as high blood pressure, high cholesterol, or liver disease. Having more than one disease can make them all more difficult to manage. Patients often need multiple medicines to control their health problems. Healthcare providers may need to spend extra time planning care for these patients, working with their other doctors, and following up with patients online or by phone. Time spent planning and coordinating care outside of regular office visits for patients with several health problems is called chronic care management. Starting in 2015, providers can get paid for the time they spend managing Medicare patients care needs outside of normal office visits. Because this change is recent, researchers dont know how hard or easy it is for providers to deliver these types of services. Researchers also dont know whether paying providers for these types of services results in better health for patients with diabetes who also have other health problems.
Also Check: What Are The Costs Of Medicare Advantage Plans
Taking The Next Steps
Once you turn 65, youre able to apply for Medicare online. You can enroll in Medicare Advantage during this time or during Medicares Open Enrollment Period, which runs from October 15 through December 7 every year. The CHRONIC Care Acts changes to Medicare Advantage take effect this year so now is the time to think about your coverage in the future.
When Can I Enroll In A Medicare Chronic Care Management
You can enroll in CCM anytime after youve enrolled in Medicare Part B or a Medicare Advantage Plan. You cant be enrolled in a CCM if youre only enrolled in Medicare Part A. Medicare has several rolling enrollment windows every year that allow you to make changes to your plan and benefits.
Initial Medicare enrollment occurs around your 65th birthday. You can enroll as early as 3 months before the month of your birthday or as late as 3 months after. Youll have to pay a late enrollment fee if you wait longer. You can enroll in Medicare before you turn 65 if you have a disability and have been receiving Social Security for two years.
Don’t Miss: How Much Does Medicare Pay For Physical Therapy In 2020
Patient Agreement And Consent
Medicare wants to make sure patients understand prospective medical services as well as the financial implications, prior to receiving treatment. With CCM, this is no different and is carried out via specific patient agreement requirements.
The patient agreement is similar to an advanced beneficiary notice, or ABN, and must be completed prior to the start of services.
CMS does not provide a standard form for this. Instead, each physician creates their own agreement, but at a minimum, it should:
- Inform the patient of CCM availability, and obtain written authorization for services. Authorization for the electronic communication of medical information should also be obtained.
- Explain the services as well as possible cost-sharing expenses. This discussion should be documented in the patients medical record, along with their decision to accept or decline the service.
- Explain how to revoke services. Generally, patients have the right to discontinue CCM services at any time by revoking the agreement, effective at the end of the current calendar month.
- Inform the patient of CCM billing limitations. The patient should understand that only one practitioner per calendar month may be reimbursed for the service.
The key here is to have everything clearly documented in the patients medical record, and ideally, within the patient agreement. Consents, revocations, and any changes in CCM services must be documented.
What Is The Impact For Primary Care Physicians
The program is still in its infancy but based on a survey of 45,000 American primary care physicians who treat Medicare patients, 67.33% of respondents are unaware or not familiar with the program . More than 50% of respondents are planning to launch a CCM program in their practice within a year. The program does offer great financial incentive for care but some challenges include:
- Enrolling eligible patients
- Lack of staff/expertise to meet the 20 minutes monthly minimum for enrolled patients
- Maintaining an auditable record of time and tasks performed
- Meeting the electronic requirements
Physicians need to continue to enroll CCM patients into the program. Moving forward, it is clear that educating both the eligible patient population and the health care professionals on what is available will lead to increased enrollment and use of this program.
If you are an eligible Medicare patient that has two or more chronic conditions, speak with your physician today to explore the option of Chronic Care Management.
Also Check: Is Tresiba Covered By Medicare
Medicare Payments For Chronic Care Management
Chronic Care Management is defined as the non-face-to-face services provided to Medicare beneficiaries who have multiple , significant chronic conditions that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline. These significant chronic conditions are expected to last at least 12 months or until the death of the patient. CCM cannot be billed during the same service period as transitional care management, home health care supervision/hospice care, or certain end-stage renal disease services. Beginning January 1, 2015, Medicare paid separately for CCM under the Medicare Physician Fee Schedule and under the American Medical Association Current Procedural Terminology. We will determine whether payments for CCM services were in accordance with Medicare requirements.
| Announced or Revised |
|---|
What Is A Ccm

Any condition that meets the Medicare criteria can qualify a patient for CCM. Some of the most common examples include:
- Alzheimer’s disease
- Lupus
- Multiple sclerosis
There are other requirements that must be met to code, bill, and get paid for CCM. Learn about these rules and more in this comprehensive Chronic Care Management Coding and Billing Guide.
