Who Can Get Medicaid
- No matter your state, you may qualify for Medicaid based on your income, household size, disability, family status, and other factors. But if your state has expanded Medicaid coverage, you can qualify based on your income alone.
- Enter your household size and state. We’ll tell you who is eligible for Medicaid, if your state expanded and if you qualify for Medicaid based only on your income.
- If you think you have Medicaid eligibility, you can create an account and fill out a Marketplace application. If it looks like anyone in your household qualifies for Medicaid or CHIP, we’ll send your information to your state agency. They’ll contact you about enrollment. You can apply any time of year.
- If you don’t qualify for Medicaid, we’ll tell you if you qualify for financial help to buy a Marketplace health plan instead.
Additional Payment For Administering The Vaccine In The Patients Home
View the infographic ) ) for COVID-19 vaccine administration in the home.
Effective June 8, 2021, Medicares additional payment amount for administering the COVID-19 vaccine in the home for certain Medicare patients is approximately $35 per dose. This payment also applies when you administer any of the additional or booster doses listed in the Medicare Payment Rates table.
Medicare will pay approximately $35 in addition to the standard administration amount , for a total payment of approximately $75 for a vaccine dose administered in a patients home. We also geographically adjust the additional amount and administration rate based on where you administer the vaccine.
We established this payment amount of approximately $35 on a preliminary basis to ensure access to COVID-19 vaccines during the PHE. We continue to evaluate the needs of Medicare patients and these policies, and well address them in the future, as needed.
Read Also: How Is Medicare Part B Financed
Disability Benefit Recipients Routinely Struggle With Medicaid Income Limits
It is fairly common for someone who is receiving disability benefits to struggle staying under the income limits for Medicaid eligibility. have incomes that are too high to qualify for Medicaid under current law. Also, with only a few limited exceptions, people who qualify for disability benefits do not become eligible for Medicare until two years after the date they are deemed eligible to receive benefits.
In too many instances, this means an individual who receives a health disability benefit check will be forced to go without health insurance during the two-year waiting period for Medicare coverage. As a result of this issue, some states offer buy-in programs to expedite your eligibility to access Medicaid coverage.
You May Like: How Do I Know If I Have Part D Medicare
How Do I Know If I Qualify For Medicaid And Medicare
Twelve million individuals are currently enrolled in both Medicaid and Medicare.1 These individuals are known as dual eligible beneficiaries because they qualify for both programs. As long as you meet the federal qualifications for Medicare eligibility and the state-specific qualifications for Medicaid eligibility, you will qualify as a dual eligible. To qualify for Medicare, individuals generally need to be 65 or older or have a qualifying disability.
There are several levels of assistance an individual can receive as a dual eligible beneficiary. The term full dual eligible refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as partial dual eligible.
*Cost sharing is the amount of your health care that you pay out of your own pocket. Typically, this includes deductibles, coinsurance, and copayments.
Can I Receive Medicaid And Social Security
It is possible for someone receiving Medicaid also to collect Social Security. However, each program has its own separate applications, separate requirements and will make its own eligibility decisions. In general, receiving SSI benefits will not affect your Medicaid eligibility.
However, SSD benefits, because they are typically higher payments, could affect your eligibility for Medicaid based on your individual states asset threshold. In other words, if you are receiving SSD benefits which put you over the minimum amount that your state permits for total assets, you might become ineligible for Medicaid. In some instances, Medicaid will require the individual to pay some of the monthly medical expenses out of the SSD money.
Don’t Miss: Is A Psa Test Covered By Medicare
Medicare/medicaid For Concurrent Benefit Recipients
Sometimes people approved for disability benefits receive both SSDI and SSI payments. In these cases, deciding whether theyll get Medicaid or Medicare coverage isnt so simple. When in doubt, you or your lawyer should contact the Social Security office in your area to determine eligibility.
Knowing how and if to apply for SSI or SSDI can be confusing. By hiring a benefits attorney at the Disability Help Center, youll have someone on your side to make things easier. Let us help you gather the needed documentation, work with medical professionals, and track the status of your application or appeal. It all starts with a free consultation, so call us today at 1-888-418-8860.
How Do You Qualify For Dual Eligibility
To be dual eligible means to be eligible for Medicare Part A and/or Part B along with full Medicaid benefits and/or assistance. Being dual eligible and enrolling in Medicare and Medicaid means you typically get assistance with Medicare costs such as premiums, coinsurance and deductibles through a Medicare Savings Program .
