Medicare Special Needs Plans: What Are They And How Do They Work
Posted: June 19, 2020
Special needs is a broad term that describes people who face a wide range of challenges. Maybe you have a disability. Or a serious, ongoing medical problem. Having low income could also play a role. This article explains the different types of health plans for people with special needs. If its for you, a family member or youre a caregiver, its good to know all your options.
If youre dual-eligible, its likely that most of your costs will be covered.
When Can I Enroll In A Medicare Snp
You may enroll in a Medicare SNP during the annual Medicare Open Enrollment Period that runs from every year.
You may also enroll in a Medicare SNP if you are granted a Special Election Period. You may be given a Special Election Period if:
- You already have Medicare and then develop a chronic health condition
- You move into a nursing home or other long-term care facility
- You move out of your current SNP coverage area
- Your SNP leaves the Medicare program
- You become eligible for Medicaid
Like other types of Medicare Advantage plans, Medicare SNPs will vary in terms of cost, coverage and availability from one location to the next.
What Is A Medicare Advantage Special Needs Plan
Medicare is a health insurance program run by the federal government. It is also known as Original Medicare. It provides medical and health-related services to:
- People age 65 and older.
- People of any age who are qualified as disabled.
- People of any age who have kidney disease, including End-Stage Renal Disease , that requires dialysis or a transplant.
- People of any age who have Lou Gehrig’s disease .
Medicare is made up of 4 parts: Part A, Part B, Part C, and Part D.
Part A is hospital coverage. It helps cover the costs of being in the hospital as an inpatient, as well as long-term hospitalization. Most people automatically get Part A at no monthly cost.
Part B is medical coverage. It helps cover your doctor visits and outpatient care as well as some preventive services that help maintain your health. Medicare Part B has a monthly premium. Once you meet a certain amount of spending, known as your deductible, Part B generally covers about 80 percent of your costs for Medicare-approved services.
Part C is also known as a Medicare Advantage Plan. Part C is provided by plans like Keystone First VIP Choice that have been approved by the Centers for Medicare and Medicaid Services and have contracts with Medicare to cover medical and hospitalization care for their members. They can also offer extra benefits that original Medicare doesn’t cover, such as hearing, dental and vision services.
Recommended Reading: Can You Change Medicare Plans After Open Enrollment
How Do I Enroll For A D
If you are eligible for the Dual Special Needs Plan .
D-SNP eligible can enroll during the regular Medicare advantage enrollment period or Special Enrollment Period . The Special Enrollment Period is for s is once every quarter.
If you meet Medicare special needs plans eligibility, or you recently lost eligibility, you can make a change every three months. A person can enroll in D-SNPs during the following Medicare enrollment periods:
- During Open Enrollment Period from October 15th to December 7th
- In the Special Enrollment Period if there is a change in a persons circumstances, such as relocating to a new area.
For those who, for some reason, lose their Medicaid eligibility, they have a Special Enrollment Period starting at that particular month they receive the notice of the loss of eligibility plus two additional months to make an enrollment choice.
Note that, a beneficiary can only remain enrolled in a Special Needs Plan as they meet the eligibility requirement of the plan. If their health situation improves and they no longer meet the enrollment requirements for the Special Needs plan, they will get a Special Election Period to switch to a different Medicare Advantage plan or return to Original Medicare.
Medicare Advantage Vs Medicare Advantage Snp
There are a few differences between a traditional Medicare Advantage plan and a Medicare Advantage Special Needs plan. The following must be allowed or included in a Medicare SNP:
- You CAN enroll in a SNP if you have End Stage Renal Disease
- All SNPs must include prescription drug coverage
- Plans are specific to your needs
- You CAN enroll in a Medigap plan while enrolled in Medicare Advantage SNP
To learn if you qualify for a Medicare Special Needs Plan call the number above or contact Senior65.
Related Articles:
- Pros and Cons of Medicare Advantage Finding the right Medicare insurance can be rather confusing for seniors – especially when parsing through the 150-page “Medicare and You” booklet that the government sends out as you approach age 65. We have made a list of the advantages and disadvantages of choosing a MA plan that should help you understand if this product is right for you.
