Does Medicare Cover Inpatient Mental Health Treatment
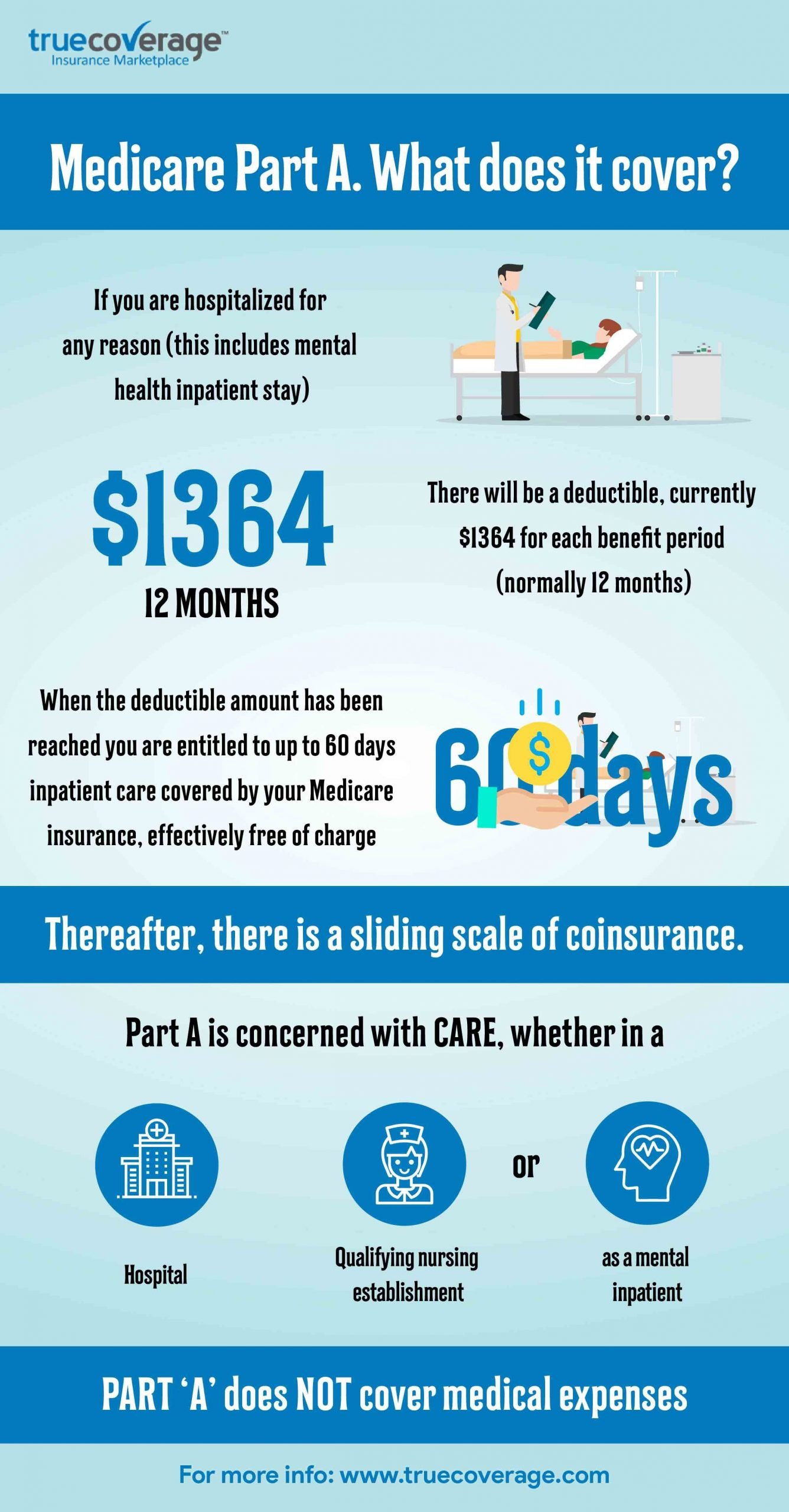
You must have Medicare Part A to be covered for inpatient mental health treatment at a general or psychiatric hospital. Medicare will pay for most of your inpatient treatment services. However, you may still owe some out-of-pocket costs depending on your plan and the length of your stay.