You May Like: Does Medicare Cover Genetic Cancer Screening
Impact Of The Affordable Care Act For Disability Benefit Recipients
The Medicaid program was expanded greatly under the landmark Affordable Care Act . For example, the ACA encouraged states to increase the income cutoff for Medicaid eligibility to 133 percent of the Federal Poverty Level. In 2021, the eligibility threshold is set at $17,130 in annual income for an individual.
In addition to encouraging states to expand eligibility for Medicaid, the ACA also overhauled the way states calculate income and assets for Medicaid eligibility in ways that allowed more low-income disability benefit recipients to qualify for supplemental security income during the two-year waiting period. However, it is important to note that multiple states opted not to participate in the expansion of Medicaid, so you need to check the relevant rules and regulations in effect in the state you reside.
Have Questions About the Impact of Disability Benefits on Your Eligibility for Medicare or Medicaid? Get Answers by Completing a Free Evaluation Form
If you are interested in applying for disability benefits, or are currently in the process of applying for benefits, you may have important legal questions that need to be answered by an experienced professional. This is why you should complete the free evaluation form on this page so you can be connected to an experienced and knowledgeable disability benefits lawyer in your area.
What Is Covered By Medicaid
Mandatory benefits include services including inpatient and outpatient hospital services, physician services, laboratory and x-ray services, and home health services, among others. Optional benefits include services including prescription drugs, case management, physical therapy, and occupational therapy.
Also Check: How Often Will Medicare Pay For A Walker
Can One Have Dual Eligibility For Both Medicare And Medicaid
Yes, Medicare and Medicaid are not mutually exclusive programs. Persons who are eligible for both are referred to as having Dual Eligibility, Dual Eligibles, or often simply Duals. Medicare is the first payer of covered benefits, while Medicaid is the secondary payer.
Typically, Medicaid will pay for Medicare premiums and co-payments for dual eligibles. In fact, many states have special programs intended to make it easier for seniors to manage their dual eligibility status, as it can be confusing to know where to turn for what services. This is generally in the form of managed care.
There are also programs called Medicare Saving Programs for low-income seniors that dont quite qualify for Medicaid.
We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Does Medicaid Pay What Medicare Doesn T
Both Medicare Part A and Part B copays and coinsurance. The Medicare Part D premium, deductibles and copays for prescription drugs. In some states, Medicaid will cover benefits that Medicare does not, such as dental care, transportation to and from doctor visits, eyeglasses, physical therapy and other services.
Also Check: Will Medicare Pay For Handicap Bathroom
You May Like: How To Enroll In Medicare Part B Online
How To Choose The Right Health Care Coverage For You
Although you may be eligible for both programs, in some cases, you might be in a position to choose between Medicare and Medicaid.
If youre eligible for Medicare, you have to choose between Original Medicare or Medicare Advantage, based on your preferences. But how do you decide? Take a look at some of the key differences.
If You Get Ssdi Benefits And Are In A 24
- You may be able to get Medicaid coverage while you wait. You can apply 2 ways:
- Create an account or log in to complete an application. Answer yes when asked if you have a disability. Well forward your application to your state Medicaid agency.
- Apply directly to your state Medicaid agency. Select your state from the menu on this Medicaid page for contact information.
When asked about your income on your Marketplace application, be sure to include your SSDI income.
Also Check: What Is Earliest Age For Medicare
Qualifying Medicaid Beneficiary Plus
The QMB Plus category is for people with incomes lower than QMB levels. It provides full Medicaid benefits, including free or nearly-free medical services and nursing home care.
In 2020, the maximum monthly income is $1,094 for an individual and $1,472 for a couple. For 2021, the maximum asset level is $7,970 for an individual and $11,960 for a couple.
The Solution: Medicaid Could Make Up The Medicare Difference For You
Some people think that Medicaid is welfare, but that is not true. Medicaid covers medical expenses, long-term care services, case management, and much more. Medicaid is a different program than Medicare.
Medicaid is for people whose incomes are close to the federal poverty line. Today, Medicaid provides extra help paying doctor bills, hospital bills, and prescriptions for millions of Americans aged 65 and over. If you fall into this category, then youll want to take a close look at your Medicaid eligibility.
