What Are My Costs With Dual Eligibility
Dual eligibility can limit individual costs for beneficiaries. For those with Medicare, state Medicaid programs will pay for many cost-sharing and out-of-pocket expenses for medical services. For any service you receive, Medicare pays first and covers all eligible costs. Any qualified costs not covered by Medicare will be covered by Medicaid.
What extra benefits and savings do you qualify for?
How Do I Know If I Should Be Dual Eligible
Beneficiaries can find out if theyre eligible for Medicaid by contacting their Medicaid office. An Internet search for Medicaid offices in a beneficiarys state should provide the number to call but beneficiaries should make sure they are contacting a government office before sharing any personal information.
The Centers for Medicare and Medicaid Services also maintains a list of state agencies that oversee Medicaid. Beneficiaries can see if they already have Medicaid by contacting 1-800-MEDICARE and asking whether they receive Extra Help with their prescription drug costs .
What To Consider When Enrolling In A D
You have the option to choose the plan for your D-SNP and BHSO coverage if you live in a county that offers aligned enrollment.
Aligned enrollment helps dual-eligible clients manage their physical and behavioral health services under one plan. This makes it easier to find a provider and coordinate your Medicare and Apple Health services.
View the aligned enrollment map in our service area guide to see if alignment is available in your county.
Each plan may recommend different steps to enroll. Visit their webpages for more information.
You May Like: Does Medicare Pay For Medical Alert Bracelets
What Are The State
Benefits for dual eligible beneficiaries candiffer based on your state of residence. Differences by state may include:
- Medicaid offered through Medicaid managed care plans
- fee-for-service Medicaid coverage
- plans that include all Medicare and Medicaid benefits
Income and resource standards are defined by federal law for full Medicaid and the Medicare Savings Programs. At their discretion, states can effectively raise the federally mandated limits.
Youre also considered a dual eligible beneficiary if youre enrolled in Medicare Part A or Part B and receiving cost-sharing through a Medicare savings program .
Below is table summarizing the benefits and eligibility criteria for each of the different MSPs in 2021:
| MSP | ||
|---|---|---|
| Specified Low-Income Medicare Beneficiary program | assists in the payment of Part B premiums | individual monthly income of $1,308 or less, individual resources limit of $7,970 married couple monthly income of $1,762 or less, married couple resources limit of $11,960 |
In addition to the Medicare savings programs, you also may be eligible for some of the following needs-based programs through Medicare:
- PACE : a Medicare-Medicaid joint program that provides medical and social services for people with significant needs who want to continue living at home
- Medicares Extra Help program: can help those with low incomes get the prescription drugs they need at reduced or no cost
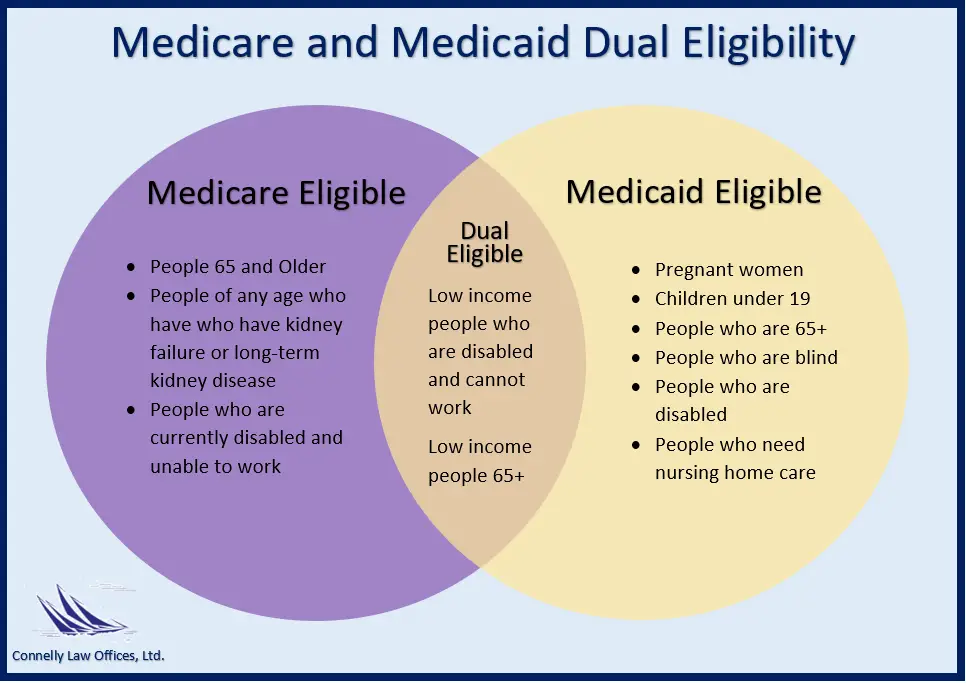
Dual eligibility for Medicare and Medicaid means that youre enrolled in Medicare and either:
Can You Have Both Medicare And Medicaid
- Beneficiaries who are eligible for both Medicare and Medicaid are considered dual eligible. Learn how to enroll and the benefits you can expect if you qualify for dual eligibility.
