Do I Need To File Part D Claims
Medicare Part D plans contract with pharmacies where you can fill your prescriptions. Both preferred and non-preferred pharmacies can bill your Part D insurer, although your cost will be lower if you use a preferred pharmacy. If you have to fill medications at a pharmacy outside your plans network because of an emergency, you may be able to receive partial reimbursement by submitting your receipt and supporting documentation to your Part D insurer. Contact your insurer for instructions if you need to file an out-of-network claim.
You may also have to file a Part D claim if you receive medications while hospitalized that arent reimbursed by Medicare or your Medicare Advantage plans payment for your care. Whether you need to submit the claim yourself depends on whether the hospitals pharmacy has a contract with your Part D plan.
Time Frames To Submit A Claim
Please note the following time frames for submitting Medicare Advantage or commercial claims:
Medicare Advantage: Claims must be submitted within one year from the date of service or as stipulated in the provider agreement.
Commercial: Claims must be submitted within 90 days from the date of service if no other state-mandated or contractual definition applies.
If a claim is submitted in error to a carrier or agency other than Humana, the timely filing period begins on the date the provider was notified of the error by the other carrier or agency.
When Should I Be Filing A Claim For Myself
Another specific and unusual circumstance in which you may need to file a Medicare claim on your own is if your medical provider has not filed the claim within the appropriate timeline. Medicare claims are expected to be filed within 12 months of the original date of service. If the claim was not filed within this 12-month limit, Medicare will not pay their portion of the bill.
If you find that your claims are not being filed within the appropriate timeline, the first thing to do is contact your provider, whether it be a doctor or medical supplier, and request that they file the claim.
If they still do not file the claim, your next step would be to contact Medicare directly. If the time limit is coming to a close and it looks like they still may not submit the claim, you can then file it on your own.
Read Also: Does Medicare Pay For Eyeglasses For Diabetics
How To Get Reimbursed From Medicare
To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out. You can print it and fill it out by hand. The form asks for information about you, your claim, and other health insurance you have.
The itemized bill must contain the following information:
- Date of service
Disclaimer: By clicking the button above, you consent to receive emails, text messages and/or phone calls via automated telephone dialing system or by artificial/pre-recorded message from representatives or licensed insurance agents of Elite Insurance Partners LLC, its affiliates or third-party partners at the email address and telephone number provided, including your wireless number , regarding Medicare Supplement Insurance, Medicare Advantage, Medicare Part D and/or other insurance plans. Your consent is not a condition of purchase and you may revoke your consent at any time. This program is subject to our Privacy Policy and Terms of Use. This website is not connected with the federal government or the federal Medicare program.
Obtain An Itemized Bill For Your Medical Treatment
Your itemized bill or bills for medical treatment proves your claims validity. Make sure your itemized bill contains the following information to ensure your claim is processed smoothly:
- The date of your treatment
- The place you received treatment
- Your doctor or medical suppliers name and address
- Description of each surgical or medical treatment or supply received
- Itemized charge for each treatment or medical supply
- Your specific diagnosis. This may not be necessary on the itemized bill if your Patients Request for Medical Payment form contains a thorough illness or injury description
If the bill you received from your health care supplier doesnt contain these details, contact your physician and request a new one with all the information Medicare requires.