Not Limited to Seniors
Others besides seniors can receive Medicaid benefits In all states, Medicaid provides health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities. In some states the program covers all low-income adults below a certain income level. People with a disability or certain medical conditions may qualify for Medicaid at any age.
Read Also: Why Is My First Medicare Bill So High
Understanding What The Two Programs Are
Category: Educational, Medicare Healthcare
Just when you think that Medicare itself cannot get any more confusing, it does. But, for some Americans, it becomes more confusing in a positive way. For many Americans who are close to retirement and qualify for Medicaid health assistance, the question about whether they will also qualify for Medicare health insurance is one theyre likely to consider, especially if they dont have the answer. And if its still a question you have, you can rest easy knowing that it will be answered by the end of this article.
This article is intended to answer your question about whether you qualify for both Medicare and Medicaid, what each is, how you can qualify for the two services and what their overall differences are.
Lets get into it by first understanding what the two programs are.
Medicare Advantage And Medicaid Whats The Difference
The Medicare Advantage program is considered a âpartâ of Medicare â Medicare Part C. If you qualify for both Medicare and Medicaid, you can generally sign up for a Medicare Advantage plan. Or, you might want to look into the Medicare Savings Programs described above.
Many people prefer Medicare Advantage plans as a way to get their Medicare coverage. Medicare Advantage is a program that lets you get your Medicare Part A and Part B benefits through a private, Medicare-approved insurance company. Many plans have extra benefits, too, like prescription drug coverage and routine dental care.
Also Check: Does Medicare Cover Home Health Care After Surgery
Medicaid And Medicare Can You Get Both
If you qualify for both Medicare and Medicaid, thatâs called being dual eligible. So besides your Medicare Part A and Part B coverage, Medicaid may also cover additional services. Specific benefits can vary by state, but may include medical transportation, vision, chiropractic and dental care, and nursing facility care beyond the 100-day limit that Medicare covers.
There are four Medicare Savings Programs available, with each providing a different level of financial assistance:
- The Qualified Medicare Beneficiary Program helps pay Medicare Part A and part B premiums, deductibles, copayments, and coinsurance.
- The Specified Low-Income Medicare Beneficiary Program helps pay Medicare Part B premiums.
- The Qualifying Individual Program helps pay Medicare Part B premiums.
- The Qualifying Disabled and Working Individuals Programpays Medicare Part A premiums for certain people who have disabilities but are still working.
Dual-eligible beneficiaries who are eligible for the Qualifying Individual, Specified Low-Income Medicare Beneficiary, or Qualifying Medicare Beneficiary Programs will automatically be eligible to get Extra Help , which helps with Medicare prescription drug costs.
Each Medicare Savings Program has different eligibility requirements, which may change from year to year. Check with your stateâs Medicaid program to see if you qualify.
Qualifying Medicaid Beneficiary Only
This is for people who are not eligible to receive full Medicaid benefits. Medicaid will pay the recipients Medicare Part A premiums . It will also pay their Medicare Part B premium for them. Besides, there may be extra help with Medicare insurance deductibles and copayments.
If youre a QMB recipient, you chose the Medicare insurance that you like. Then, Medicaid helps with your deductibles and copayments.
You will want to have good Medicare insurance, like a Medicare Advantage plan, in place if you receive Medicaid benefits. Remember, QMB is a dual-eligible program, not a Medicaid-only program.
Maximum monthly income for those aged 65 and over to qualify for QMB in 2021 is $1,094 for an individual and $1,472 for a couple. For 2021, the maximum asset level is $7,970 for an individual and $11,960 for a couple.
In certain situations like nursing home benefits, people with greater assets may be asked to spend down their assets first before Medicaid kicks in with help.
You May Like: What Is Difference Between Medicare Advantage And Supplement
Close To Dual Eligibility Check With Your States Medicaid Office
As part of the Affordable Care Act, each state was allowed to broaden its Medicaid assistance levels. Some states agreed to expand coverage but others did not. So dont automatically rule yourself out discuss your circumstances with your local social services provider.
The Medicare-Medicaid Coordination Office: Medicaid can be quite confusing. Complexity keeps some people from even applying for Medicaid, even though the application process is quite simple.
