Find A $0 Premium Medicare Advantage Plan Today
1 Badger, Cary. The Rise of Over-the-Counter Programs in Medicare Advantage Plans. . HealthScape. Retrieved from https://healthscape.com/insights/the-rise-of-over-the-counter-otc-benefits-in-medicare-advantage.
MedicareAdvantage.com is a website owned and operated by TZ Insurance Solutions LLC. TZ Insurance Solutions LLC and TruBridge, Inc. represent Medicare Advantage Organizations and Prescription Drug Plans having Medicare contracts enrollment in any plan depends upon contract renewal.
Plan availability varies by region and state. For a complete list of available plans, please contact 1-800-MEDICARE , 24 hours a day/7 days a week or consult www.medicare.gov.
Medicare has neither reviewed nor endorsed this information.
How Much Do Hormone Medications Cost
The cost of hormone pellets may range from $300 to $350 for women and $650 to $750 for men. The cost may depend on the number of doses as well as the type of hormone needed.
Note: Medicare coverage changes all the time. And your specific coverage may vary from plan to plan for Medicare Advantage and Medigap plans. Always be sure to double check with your health care provider and/or Medicare insurance provider about what your plan covers and what it does not.
Will Medicare Cover Anemia Treatment
Part A covers therapy during a hospital stay. Coverage may include services such as blood transfusions, medications, injections, and surgeries. Part B covers doctor visits and specific treatments.
Also, outpatient drugs fall under Part B. Further, Part B may pay for B-12 or iron injections that you obtain from your doctor. With Medicare, deductibles and coinsurances apply. Medigap can help cover these costs.
Also Check: Does Medicare Cover Dupuytren’s Contracture
Does Medicare Cover Anemia
Home / FAQs / Medicare Coverage / Does Medicare Cover Anemia
Medicare covers anemia, but the costs depend on treatment, and if you have supplemental coverage. Below were going to discuss everything you need to know about how Medicare covers anemia. When you finish this article, youll be an expert!
Does Medicare Cover Medical Nutrition Therapy
If you have kidney disease or diabetes, you might be entitled to free nutrition therapy services under Medicare Part B, which includes:
- Initial lifestyle and nutrition assessment
- Group or individual therapy
- Assistance managing certain lifestyle factors, potentially including vitamin supplementation
- Follow-up visits
Read Also: What Does Original Medicare Mean
Does Medicare Cover Rheumatoid Arthritis
In general, Medicare covers the necessary treatments. But the way its covered will depend on the type of care you receive. Part A covers services, procedures, and drugs you receive as an inpatient at a hospital.
For Rheumatoid Arthritis patients, this might include joint replacement surgery or treatment for other medical conditions that develop. Part B covers infusions, outpatient surgeries, physical therapy, and other treatments for Rheumatoid Arthritis. But, youll pay a portion of the cost. If your arthritis is severe, Part B could cover a lift chair due to medical necessity.
Part D covers the prescriptions you take at home, including prescription injections. If you have Medicare Advantage, your coverage will be at least as good as Medicare. But your copays and other costs may be different. Many Medicare Advantage plans have prescription coverage built-in.
Also, those with chronic health issues may be eligible for Chronic Care Management that would increase the quality of life.
Are Punctal Plugs Safe
Its rare, but the irritation could be so severe, your doctor will decide to remove them. Sometimes they can be flushed out, but if that doesnt work, you may need surgery. The risks include scarring and damage to the tear duct. In severe cases, your doctor may have to replace the duct with an artificial one.
Recommended Reading: Does Medicare Coverage Work Overseas
Does Medicare Cover Vitamin D Testing
Routine tests are a fundamental part of preventive care and health management. However, additional screenings and lab work may be ordered by your physician if deemed medically necessary. Different medical conditions and some lifestyle factors can contribute to low vitamin D levels in the body. Medicare insurance may cover additional tests to determine or monitor deficiency for some situations.
Benefits of Vitamin D
The primary function of vitamin D in the body is to contribute to bone strength and density. Because vitamin D helps your body absorb calcium, you need it to prevent your bones from becoming fragile or softening.
Reports from the Mayo Clinic note that vitamin D may also play a role in improving cognitive health, preventing certain cancers, and treating plague-type psoriasis in a topical preparation. Some studies also suggest that maintaining appropriate vitamin D levels can have a positive impact on mental health.
Most people gain enough vitamin D from exposure to the sun or from fortified foods. In cases where you have limited sun exposure or you may have other underlying health conditions that decrease your natural vitamin D levels, you may need to supplement.