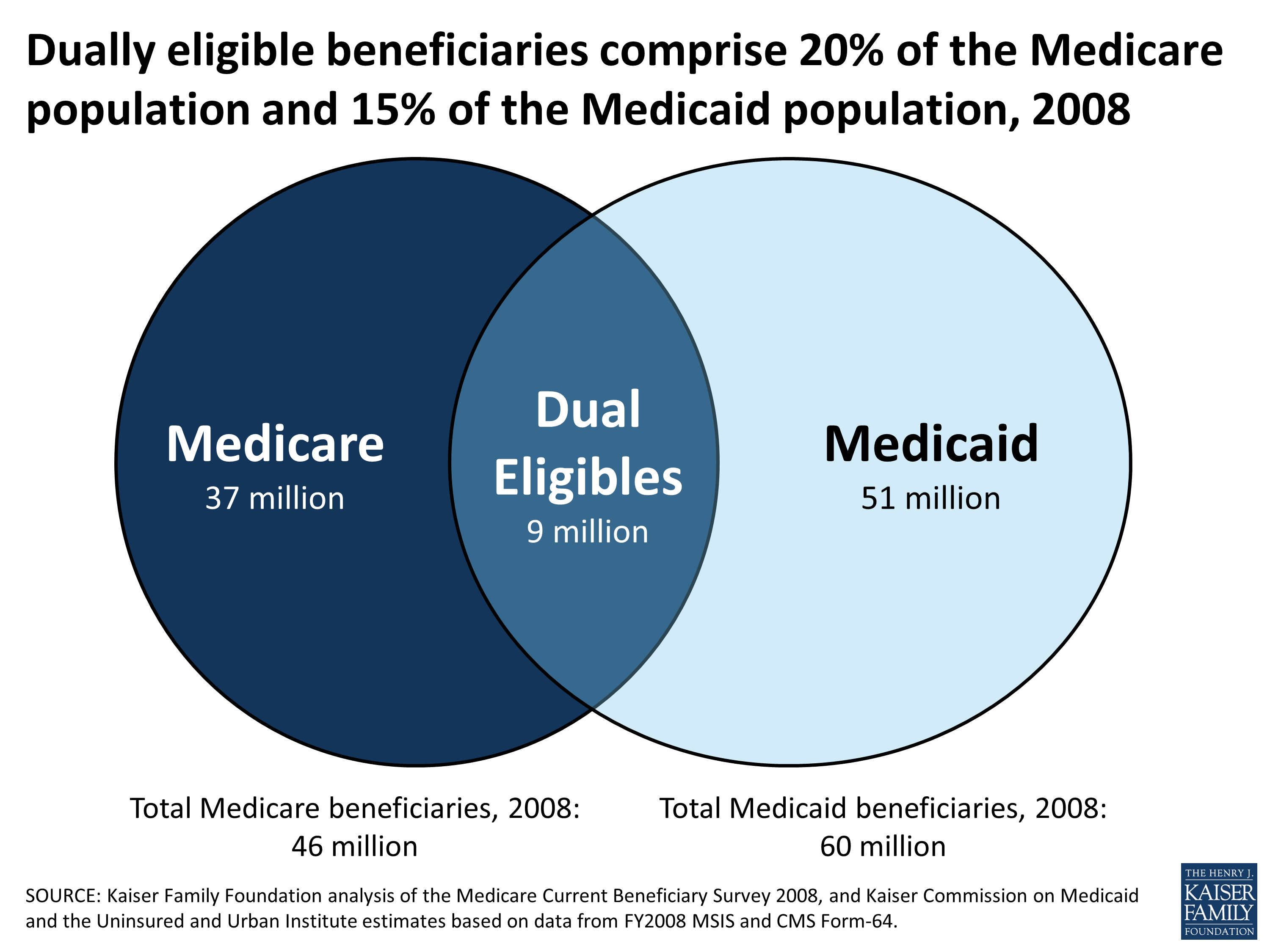
More than 62 million Americans are enrolled in Medicare in 2020, and nearly 69 million people are enrolled in Medicaid.