Also Check: What Does Cigna Medicare Supplement Cover
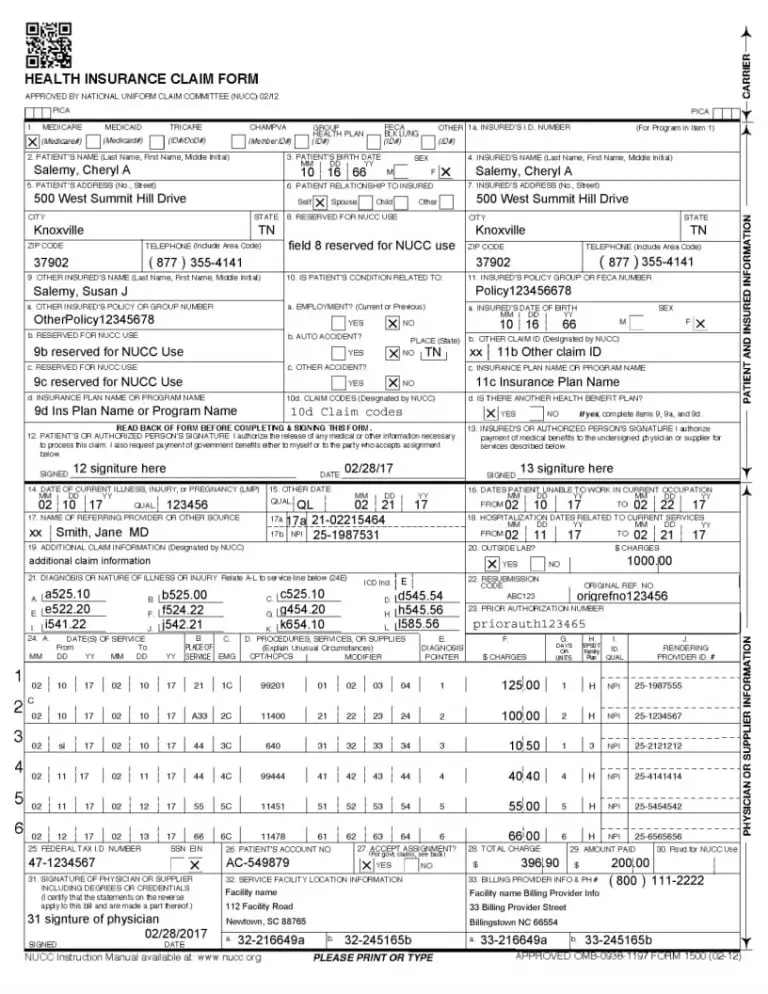
Billing Guidelines For Submitting A Roster Bill On A Paper Claim
Healthcare providers should follow the billing guidelines below when submitting roster bills to Humana:
- Healthcare providers can submit multiple documents in a single large envelope.
- Documents may include information regarding multiple patients.
- Healthcare providers can submit CMS 1500 forms or UB04 forms with an attachment listing multiple patients receiving the same service. The claim form should have the words “see attachment” in the “Member ID” box.
Please send a roster bill to the following address:
HumanaLexington, KY 40512-4601
Before You Submit A Claim
Payment of claims for MNT provided in the outpatient environment is dependent on several factors, including an individual’s benefits for MNT for their condition or reason , approved settings, and the network status of the RDN with the client/patient’s payer. Claims can be submitted to payers electronically through many vehicles, including practice management systems, provider portals, and claims clearinghouses. There may be some instances where paper claims are still used.
Read Also: Does Medicare Cover You When Traveling Abroad
When And How To File A Medicare Claim
July 14, 2021 / 6 min read / Written by Jason B.
Where you can go for health care, how much you will pay, and the process for filing a Medicare claim varies depending on how you get your Medicare coverage. Original Medicare, Part A and Part B, has different rules than Medicare Part C and Medicare Part D , where coverage is provided through Medicare-approved private insurance companies. Here are some guidelines for when you need to file an Original Medicare claim form and how to do it.
Medicare claims for Original Medicare
If you have Original Medicare, the amount you pay at the time you receive a health service will depend on whether your doctor is a Medicare-participating provider and accepts assignment. Medicare-participating providers are on contract with Medicare to accept assignment for all Medicare-covered services and supplies. A provider that accepts assignment agrees to accept the Medicare-approved amount as full payment for a covered service or supply. The Medicare fee schedule is a list of approved provider reimbursement rates set by the Medicare program for each service a doctor or hospital that accepts assignment will not charge you above the Medicare fee schedule . In this instance, the provider or supplier is required to file Medicare claims for any services you received, and Medicare will pay the provider directly for those services. The provider is not allowed to charge you to submit the claim.