Here are the basic costs for Medicare Part A:
- $252458 premium, if you have one
- $1,408 deductible
- 20 percent of all Medicare-approved costs during the stay
- $0 coinsurance for days 160 of treatment
- $352 coinsurance per day for days 6190 of treatment
- $704 coinsurance per day for days 91+ of treatment, through your lifetime reserve days
- beyond your lifetime reserve days, youll owe 100 percent of the treatment costs
Its important to note that while theres no limit to how much inpatient care you can receive in a general hospital, Part A will only cover up to 190 days of inpatient care in a psychiatric hospital.
Who Qualifies As A Caregiver Under Medicare Rules
Who’s eligible?
- You must be under the care of a doctor, and you must be getting services under a plan of care created and reviewed regularly by a doctor.
- You must need, and a doctor must certify that you need, one or more of these: …
- You must be homebound, and a doctor must certify that you’re homebound.
Read also
Do I Qualify For Medicare Mental Health Coverage
If youve been diagnosedwith a mental health condition, you most likely qualify for the mental healthservices that Medicare offers. Common conditions include anxiety, depression,addiction, and eating disorders. Symptoms of mental health conditions caninclude, but arent limited to:
- Loss of interest/lack ofenergy
- Feeling of hopelessness
- Poor appetite
- Suicidal thoughts oractions
If you or someone youknow is experiencing these symptoms, proper treatment can help tremendously.
You May Like: How Do I Change Medicare Supplement Plans
Medicare Outpatient Mental Health Services
Medicare Part B covers outpatient mental health services, such as care youd get in a health clinic or doctors office. Youll generally pay 20% of the Medicare-approved cost for outpatient care delivered by providers that accept Medicare assignment.
Medicare covers the following types of psychotherapy :
- Psychiatric assessment
- Family counseling, when the primary goal is to treat your condition
- Alcohol misuse counseling, up to four sessions
You may need to meet other criteria to be eligible for therapy coverage, and the doctor, psychologist, or other health-care professional must accept Medicare assignment. Medicare doesnt cover certain types of therapy, such as pastoral counseling or marriage counseling.
If you need more structured or frequent treatment, Medicare Part B also covers partial hospitalization programs, which are outpatient mental health programs where treatment is provided throughout the day and doesnt require an overnight, inpatient stay. The programs are usually run through a community mental health center or a hospitals outpatient department. Services may include therapy with a mental health professional, diagnostic services, and occupational therapy . These programs dont cover meals or transportation to the facility.
Does Medicare Cover Mental Health
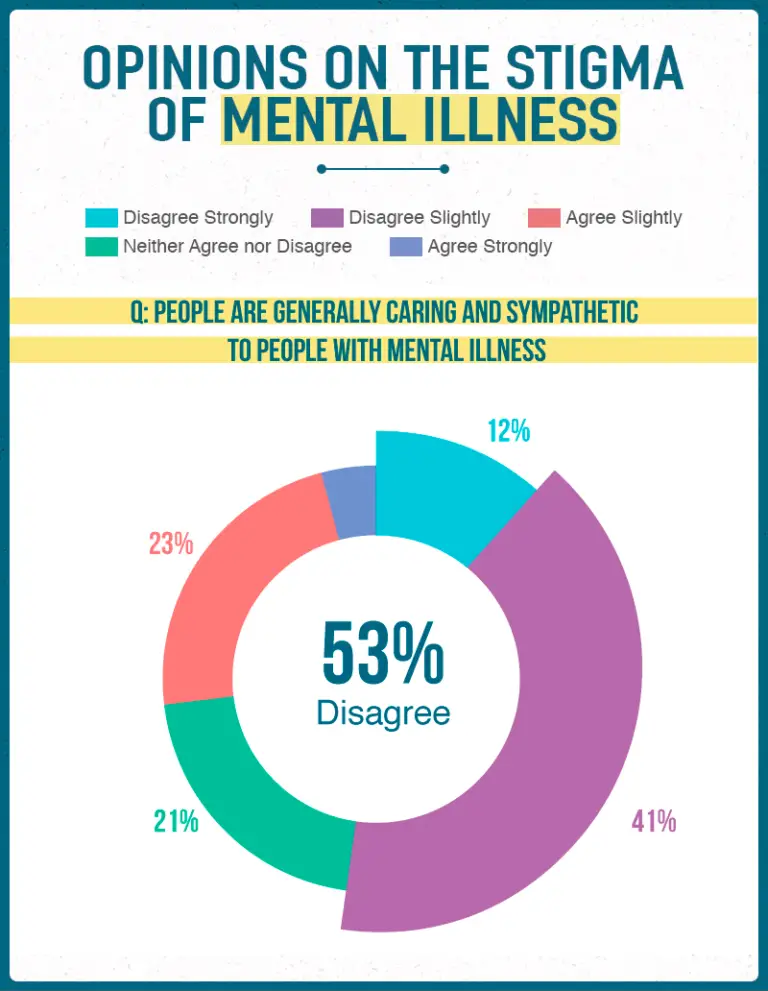
Mental health conditions affect many people, and people who experience them for the first time later in life may have a hard time recognizing them. Without proper mental health care these conditions can be severe and even life-threatening. Fortunately, the stigma associated with asking for help is disappearing, and Medicare offers coverage for many mental health services.