As of 2019, well over 12 million Americans are dual eligible for both Medicare and Medicaid. You may wonder how someone can have both Medicare and Medicaid, and you may wonder if you qualify for dual eligibility.
Below well discuss the eligibility qualifications for Medicare and Medicaid, the benefits available to you if youre dual eligible and other information you may want to know about dual eligibility.
Read Also: Are Lidocaine Patches Covered By Medicare
Medicare Part D Extra Assistance Program
Aside from Medicaid, many other programs assist with medical expenses, and government sponsors them. Extra Help, a program that assists Medicare Part D enrollees with their prescription drug costs, can be applied for by a qualified individual.
To be eligible for Extra Help, a persons combined investments, real estate property, and savings must total no more than $29,160 if they are married and live with their spouse, or $14,610 if they are single.
To learn more about Extra Help and how to apply for it, go to the Medicare website.
How To Qualify For Both Medicare And Medicaid
The government-funded healthcare programs Medicare and Medicaid are two distinct programs however, a person may be eligible for both at the same time.
Medicare and Medicaid are both government-sponsored programs that are intended to assist people in meeting their healthcare expenses. A person who qualifies for both programs is called dual eligible by the federal government.
According to Medicaid.gov, approximately 12 million people in the United States are considered to be dual-eligible for Medicare and Medicaid benefits.
In this post, well go through Medicare and Medicaid eligibility, as well as what you should know about each program.
Read Also: How Much Will Medicare Pay For Mental Health Services
Having Dual Eligibility For Medicaid & Medicare: Who Is Eligible And Benefits
SummaryMedicaid is a health insurance program run by each individual state for people who are low-income, and Medicare is a national health insurance program for all Americans over 65. People who are eligible for both Medicaid and Medicare are considered dual eligibles. While some benefits are available through both programs, there are also differences in coverage that make dual eligibility a good way for many seniors to pay for their care needs. Only Medicaid, for example, pays for long-term nursing home care.
Who Can Apply For Dual Eligibility
To qualify for dual eligibility, you need to meet the enrollment criteria for both the Medicare and Medicaid program.
To get Medicare coverage, you will need to be either:
-
65, or turning 65 in the next three months.
-
Disabled.
-
Suffer from ESRD .
To get Medicaid coverage, you will need to:
-
Be a citizen or lawful permanent resident of the U.S.
-
Be a resident of the state in which you are receiving Medicaid coverage.
-
Pass a state-specific income and asset eligibility test to determine if you qualify.
Specific individuals are exempt from the income eligibility requirement. You can learn more about this by visiting the Medicaid.gov website.
If you meet both the Medicare and Medicaid enrollment criteria you will become dual eligible, and Medicaid will assist in covering the cost of your Medicare coverage.
Income and asset requirements are different for each state. Here are three examples to show you what these are in 2022 for different parts of the U.S.
Read Also: Does Medicare Cover Ct Scans
Can You Have Medicare And Medicaid
The short answer is yes. If you receive coverage from both Medicaid and Medicare, youre a dually eligible beneficiary. If you are dual eligible, you may be enrolled in Medicare and then qualify for Medicaid, or enroll first in Medicaid but later qualify for Medicare. Medicaid assists seniors with limited income and people with disabilities also enrolled in Medicare.
How does dual eligibility work?
Dual-eligible beneficiaries can have:
- Medicare Part AMedicare Part A, also called “hospital insurance,” covers the care you receive while admitted to the hospital, skilled nursing facility or other inpatient services. Medicare Part A is part of Original Medicare.
- Medicare Part BMedicare Part B is the portion of Medicare that covers your medical expenses. Sometimes called “medical insurance,” Part B helps pay for the Medicare-approved services you receive.