When to file an Original Medicare claim
Options If You Have Medicare But Your Doctor Doesn’t Accept It
Not all doctors accept Medicare for the patients they see, an increasingly common occurrence. This can leave you with higher out-of-pocket costs than you anticipated and a tough decision if you really like that doctor.
So what happens when you sign up for Medicare only to learn it’s a no-go at your favorite medico? Fortunately, you have some options.
You May Like: When To Sign Up For Medicare Part D
How To: Submit Claims To Priority Health
For more information about billing and payment, including general claim requirements and service-specific billing information, visit the billing and payment section of our Provider Manual.
Avoiding The Need For Claims
Make sure that your doctor accepts Medicare assignment. For Original Medicare, Part A and Part B, this means that your doctor or provider agrees to be paid by Medicare, and that they accept the Medicare-approved amount for a particular service. When your doctor accepts Medicare assignment, it also means she or he agrees not to bill you for more than the Medicare deductible and/or coinsurance. Private insurance companies contracted with Medicare may bill Medicare differently.
If your health-care provider doesnt accept Medicare assignment, you may have to pay the full cost for the service up front, and get reimbursed by Medicare. You also might have to pay more than the Medicare-approved amount. In most cases, the doctors office should file the reimbursement claim for you. If you have to file your own claim, see below.
You May Like: How Is Part B Medicare Premium Determined
What Should I Do If My Provider Doesnt File My Claim
Before receiving care, ask your providers office whether they will submit your bill to Original Medicare. While they arent required to do so, some non-participating providers will still file your claims with Medicare.
The same situation applies for Medicare Advantage enrollees who see out-of-network providers. These providers dont have to file claims with your Advantage plan, but may choose to do so.
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself. You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the providers bill or invoice to your regional Medicare Administrative Contractor . Keep copies of everything you submit.
, Home Health Advance Beneficiary Notice, or Skilled Nursing Advance Beneficiary Notice if they believe Medicare will not cover your care. Providers normally will not bill Medicare after they issue an ABN.
You have the right to demand bill, which is when you demand that the provider or facility submit a claim to Medicare for your care. In order to demand bill, you must sign the ABN and agree to pay the charges if Medicare denies coverage. Demand billing can be used to generate a formal Medicare coverage denial, which gives you further appeal rights.)
If You Submit With A Private Health Insurer
To submit your Medicare Two-way claim with your private health insurer you need to follow these steps:
Your private health insurer will forward your claim to us. We’ll process your Medicare claim and if payable, well forward it to your private health insurer. Your private health insurer will pay you by cheque or EFT.
Under Medicare Two-way, private health insurers don’t collect each others forms.
Recommended Reading: When Can I Get My Medicare Card
Electronic Health Care Claims
How to Submit Claims: Claims may be electronically submitted to a Medicare Administrative Contractor from a provider using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by meeting CMS requirements contained in the provider enrollment & certification category area of this web site and the EDI Enrollment page in this section of the web site. Providers that bill institutional claims are also permitted to submit claims electronically via direct data entry screens.
HIPAA TR3s can be purchased at the official Washington Publishing Company website.
For more information please contact your local MAC or refer to the Medicare Claims Processing Manual , Chapter 24.
How To Resubmit A Denied Claim
Instructions Check the remittance voucher before submitting a second request for payment. Claims may be resubmitted for one of the following reasons only:
· The claim has not appeared on a remittance voucher as paid, denied, or suspended for thirty days after it was submitted or· The claim was denied due to incorrect or missing information or lack of a required attachment.
Do not resubmit a claim denied because of Medicaid program limitations or policy regulations. Computer edits ensure that it will be denied again.
No Response Received
If the claim does not appear on a remittance voucher within 30 days of the day it was mailed, the provider should take the following steps:
· Check recently received remittance voucher dates. Look for gaps. A remittance voucher may have been mailed but lost in transit. If the provider believes this is the case, call ACS Provider Inquiry.
· If there is not a gap in the dates of remittance vouchers received, please call the Medicaid fiscal agent, Provider Inquiry. An associate will research the claim.
· If the fiscal agent advises that the claim was never received, please resubmit another claim immediately. See the Resubmission Checklist on the following page in this chapter.