Potential Risk Factors for Vitamin D Deficiency
If you experience medical conditions that prevent your body from processing vitamin D through sun exposure or diet, vitamin D deficiency can pose a major health risk. These conditions can include:
- Crohns disease
- Tuberculosis
- Histoplasmosis
Related articles:
Low Income Subsidy Questions
No. The “extra help” is a subsidy that people with Medicare and Medicaid automatically qualify for without having to complete an application.
If you do not have Medicaid, but Medicaid pays your Medicare Part B premium, you automatically qualify for “extra help” and you don’t need to apply.
You may still be eligible for “extra help” to pay for the Medicare prescription drug plan premiums. To apply for extra help, you should visit or call your local Social Security Administration office or apply on line at
Recommended Reading: How Much Do Medicare Plans Cost
Does Medicare Cover Over
Recently, we wrote about whats missing from Original Medicare. One key thing is prescription drug coverage, which can be purchased through a Medicare Part D plan or by enrolling in a Medicare Advantage plan with Part D coverage . But we also know some of the medications and health-related items you need may not require a prescription.
Theres good news! Over the last few years, the Centers for Medicare & Medicaid Services has given MA plans the flexibility to offer supplemental benefits such as over-the-counter medication allowances. This allows you to purchase select, eligible health and wellness items like allergy pills, cold and flu products, first aid supplies, vitamins and more.
This is important because Original Medicare and Medicare Part D do not pay for OTC drugs. This includes:
- Medications used for hair growth or other cosmetic reason
- Medications used to treat cold or cough symptoms
- Medications used to treat sexual dysfunction
- Vitamins and minerals
- Weight gain or weight loss medications
According to the Consumer Healthcare Products Association , the average person in the U.S. makes 26 trips each year to purchase OTC products. We assume this number increases as you age, so every penny counts. An OTC allowance gives you an allotted amount usually per month or per quarter not to be exceeded. MA plans offering an OTC allowance usually have a catalog with approved products to choose from.
Prescription Drugs You Take At Home
PartB medical insurance covers only drugs that cannot be self-administered and thatyou receive as an outpatient at a hospital, a clinic, or at the doctor’soffice.
MedicarePart A covers drugs administered while you are in the hospital or in a skillednursing facility, and coverage for all other prescription drugs falls underMedicare Part D, which you must enroll in and pay for separately from Parts Aand B.
Read Also: How Much Is The Cost Of Medicare Part B
How Is Anemia Diagnosed
When making a diagnosis, a doctor may look at a persons medical history, do a physical exam, and order a complete blood count test to detect anemia. The doctor may also use a CBC test to evaluate a persons overall health.
The recommended treatment will depend on the type of anemia. Recommendations may include:
- an iron supplement
- a certain type of vitamin
- intravenous iron therapy
- prescription medicine to help the body produce more red blood cells
- for severe cases, red blood cell transfusions
The doctor may also suggest a change in diet to prevent future health problems.
Does Medicaid Pay For Blood Tests

If you qualify for both Medicare and MedicaidMedicaid is a public health insurance program that provides health care coverage to low-income families and individuals in the United States…., in most cases Medicaid will cover nearly all of your costs for blood work. Visit www.medicare.gov to learn more about how to qualify.
Also Check: Does Medicare Cover Dexcom G6 Cgm
Medicare Part A Costs
In-hospital blood work ordered by your doctor is generally fully covered under Medicare Part A. However, you still need to meet your deductible.
In 2021, the Part A deductible is $1,484 for most beneficiaries during the benefit period. The benefit period lasts from the day you enter the hospital through the next 60 days. It is possible to have multiple benefit periods in a year.
Does Medicare Cover Enbrel
Enbrel is a biologic DMARD that belongs to a class of drugs known as TNF inhibitors.
If your doctor prescribes Enbrel, youll inject yourself weekly. Because you take Enbrel at home, it falls under Part D. According to Enbrels website, the medications list price is $1,389 per week for a 50 mg dose.
Although Enbrel offers a copay card to help reduce costs. It claims that 76% end up costing less than $50 a month, while the other 24% cost $469 a month. The amount you pay depends on the specifics of your prescription plan. If you have a limited income, you may qualify for extra help with prescription costs.
You May Like: Does Medicare Cover Cosmetic Surgery
What Anemia Treatments Does Medicare Cover
Your treatment for anemia will depend on the kind of anemia you have. In mild cases, you might be able to treat your anemia with dietary changes.
Your doctor might recommend you eat more foods that can help your body get the iron, vitamin B12, or folic acid it needs. In other cases, you might need more complex treatment.