Recommended Reading: How To Calculate Medicare Wages
How Much Does Medicare Reimburse For Psychiatrist
Medicare rebates of about $125 per standard consultation are available for up to 10 sessions, if a Medical Practitioner or Psychiatrist refers you through completing a Mental Health Care Plan. Alternatively, Private Health Fund rebates can be claimed if your policy covers you to see a Clinical Psychologist.
Mental Health Credentialing Recommendations
In our experience, the higher the reimbursement rate, the higher your license level need be to become in-network with that company.
If you want to become in-network with higher paying, lower fuss plans, it is likely youll need a longer amount of experience and possibly a track record of working with that plan as a provider in a previous group or agency.
Some companies, such as many of the BCBS plans, require you to establish a business, E-IN, and group NPI.
For mental health credentialing, we are quick to recommend Aetna, Cigna, and if your license allows it, Medicare .
Also Check: Does Medicare Cover Chronic Pain Management
Is Facetime Allowed For Telehealth
Under this Notice, covered health care providers may use popular applications that allow for video chats, including Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, Zoom, or Skype, to provide telehealth without risk that OCR might seek to impose a penalty for noncompliance with the HIPAA Rules.
Medicare And Mental Health Coverage
When a person first enrolls in Medicare, they receive a Welcome to Medicare preventive visit. During this visit, a doctor reviews risks of depression.
Yearly wellness visits can then include discussions with a persons doctor on any changes to mental health that may have occurred since the last visit.
In addition to the wellness visits, Medicare covers certain mental health services both inside and outside of a hospital.
Read Also: Will Medicare Pay For Diapers
What Are The Medicare Annual Limits For Mental Health Provider Services
The law limits Medicare payments for outpatient mental health to 62.5% of expenses in the calendar year. Services include the treatment of mental, psychoneurotic, and personality disorders for people not inpatient in a hospital. These limitations DO NOT apply to diagnosis, but rather, they apply to treatment.
Why Is Medicaid Hard To Bill For Mental Health Providers
For the same reason that Medicare is hard to bill, except that each state has their own contract instead of each region . As such, your states Medicaid policy is up to them.
Each state may have their own system that they have built that might be slow and require many enrollments as well, or they might contract out the insurance coverage to existing commercial insurance companies.
Example: What you think is UHC is actually Medicaid via UHC and while youre in-network with UHC, youre out of network with their Medicaid network your claims get denied.
Make sure you understand exactly which Medicaid panels you are enrolling with, including if youre in-network with their commercial or Medicaid or HMO or PPO or EPO plans.
You May Like: How Do You Qualify For Medicare Part A And B
Does Medicare Cover Psychotherapy
Psychotherapy, which is commonly referred to as talk therapy, can be used to treat a wide variety of mental heath needs. If you find that your daily routines or lifestyle are inhibited by your psychological well-being or emotional stability, psychotherapy may provide effective treatment. Medicare benefits may help cover the costs of certain types of therapeutic services.
Overview of Psychotherapy
As described by the American Psychiatric Association , psychotherapy uses a number of techniques to help patients improve their mental health by addressing troublesome behaviors and emotional difficulties. Your needs as a patient will dictate the exact type of therapy your healthcare professional suggests. This can include individual sessions or joint sessions as a couple or family.
Certain medications that help alleviate chronic symptoms of mental illness may also be used in combination with regular therapy sessions. Both medication and therapy may be used for short and long-term treatment.
Some diagnostic tests may be prescribed if neurological factors are suspected to contribute to mental illness or emotional disturbance. Other tests may be required in order to monitor any medications impact on the body, such as checking blood pressure or liver and kidney function.