Correcting a Denied Claim
* Did you wait thirty days after the original submittal before resubmitting a missing claim?
* If using a photocopy of a claim, did you make sure it was legible and properly aligned?
Don’t Miss: Is Eliquis Covered Under Medicare
You Should Only Need To File A Claim In Very Rare Cases
Medicare claims must be filed no later than 12 months after the date when the services were provided. If a claim isn’t filed within this time limit, Medicare can’t pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the “Medicare Summary Notice” you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
What Additional Documentation Will I Need To Send With My Claim
Depending on the type of claim you are filing, the required documentation can vary. Generally, you will at least need the completed Patient Request for Medical Payment form and the itemized bill from your doctor or medical provider that shows the exact services provided.
Additionally, Medicare will most likely require a detailed letter that explains why you are submitting the claim personally. Reasons for filing your own claim that you may want to put into the letter include your provider not filing the claim in a timely manner, the provider or supplier does not participate in Medicare, or that they are just refusing to file the claim entirely.
You may also want to send any additional documents that you think will support your claim and that are relevant.
Also Check: How Much Does Medicare Part C And D Cost
If You Submit An Ancillary Claim At A Service Centre
Ancillary claims, including dental, optical and physiotherapy, don’t attract a Medicare benefit. However, as part of the Medicare Two-way program, you can follow these steps:
Your claim will be forwarded to your private health insurer for payment.
Medicare Reimbursement Rates And Allowable Charges
Medicare reimbursement rates or allowable charges are the amount of money that Medicare pays to doctors after they have filed a claim for services. Also known as the Medicare Physician Fee Schedule, the payments vary depending on which service is provided.
Medicare reimbursement rates will be based upon Current Procedural Terminology codes . These codes are numeric values assigned by the The Centers for Medicare and Medicaid Services for services and health equipment doctors and facilities use.
An example scenario would be when a doctor performs a diabetes test. After the treatment they may look up the CPT code for the procedure then file the necessary claim to Medicare. In return, Medicare would look up the allowable charge for that procedure and then reimburse the doctor the amount of money. Generally, doctors are reimbursed at a lower rate for Medicare services 80% of the total rate when compared to private health insurance.
Read Also: Is Coolief Covered By Medicare
Can Doctors Refuse Medicare
The short answer is “yes.” Thanks to the federal program’s low reimbursement rates, stringent rules, and grueling paperwork process, many doctors are refusing to accept Medicare’s payment for services.
Medicare typically pays doctors only 80% of what private health insurance pays. While a gap always existed, many physicians feel that Medicare reimbursements haven’t kept pace with inflation in the past several years, especially the rising costs of running a medical practice. At the same time, the rules and regulations keep getting more onerous, as do penalties for not complying with them.
Most American physicians participate in Medicare and “accept assignment” for their services without additional charges. However, if your doctor is non-participating or has opted out of Medicare, here are five options.
Medicare Claims And Reimbursement
In most cases, you wont have to worry about filing Medicare claims. Here are some situations where you might or might not need to get involved in the claim process.
- If you have Original Medicare, Part A and/or Part B, your doctor and supplier are required to file Medicare claims for covered services and supplies you receive. If your doctor or the supplier doesnt file a claim, you can call Medicare at 1-800-MEDICARE . TTY users can call 1-877-486-2048. Phone representatives are available 24 hours a day, seven days a week.
- The process is a bit different when it comes to Medicare insurance plans like Medicare Advantage plans. Under the Medicare Advantage program, providers typically dont file claims with Medicare, because Medicare pays these Medicare-approved insurance companies a fixed monthly amount. If you go outside of the plans network for services, however, you may have to file a claim with the health insurance plan, not with the Medicare program. If you have questions or concerns about claims, contact your Medicare Advantage insurance company.
Any Medicare claims must be submitted within a year of the date you received a service, such as a medical procedure. If a claim is not filed within this time limit, Medicare cannot pay its share.
Recommended Reading: Is A Sleep Study Covered By Medicare