- Medigap Overview You may already know that Medicare covers you up to 80%. A Medigap plan will take care of the remaining 20%. This means that whatever Medicare covers, Medigap will cover too.
- New to Medicare: Everything you need to know. Medicare is the United States federal health insurance program for Americans 65 and older, as well as people with certain disabilities or End Stage Renal Disease .
Recommended Reading: Does Medicare Pay For Entyvio
How Medicare Special Needs Plans Work
Medicare Special Needs Plans are a type of Medicare Advantage Plan. All Medicare Advantage plans must cover the same Medicare services. But some Medicare SNPs are for people with specific diseases or challenges. These plans may tailor benefits, doctors and drug choices to match the needs of the groups they serve.
What Are The Benefits Of Medicare Advantage Special Needs Plans
Medicare Advantage Plans, including SNPs, offer many benefits beyond Original Medicare.
Original Medicare is limited to:
- Hospitalization
- Primary care coverage
- Optional prescription drug plan at an additional cost
An SNP will offer several benefits to take advantage of to either bring you back to good health or maintain your health:
- Original Medicare benefits hospital and primary care)
- Prescription drug coverage
- Meals after a major surgery
- A care manager or care coordinator assigned to help coordinate your care
Also Check: Does Medicare Cover Oxygen At Home
Who Is Eligible For Medicare Snps
To be eligible for a Special Needs Plan, you must qualify for a C-SNP, I-SNP, or D-SNP, and you must already be enrolled in both Medicare parts A and B, or a combination also known as Part C.
Apart from that, youll need to qualify for a specific type of SNP based on the rules of that plan, such as having a medical diagnosis or certain level of income.
Companion Care With Papa
Up to 8 hours of in-person or virtual companion care visits each month.
Papa connects college students to Medicare members who need assistance with transportation, house chores, technology lessons, grocery delivery, companionship, and other senior services. All plans with Papa include Papa Care Concierge. A team of caring individuals who can help you navigate your benefits, schedule doctor appointments, find providers and so much more.
You May Like: Are Medicare Advantage Plans Hmos
What Is Covered By A Medicare Snp
A Medicare SNP includes all of the Medicare services under one program, offering hospitalization , medical care , and prescription drug coverage .
Under this type of plan, you have coverage for your doctors visits, hospital stays, medications, and other services that you may need to manage your health.
The main difference between SNPs and other Medicare Advantage options is that SNPs offer extra services based on your unique healthcare needs. This may include an allowance for extra days in the hospital, a care management specialist, or other social services.
The Truth About Medicare Special Needs Plans
Some of the most advanced and innovative Medicare Special Needs Plans are those that offer D-SNP or Drug Subsidy. This is a plan that will not only cover your drug costs, but also offers protection against high out-of-pocket expenses incurred by co-payments, coinsurance, and deductibles.
These plans can be very beneficial for senior consumers who have chronic conditions such as diabetes, arthritis, or heart disease requiring them to take expensive medications on a daily basis.
The truth about these plans? They are available without regard for age or income level and they provide coverage for drugs even if you cannot get them through your prescription drug plan.
Read Also: What Age Can You Get Medicare Health Insurance
Chronic Conditions Snps Apply To
If you have cancer or heart disease, you could get a SNP. Those are among the 15 chronic conditions that SNPs cover. Other examples are autoimmune disorders, diabetes, dementia, lung disease, and end-stage liver and kidney diseases. A SNP may focus on one chronic condition or several.
For a full list of conditions, go to Medicare.gov and search special needs plan.”
Medicare Special Needs Plans
There are a variety of federal and state-run programs available to help Medicare beneficiaries with specialized health or financial needs. Some of these situations might include:
- High-risk groups of individuals having one or more severe or disabling chronic condition.
- Living in an institution.
- Being eligible for Medicaid.
If youre a Medicare beneficiary with one of the above circumstances, you may not realize that there are Medicare plans available that are specifically designed to help you manage the complex health challenges that may come with your situation.
Special Needs Plans tailor their benefits and services for Medicare beneficiaries with unique health or situational challenges. Heres an overview of how they work, including what they cover, eligibility, and how to enroll.