Types of Psychotherapy Treatment
In other cases, your therapist may specialize in one or two styles of therapy that address specific types of mental health needs. The most common forms of therapy include:
How Do Psychologists Bill Medicare
This visit should be billed using a CPT code for psychotherapy with E/M, but Medicare limits the psychologist to billing only for the time spent on psychotherapy. The time spent by the psychologist monitoring the patients progress on medication, a critical element of psychotherapy with E/M, is not accounted for.
Don’t Miss: Does Medicare Cover Any Dental Surgery
Is A Landline Hipaa Compliant
Phone calls to patients are HIPAA compliant provided the nature of the phone call falls within the reasons for which a patient is considered to have given their consent. If a phone call to a patient relates to any other subject, the Covered Entity must have consent from the patient before making the call.
Top 4 Insurance Companies For Established & High License Level Providers
Best suited for LCSWs, PsyD, PhD, and MDs:
Investigate which companies are paying the most in your State by asking your colleagues.
Tip: You will probably need to establish a separate legal business to work with these companies so expect to create an E-IN for your new practice to get paid the best rates.
Also Check: How To Enroll In Original Medicare
Does Medicare Cover Therapy
In short, yes, Medicare does help pay for therapy and a variety of other mental health services. However, it’s important to note that to receive this coverage, beneficiaries must be enrolled in Medicare Part B, which includes both medically necessary and preventative services for its members. Additionally, there are some limitations to the services that can be accessed, and beneficiaries may be required to pay a deductible and a co-pay, depending on the service they access.
Does Medicare Cover Family Counseling
Medicare Part B may help pay for family counseling if the goal of the therapy is related to helping your treatment. In addition, grief and loss counseling may be covered by Medicare for qualified hospice patients and their families, if it is provided by a Medicare-approved hospice and available in that state. Medicare does not cover other types of relationship counseling, such as marriage counseling. Youre only covered for mental health services from a licensed psychiatrist, clinical psychologist, or other health care professional who accepts Medicare assignment.
Don’t Miss: What Is Medicare Premium Assistance
How Much Does Medicare Pay For Mental Health Counseling And Other Services
WhileMedicare offers many mental health services, it doesnt usually cover theentire costs. Original Medicare alone typicallyonly pay up to 80% for your inpatient or outpatient services, excluding othercharges like copays and deductibles. Original Medicare also doesnt typicallycover your prescription medications. There are several solutions to helpcontrol your costs:
- Medicare Supplement Plans: Medicare Supplement plans come in a range of coverage options, and help cover the gaps in the services that Medicare pays for. For instance, if you have Medicare Supplement Plan G, you may have no other out-of-pocket costs after you pay your yearly deductible, which is $203 in 2021. Youre able to keep Medicare as your primary coverage, but they dont offer any prescription coverage.
- Medicare Part D Prescription Plans: These plans help cover the costs of your prescription medications. They vary in coverage by carrier and zip code, and your costs may also change depending on which pharmacy you receive your prescriptions from.
- Medicare Advantage Plans: Medicare Advantage plans are primary instead of Medicare. Some of them offer prescription coverage, and they may reduce your out-of-pocket costs for mental health services compared to Original Medicare alone. If you have a Medicare Advantage plan, you should refer to it directly for details on costs and coverage.
Does Medicare Cover Mental Health Services
Many or all of the products featured here are from our partners who compensate us. This may influence which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list ofour partnersandhere’s how we make money.
Medicare pays much of the cost of a wide range of mental health services, whether provided on an outpatient basis or for inpatients in a psychiatric or general hospital. But you need to be aware of limits on these benefits, including substantial copays, coinsurance and a lifetime maximum.
Mental health issues are common among older adults: Thirty-one percent of Original Medicare beneficiaries are living with mental illness, according to a July 2020 report by the Commonwealth Fund, a private foundation focused on health care. And in a July 2020 survey by the Kaiser Family Foundation, 46% of Americans ages 65 and up said that pandemic-related stress and worry were detrimental to their mental health.
You May Like: Do Doctors Have To Accept Medicare Advantage Plans
Other Parts Of Medicare
Although parts A and B cover most of your mental health needs, you can get additional coverage by enrolling in the following Medicare plans:
- Medicare Part C: automatically covers all Medicare Part A and Part B services, plus prescription drugs and other coverage areas
- Medicare Part D: can help cover some of your mental health medications, including antidepressants, anti-anxiety medications, antipsychotics, mood stabilizers, etc.