Also Check: Does Medicare Cover Oxygen At Home
Independence At Home Extension
The Independence at Home program provides primary care in the homes of Medicare beneficiaries with chronic disorders. With IAH, medical professionals visit patients homes to accommodate travel expenses. With the CHRONIC Care Act, IAH will expand its course to offer this home-based service to more individuals. 15,000 people nationwide will benefit from IAH through September 2019.1
Chronic Care Management At Urology Austin
Because Urology Austin understands the interaction of disease states, and the importance of providing top quality patient healthcare, we have established a new Chronic Care Management program for patients who have two or more chronic conditions and are covered by Medicare. Medicare patients who choose to participate, will receive a monthly phone call from a Care Team Coordinator to review and help manage their chronic conditions.
Care Team Coordinators work with our patients each month to:
- Assess their current conditions, symptoms, and medical care progress
- Answer patient questions about their medical conditions and treatments
- Review their current medications
- To ensure that patients are receiving medical attention in a timely manner
- To assist patients with transitioning their care to the necessary medical providers
- Assist patients with physician referrals and authorizations
- Ensure that their billing questions are answered
If you are a Urology Austin patient with chronic medical conditions who is covered by Medicare, call 512-212-7880 to learn more or to sign up for the Chronic Care Management program.
You May Like: Is Mutual Of Omaha A Good Medicare Supplement Company
How Can I Educate Patients About Ccm And What To Expect
CCM requires patient consent be obtained, providing an opportunity to explain and engage the patient in the goals and activities of CCM. When obtaining patient consent, the patient should be aware of the 20% cost sharing requirement for each month of CCM service. Verbal or written consent must be documented in the EHR and include the following:
- CCM services are available and cost-sharing is applicable,
- Only one of the patients providers can provide and bill for CCM services each month, and
- The patient has the right to stop CCM services at any time.
Informed consent is only required once prior to initiating CCM services or if the patient chooses to change the billing provider for CCM services.
Examples of consent forms are available through the ACP’s Chronic Care Management Tool Kit.
What Does Chronic Care Management Include
When you consent to receive CCM, you may receive on or a few of a whole host of services that Medicare covers.
- First, a dedicated healthcare professional will work with you to develop a comprehensive care plan that includes your health problems and goals, other providers, medications, community services available near you and more.
- Once developed, they will share that care plan with you as well as all of your other providers to ensure timely, coordinated care.
- As part of the CCM, youll also receive phone or portal check-ins between visits to keep you on track. During these check-ins, youll review your medications and discuss how other changes in your life might affect your health, as well as what you need in terms of support to meet your goals.
With CCM, youll also receive help with care transitions, care coordination with home- and community-based providers and 24/7 access to your provider for urgent care needs. All in all, its at least 20 minutes of services each month designed to help you get the connected care you need.
Don’t Miss: Will Medicare Pay For Drug Rehab
No Cost For Most Patients
CCM and RPM services are covered by Medicare and most secondary insurances. That means if you have Medicare, and a secondary plan, you can enroll at no cost.
Get personalized attention from a Medical Assistant monthly, conveniently via a phone call or text message
Identify potential issues earlier and enable your doctor to respond more quickly
Easily let your doctor know about health changes, refills needed, or appointments youd like to schedule
Receive a personalized care plan tailored to your chronic conditions and medical history
Eligibility For Chronic Care Management
The Chronic Care Management program was created by Medicare to close those communication gaps. It also looks to give 24/7 access to care so that people with chronic conditions have better health outcomes.
To be eligible for the program, you must be enrolled in Medicare Part B and have two or more chronic conditions. Medicare defines these as conditions expected to last at least 12 months or, if you are at the end of life, as long as you live.
Those conditions put you at risk for disease complications, flare-ups, functional decline, or even death. Simply put, the disease affects your quality of life and is expected to get worse over time if not properly treated.
Also Check: When Can I Change My Medicare Prescription Drug Plan
The Evolution Of Chronic Care Management
Chronic care management is a relatively new branch of medicine. Beginning in the 1980s, members of the medical community began to try to understand and research chronic care and its phases and stages. Since then, there has been a significant effort in the development of treatments and research on understanding the physical and psychological effects on people suffering from chronic illnesses.
Chronic diseases affect approximately 133 million Americans or 40% of the total population of this country. By 2020, it is projected that the number will reach 157 million, with 81 million of those people having multiple conditions.
The supply and distribution of primary care health professionals will be insufficient to meet the needs of the growth in chronically ill patients. Increasing the role of registered nurses and recruiting more people into nursing may be part of the solution to the demand placed on health care as the number of people with chronic conditions increases.
As the number of Americans with chronic condition grows, so does the demand for chronic care management software.