- Both Part A and Part B
- Full Medicaid benefits
- State Medicare Savings Programs
Medicare benefits always pay first, and Medicaid benefits assist with costs not fully covered by Medicare.
Medicaid will pay premiums and out-of-pocket expenses for dual-eligible Medicare beneficiaries. Medicare and Medicaid work together to cover costs, including long-term services. If you do not have full Medicaid benefits, Medicare Savings Programs may help cover some of those costs:
Are you eligible for cost-saving Medicare subsidies?
Unitedhealthcare Connected General Benefit Disclaimer
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the Member Handbook. Limitations, copays and restrictions may apply. For more information, call UnitedHealthcare Connected® Member Services or read the UnitedHealthcare Connected® Member Handbook. Benefits, List of Covered Drugs, pharmacy and provider networks and/or copayments may change from time to time throughout the year and on January 1 of each year.
You can get this document for free in other formats, such as large print, braille, or audio. Call Member Services, 8 a.m. – 8 p.m., local time, Monday – Friday . The call is free.
You can call Member Services and ask us to make a note in our system that you would like materials in Spanish, large print, braille, or audio now and in the future.
Language Line is available for all in-network providers.
Puede obtener este documento de forma gratuita en otros formatos, como letra de imprenta grande, braille o audio. Llame al Servicios para los miembros, de 08:00 a. m. a 08:00 p. m., hora local, de lunes a viernes correo de voz disponible las 24 horas del día,/los 7 días de la semana). La llamada es gratuita.
Puede llamar a Servicios para Miembros y pedirnos que registremos en nuestro sistema que le gustaría recibir documentos en español, en letra de imprenta grande, braille o audio, ahora y en el futuro.
You May Like: How To Apply For Medicare Through Social Security
American Disabilities Act Notice
In accordance with the requirements of the federal Americans with Disabilities Act of 1990 and Section 504 of the Rehabilitation Act of 1973 , UnitedHealthcare Insurance Company provides full and equal access to covered services and does not discriminate against qualified individuals with disabilities on the basis of disability in its services, programs, or activities.
What If I Wish To Change My Bhso
If you enroll in a D-SNP, your BHSO plan will still cover your behavioral health care needs.
You may wish to change your BHSO plan to be the same plan as your D-SNP. You can also choose one plan as your D-SNP and another plan as your BHSO. It is up to you and your providers to choose which plans work best for your health care needs.
Visit our Apple Health managed care map and managed care matrix to see which BHSO plans are available in each region.
Contact Washington Apple Health if you wish to change your Apple Health BHSO plan.
You May Like: Does Medicare Cover Knee Injections
Health Services Not Covered By Medicare
Medicare isnt a one-size-fits-all solution. Original Medicare do not cover dental, hearing, or vision screenings. As a result, beneficiaries struggle to find dentures, hearing aids, or corrective lenses . People who join Medicare Advantage may select a plan that includes these services.
If these services are available via your states Medicaid program, you may be able to take advantage of them. However, not all states will provide coverage, and even if they do, it may not be available to everyone who meets the Medicaid eligibility requirements.
Unitedhealthcare Senior Care Options Plan
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
You May Like: Can Medicare Be Used Out Of State
Medicare And Medicaid: How To Qualify For Both
Home / FAQs / General Medicare / Medicare and Medicaid: How to Qualify for Both
Medicare and Medicaid are government healthcare programs for individuals with specific needs. Often, eligibility for the two forms of coverage overlap, and recipients can benefit from both programs.
Get A Free Quote
Find the most affordable Medicare Plan in your area
However, just because you qualify for one program does not mean you will automatically be eligible for the other. Medicare is a federal program, while Medicaid is a state program, so eligibility qualifications can vary from state to state for Medicaid. Below, we review the differences between Medicare vs. Medicaid and how you can utilize their benefits.
Dual Eligible Special Needs Plans
In some states, dual eligible beneficiaries may have the option of enrolling in a D-SNP, which is different from a traditional SNP or Special Needs Plan. These plans are specially designed to coordinate the care of dual eligible enrollees. Some plans may also be designed to focus on a specific chronic condition, such as chronic heart failure, diabetes, dementia, or End-Stage Renal Disease. These plans often include access to a network of providers who specialize in treating the specified condition. They may also include a prescription drug benefit that is tailored to the condition.