To help solve that problem, the federal government runs a Medicare-Medicaid Coordination Office. The office streamlines the experience of getting healthcare to those who need it. They work to develop insurance policies designed to work especially with dual-eligible citizens.
Personal Support Is Part Of A Dual Plan
With many MSHO plans, youll choose a primary care physician to manage your care. Your doctor can also refer you to a specialist or get health plan approval for certain care, if needed.
The plan will have a network of doctors, clinics and hospitals. Check the provider list to make sure you get your care in-network. You may have to pay for services you get out of the network . For home and community-based services, MSHO plans use every provider that is enrolled with the State.
Youll also have a Care Coordinator to guide your health care. This person is usually a registered nurse or a licensed social worker. Heres the type of personal support a care coordinator provides when youre enrolled in an MSHO plan:
- Explains how your plan works
- Partners with you to understand your key health goals and collaborates with you to create a person-centered care plan then gives you support and tools to reach those goals
- Helps you refill prescriptions as needed
- Helps you navigate Medicare and Medicaid services you may qualify for, like home health care, a personal care assistant, homemaker and companion services, delivered meals, or home safety equipment
Don’t Miss: Does Medicare Cover Laser Surgery
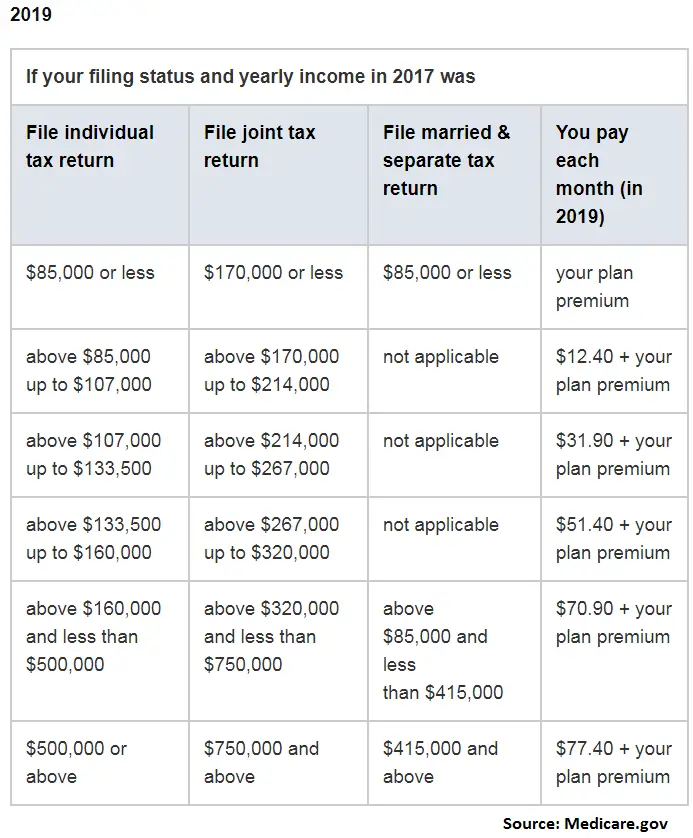
Help Paying For Medicare Premiums
Medicare Savings Programs are programs run by state governments. They may payfor Medicare Part A and/or Part B premiums, deductibles, copayments and coinsurance associated with Medicare for people with limited income and assets.
To learn more about the costs of Medicare, read the most frequently misunderstood Medicare terms.
Income is the amount of money you earn during the year.
Assets are any money you have in the bank, and the value of certain investments . However, the house you live in and up to one car you own are not counted as assets when it comes to qualifying for a Medicare Savings Program.
Medicaid And Medicare Are Both Available To Me What Is The Reimbursement Process
When dual-eligible Medicare and Medicaid beneficiaries have medical costs, Medicare becomes the primary payer and pays first, with Medicaid paying second, always paying last. However, there are certain things that Medicare doesnt cover, such as long-term care. If a beneficiary has a skilled need for long-term care services, which Medicaid primarily covers, Medicare will remain the primary health insurance carrier for services rendered in the long-term-care facility, such as nursing care and physical therapy.
In rare cases, if a dual-eligible Medicare and Medicaid beneficiary has supplementary benefits , Medicare is the largest payer, Medigap becomes the next payer, and Medicaid, which always pays last, will be the tertiary payer.
Also Check: How To Become A Licensed Medicare Agent