Some treatments covered by Medicare include:
Other treatments will depend on your anemia.
For example, if your anemia is caused by a heart condition, youll need treatments that help your heart. If your anemia is caused by your bone marrow, you might need a bone marrow transplant.
Medicare will cover those treatments as long as theyre medically necessary.
Your anemia treatment might include several parts of Medicare. Its a good idea to know what parts you have and what each part will cover for your anemia diagnosis.
Heres a breakdown of the Medicare parts:
Tips for choosing a Medicare plan if you have anemia
- Make sure you have prescription drug coverage.
- Compare the costs of Part D and Advantage plans in your area.
- Check the formulary of Part D and Advantage plans to make sure the supplements you need are included.
- Consider a Medigap plan if you think you might need blood transfusions.
Why Should Seniors Take Vitamin Supplements
There are several reasons why older adults should take vitamins.
- An older body is less efficient at absorbing key nutrients from food.
- Certain healthy vitamin-rich foods can become difficult to chew or digest as we age.
- Our bones become more brittle as we age, and certain vitamin supplements can also give us a much-needed calcium boost.
- Older adults may not get as much sunlight exposure as they once did, which causes Vitamin D levels to wane.
- Medications, especially diuretics, can flush out nutrients before they can be properly absorbed by the body or block them from being absorbed at all.
- Age-related diseases and conditions can suppress the bodys ability to absorb nutrients, and some may even require a special diet that is low on certain vitamins and nutrients.
- Older adults may not cook as often as they once did, and ready-to-eat meals can rob you of essential vitamins and nutrients.
You May Like: Does Medicare Cover Cancer Treatment Centers Of America
Supplementing Part B Medical Insurance
Whenyou look at the list of what Medicare medical insurance does not cover, it’seasy to understand why people with Medicare still wind up personallyresponsible for an average of half of their medical bills.
Part BMedicare medical insurance is intended to pay for only a portion of doctorbills, outpatient hospital and clinic charges, laboratory work, some homehealth care, physical and speech therapy, and a very few drugs and medicalsupplies.
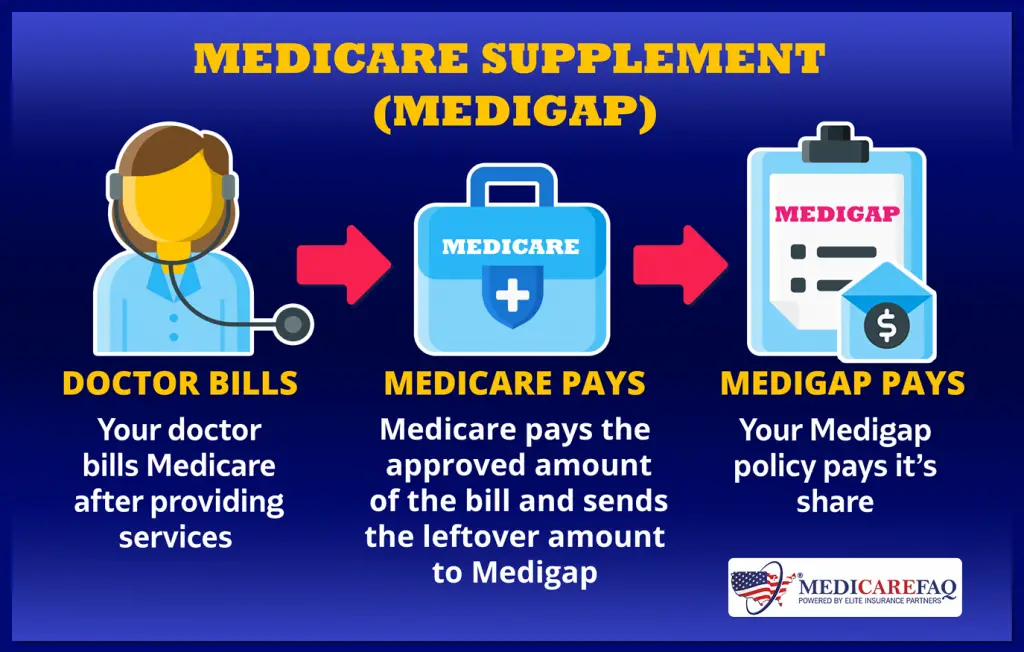
PrivateMedicare supplement insurancecalled medigap insurancemay help you make up thedifference. Alternatively, many people fill in the gaps in Medicare by joininga Medicare Advantage health plan . A Medicare Advantageplan often comes in the form of a managed care plan and combines basicMedicare-level coverage with supplemental benefits. If you cannot affordprivate supplement insurance, you may be eligible for Medicaida public programfor people with low income and few assets.