You May Like: How To Reorder Medicare Card
When You Can Enroll
Automatic enrollment doesnt occur with SNPs, and typically you would join a SNP during set Medicare Advantage enrollment periods.
Special enrollment periods are also offered for a number of reasons, including a change in your health conditions, employment status, where you live, or the plan you have.
Special enrollment is offered to anyone with both Medicare and Medicaid as long as you are enrolled in both programs. People who need to move to a higher level of care or into a nursing home, and those with disabling chronic illness, can enroll in an SNP at any time.
What Are The 3 Types Of Special Needs Plans
There are three types of Medicare Special Needs Plans:
- Dual-eligible Special Needs Plans These plans are designed for people who are dual-eligible, or eligible for both Medicare and Medicaid.
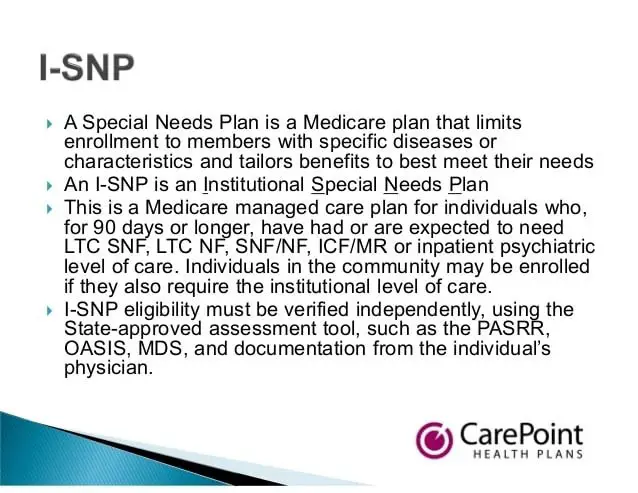
- Institutional Special Needs Plans These plans are for people who are institutionalized in a nursing home or require nursing care at home.
- Chronic Condition Special Needs Plans There are 15 different health conditions that may have a corresponding Medicare Special Needs Plan:
- Chronic alcohol and drug dependence
- Certain autoimmune disorders
Keep in mind, Special Needs Plans may not be available where you live.
You May Like: Which Insulin Pumps Are Covered By Medicare
How Do I Enroll In A Medicare Special Needs Plan
You may join a Medicare Special Needs Plan during the same enrollment periods used for standard Medicare Advantage plans.
These enrollment periods include:
- Initial Enrollment Period Your Medicare IEP is a seven-month period that begins three months before you turn 65 years old, includes the month of your birthday and extends for three more months thereafter.
- Annual Enrollment Period The Medicare AEP takes place every year from .
- Special Enrollment Period You may be granted a Special Enrollment Period at any time throughout the year, depending on your circumstances. You may potentially qualify for an SEP if you go through a qualifying event, such as moving to a new service area, losing employer coverage, being released from a long-term care facility and more.The length of your Special Enrollment Period and the effective date of coverage changes you make may vary depending on your qualifying circumstances.
You can learn more about Medicare Special Needs Plans by visiting MedicareAdvantage.com.
1 CMS. SNP Comprehensive Report . Retrieved June, 2019, from www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MCRAdvPartDEnrolData/Special-Needs-Plan-SNP-Data-Items/SNP-Comprehensive-Report-2019-05.html.
Christian Worstell is a health care and policy writer for MedicareSupplement.com. He has written hundreds of articles helping people better understand their Medicare coverage options.
Who Is Eligible For A Dual Special Needs Plan
If you are qualified for both Medicare and Medicaid and have a specific disabling or severe chronic condition, then you are eligible for D-SNP.
To qualify for Medicare, an intending enrollee must be 65 years or older or have a qualifying disability. On the other hand, to qualify for Medicaid income and asset level of intending you must fall below a certain threshold as determined by your state.
The Dual Special Needs Plan is there to address the health needs of those who fall in the above categories.
DSNP beneficiaries often face special health needs and could use such coordinated assistance to improve their health and quality of life. For example, they may be experiencing the following:
- A disabling condition and difficulty with routine activities such as bathing and dressing
- A mental disorder or cognitive impairment
- Have a variety of health conditions and require care from multiple doctors to manage their health
- Incapacitated by an underlying health condition and require the services of in-home care providers and other health and social services.