You May Like: How To Find Medicare Number
What Does Medicare And Medicaid Pay For
Medicaid is known as the payer of last resort. As a result, any health care services that a dual eligible beneficiary receives are paid first by Medicare, and then by Medicaid. For full dual eligible beneficiaries, Medicaid will cover the cost of care of services that Medicare does not cover or only partially covers . Such services may include but are not limited to:
- Nursing home care
- Dental services
- Eye examinations for prescription glasses
The financial assistance provided to partial dual eligible beneficiaries is outlined in the table above.
Medicare Dual Eligible Special Needs Plans
Another type of coverage that may be available to dual eligible beneficiaries is a Medicare Dual Eligible Special Needs Plan .
A Medicare special needs plan is a certain type of Medicare Advantage plan that is designed for people with specific health conditions or circumstances.
A D-SNP is built for the specific needs of dual eligibles. All Medicare SNPs provide prescription drug coverage.
Read Also: Does Medicare Pay For Tdap Shot
What Is A Dual
Dual-eligible beneficiaries are also eligible for a certain type of Medicare Advantage plan called a Dual-Eligible Special Needs Plan .
Medicare Advantage plans, also known as Medicare Part C, are sold by private insurers. By law, they must provide all of the same basic coverage as Medicare Part A and Part B. Medicare Advantage plans may also offer additional benefits that Original Medicare doesnt cover, such as coverage for dental, vision, hearing aids, prescription drugs and more.
A Special Needs Plan is a specific type of Medicare Advantage plan that is designed for beneficiaries who have certain health conditions or financial circumstances. A Dual-Eligible Special Needs Plan contains coverage that is tailored for someone with low income and resources. Prescription drug coverage is automatically a part of D-SNPs.
You can browse Medicare plans online and compare any Medicare-Medicaid D-SNP plans that may be available where you live.
Can You Have Medicare And Medicaid At The Same Time
Medicare and Medicaid are both public health insurance programs. If you are dual eligible, you can have both Medicare and Medicaid coverage at the same time.
Two of the key differences between Medicare vs. Medicaid include:
- Medicare is for people age 65 and over and for certain people under 65 who have a qualifying disability. Medicare eligibility is consistent for everyone across the U.S., no matter what state you live in.
- Medicaid is for people of any age who meet certain income qualifications. Medicaid is administered by state governments, and eligibility requirements can differ between states.
Read Also: Does Medicare Pay For Contact Lenses
How Do I Know If I Qualify For Medicaid And Medicare
Twelve million individuals are currently enrolled in both Medicaid and Medicare.1 These individuals are known as dual eligible beneficiaries because they qualify for both programs. As long as you meet the federal qualifications for Medicare eligibility and the state-specific qualifications for Medicaid eligibility, you will qualify as a dual eligible. To qualify for Medicare, individuals generally need to be 65 or older or have a qualifying disability.
There are several levels of assistance an individual can receive as a dual eligible beneficiary. The term full dual eligible refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as partial dual eligible.
*Cost sharing is the amount of your health care that you pay out of your own pocket. Typically, this includes deductibles, coinsurance, and copayments.
Income Tiers For Dual Eligibility
Each state sets its own income limits for Medicaid eligibility. Thus, the income tiers for dual eligibility will also vary from state to state.
A reasonable benchmark to use for Medicaid eligibility in 2021 is 138% of the federal poverty level. The federal poverty level is a measure of annual income issued every year by the Department of Health and Human Services to determine eligibility for Medicaid and certain other assistance programs.
For 2021, the federal poverty level for the continental 48 states and the District of Columbia is:
- $12,880 for individuals
- $17,420 for a family of 2
- $21,960 for a family of 3
- $26,500 for a family of 4
- $31,040 for a family of 5
- $35,580 for a family of 6
- $40,120 for a family of 7
- $44,660 for a family of 8
Federal poverty levels differ in Alaska and Hawaii.
Most states use an income of no more than 138% of the federal poverty level in order to be eligible for Medicaid. For example, a family of 3 in Arizona would need a household income of no more than $30,304.80 in order to be eligible for Medicaid.
If a member of that family is also eligible for Medicare because of their age or a disability, they would be dual eligible.
Some states have different income tiers for families and individuals. You can explore a complete online list of state income tiers for Medicaid eligibility.
Read Also: Will Medicare Pay For A New Mattress