Formore information, see our articles on medigap insurance, Medicaid, and MedicareAdvantage plans.
How Much Do Blood Tests Cost
Costs of blood tests and other lab screening or diagnostic tests can vary. The costs are based on the particular test, your location, and the lab used. Tests can run from a few dollars to thousands of dollars. Thats why its important to check that your test is covered before you have it done.
Here are some of the blood test costs you can expect with the different parts of Medicare.
Read Also: What Is A Ppo Medicare Plan
Does Medicare Cover Orencia Infusions
Orencia is also a biologic DMARD its available as an infusion or an injection. If you have an infusion, your doctor will administer the drug through a vein in your arm.
Because you obtain infusions outside the home, Part B covers them. If you have a Medigap plan, it will pay the coinsurance costs.
The sticker price for one Orencia infusion is $3,527, but the manufacturer says Medicare patients pay from $0 to $705. If you have Medicare Advantage, your cost will depend on your plan.
If you take Orencia injections at home, the medication falls under Part D. Your benefits will depend on the kind of plan you have. You could pay as much as $1,500 a month. But, Orencias website says more than 80% of Medicare patients pay $25 or less per month.
Most People Don’t Need Vitamin D Testing

ROCHESTER — Nearly nine out of 10 upstate New Yorkers have no medical reason to have their vitamin D levels tested, yet health care providers and patients continue to frequently request the test, according to an analysis released today by Excellus BlueCross BlueShield.
Last year, 641,000 upstate New Yorkers had their vitamin D levels tested, and about 42 percent did so without a medical indication for it. Typically, only people with certain conditions, including but not limited to osteoporosis, kidney and liver disease, malabsorption syndromes, bone disorders and certain endocrine conditions, are candidates for testing. Older adults and some pregnant or lactating women also can expect to have their doctors recommend vitamin D testing.
Even with a medical indication to test for vitamin D deficiency, its valid to question the need for the test, because the outcome wont necessarily change the treatment, said Matthew Bartels, M.D., Excellus BCBS medical director for health care improvement. If your doctor suspects a low vitamin D level, taking an over-the-counter supplement or getting more vitamin D from your diet may be sufficient.
Vitamin D is an essential vitamin in how our bodies function. It helps our bodies absorb calcium, which keeps our bones and muscles including the heart healthy and strong. Most people get enough vitamin D through the foods they eat and the time they spend in the sun, said Bartels.
Read Also: Why Is My Medicare So Expensive
Medicare Home Infusion Therapy Coverage Act
The Preserving Patient Access to Home Infusion Act is new legislation that gives patients access to Part B home infusion medications. The main goal of the Act is to ensure patients with Medicare access under the Part B Durable Medical Equipment benefit. The recent outbreak puts emphasis on the value of home-based treatments for vulnerable patients.
What Does Medicare Supplement Insurance Pay For
Medicare Supplement insurance typically helps pay for Medicare Part A and Part B coinsurance and copayments. It also may help pay Original Medicare deductibles and certain other out-of-pocket costs.
Medicare Supplement insurance only works alongside Original Medicare, Part A and Part B. As the name implies, its a supplement it adds to your Original Medicare coverage by helping pay certain Medicare-approved costs.
Don’t Miss: Does Medicare Cover Bed Rails
Do Medicare Advantage Plans Pay For Otc Drugs
In 2019, more than 51 percent of Medicare Advantage beneficiaries were enrolled in a plan with OTC benefits.1
This is due in part to the Centers for Medicare and Medicaid Services giving Medicare Advantage plan carriers more flexibility in the benefits that Medicare Advantage plans can offer.
This move was designed to:
- Improve preventive care
- Reduce health care complications
- Help keep health costs lower
This opened the door for Medicare Advantage plans to begin including coverage for things such as over-the-counter medication allowances as part of their benefit lineup.
Some of the other newly expanded Medicare Advantage benefits include things like:
- Non-emergency transportation services
- Caregiver support
- Home remodeling for aging in place
- Some home-based palliative care
- Home meal delivery
Medicare Advantage plans may sometimes partner with a national retail pharmacy like Walmart or CVS where plan members may utilize their OTC benefit. Some Medicare Advantage plans may also offer home delivery of over-the-counter drugs.
The exact OTC allowances and other benefits of Medicare Advantage plans may vary. Some Medicare Advantage plans feature $0 premiums, though these types of plans may not be available where you live.