Also Check: When Does Medicare Coverage Start
What Are The Benefits Of Medicare Snps
- Coverage for routine dental, vision, and hearing care
- Transportation to medical appointments
- Fund for over-the-counter products, such as toothpaste, supplements, blood pressure monitors, and more
- Routine foot care, such as clipping of toenails
- Incentives, such as gift cards, for fulfilling preventive screenings
An SNP plan will replace your Original Medicare. Additionally, Medicare Advantage Special Needs Plans always include Part D prescription drug coverage.
How To Sign Up For A Medicare Snp
First, find a SNP in your area.
- Go online to the Medicare Plan Finder website: www.medicare.gov/find-a-plan.
- Contact your local State Health Insurance Assistance Program. People there can help you sign up for a Medicare SNP.
Then, fill out an application form. You can ask the SNP to send you a form. Some SNPs will let you sign up through their website. Or if you have Medicare and Medicaid, you may be able to sign up at Medicare.gov. For more help, call 800-MEDICARE.
You May Like: Does Medicare Pay For Maintenance Chiropractic Care
How Special Needs Plans Work
Special Needs Plans are a type of Medicare Advantage plan for beneficiaries who meet certain eligibility criteria. Like other types of Medicare Advantage plans, these plans are available through Medicare-contracted private insurance companies. Each type of plan limits enrollment to the group that it targets, and there are three kinds:
- Chronic-Condition Special Needs Plans are for beneficiaries with severe or disabling chronic health conditions. There are 15 conditions approved by the Centers of Medicare & Medicaid Services .
- Institutional Special Needs Plans are for beneficiaries who live or are expected to live in an institution or require nursing care in their home for 90 days or more. This includes assisted living or nursing homes, long-term care skilled nursing facilities, inpatient psychiatric facilities, or intermediate care facilities for people with developmental disabilities. Enrollment of a special needs individual on the basis of the potential for a 90-day stay must be based on a CMS-approved assessment.
- Dual-Eligible Special Needs Plans are for beneficiaries who have both Medicare and Medicaid, also known as dual eligibles.
What Do Medicare Snps Cover

Like all Medicare Advantage plans, Special Needs Plans will provide all of the same coverage as Medicare Part A and Part B.
Additionally, Special Needs Plans may feature a custom set of benefits designed specifically for the needs of the beneficiary.
All Medicare Special Needs Plans include prescription drug coverage.
You May Like: How To Order A Medicare Card
How Do I Enroll In A Medicare Advantage Special Needs Plan
There are several ways to enroll in an SNP. If you are eligible for Original Medicare and meet the SNP criteria, you can enroll at any time. Also, you have to meet the criteria of the SNP that you are applying for.
Before joining a Medicare SNP, research to ensure the plan is right for you, then shop again every year for a plan that suits your needs. If you need help, take advantage of resources that can assist you in the process of choosing a plan and enrolling, such as a licensed health insurance agent or local Area Agency on Aging.
You have multiple options for enrollment:
- Phone: You can apply over the phone by calling Medicare at , or you can also contact the plan of your choice directly.
- Online: You have the option of enrolling online through a third-party website or the plans website.
- Insurance agent: If you decide to recruit an agent for assistance, you will enroll either by paper or electronic application.
Before making a decision, ensure youre well informed and all of your questions get answered.
- Featured Sources
Whats It Cost To Join A Medicare Special Needs Plan
If you have both Medicaid and Medicare, its likely that most of your costs will be covered for you. If you don’t have Medicaid, your exact costs may depend on the plan you choose. In general, you’ll pay the basic costs of having a Medicare Advantage plan.
See UnitedHealthcare plans in your area.
Please note: What dual-eligible plans you can get depends on where you live. To find a UnitedHealthcare Dual Complete® plan for you, please search plans in your state.
Visit UHCMedicareSolutions.com to find out more about the C-SNPs, I-SNPs, and IE-SNPs we offer.
Resource Center
Were here to help.
Contact us at:
Were here to help.
Contact us at:8 a.m. to 8 p.m. local time, 7 days a week.
Recommended Reading: Does Medicare Advantage Pay For Hearing Aids