- Medigap: can help cover some fees associated with your inpatient or outpatient care such as coinsurance and deductibles
If youre ready to seek mental health treatment, visit the Substance Abuse and Mental Health Services Administrations website to find behavioral health treatment services near you.
Why Is Medicare Hard To Bill For Mental Health Providers

Medicare subcontracts out to many different subcontractors like Noridian or Palmetto or Novitas or NGS or WPS or FCSO.
Each contractor has their own electronic claims submission enrollment requirements, forms, and process. Each system is clunky and the enrollments take quite some time. Most clients also have a secondary insurance company to bill alongside their Medicare coverage.
We take care of this enrollment process and secondary claims submission and follow-up for our providers at TheraThink.
Don’t Miss: What Is The Best Medicare Supplement Insurance Plan
Medicare Advantage And Mental Health Care
Medicare Part C, more commonly known as Medicare Advantage , allows Medicare beneficiaries to combine their Part A and Part B benefits into a single health insurance plan. MA plans are sold by private insurance companies and resemble the group health plans many of us had through an employer.
Every Advantage plan must provide the same benefits you get with Original Medicare. However, most of them provide additional coverage as well. The most common is prescription drug coverage, which is included with around 90 percent of MA plans. Coverage and costs vary, so look at the plan carefully to understand which extra benefits it includes.
You cannot have both Medigap and a Medicare Advantage plan.
Our Find a Plan tool makes it easy to compare your Medicare plan options. Just enter your location to start reviewing Medicare plans in your area.
Does Medicare Cover Counseling
Medicare Part B covers outpatient mental health care including the following services:
- Diagnostic testing
- Activity therapies like art, dance, and music therapy
- Family counseling to address a mental health condition
- Drugs that usually aren’t self-administered
- An annual depression screening with a primary care physician
- An annual alcohol misuse screening with a primary care physician
Medicare Part B has an annual deductible that changes over time. It was $134 in 2018 and will be $135.50 in 2019. After the deductible, Medicare covers 80% of outpatient services, leaving people to pay a 20% coinsurance on the Medicare-approved amount for that service.
Read Also: How Much Is Premium For Medicare
Medicare Coverage Of Counseling And Mental Health Services
Caring for your mental well-being is just as important as taking care of your physical health. As you get older, you might feel sad or frustrated sometimes, especially when you have health problems. However, if youre feeling persistently sad or anxious or having thoughts of suicide, your doctor can be a good resource for helping you get the care you need.
Medicare covers many mental health services to help you stay healthy, such as psychological counseling services, diagnostic evaluations, and preventive screenings.
How Much Does Counseling Cost
The cost of counseling without coverage varies by the area, the counselors specialization, and the length of counseling sessions. Counseling costs usually range between $65 to $250 per hour, but they can be higher if the counselor has a greater reputation and specialization.goodtherapy.org, How much does therapy cost?, Accessed November 17, 2021
Medicare Part B will cover 80 percent of approved costs for counseling services ordered by your doctor once you have paid the annual Part B deductible. As an inpatient, Medicare Part A will cover all approved counseling services once the Part A benefit periodA benefit period is a method used in Original Medicare to measure a beneficiaries use of hospital and skilled nursing facility services. With each new benefit period, the beneficiary is charged a new benefit… deductible has been paid. If the counselor charges Excess ChargesA Medicare Part B excess charge is the difference between a health care providers actual charge and Medicares approved amount for payment…., you will pay those out-of-pocket unless you have a Medicare Advantage plan or a MedigapMedicare Supplements are additional insurance policies that Medicare beneficiaries can purchase to cover the gaps in their Original Medicare health insurance coverage…. policy that covers Excess Charges.
Recommended Reading: Which Medicare Part Covers Prescriptions
Medicare Prescription Drug Coverage For Mental Health Care
Original Medicare does not include prescription drug coverage . These benefits are available through a Medicare Part D prescription drug plan .
To get Medicare Part D, you may join either a standalone prescription drug plan or a Medicare Advantage Prescription Drug plan . Private insurance companies provide these plans, which means that costs and benefits vary.
If your mental health care provider prescribes medication to help treat your condition, your first step should be checking your Part D plan’s drug formulary. This is the list of prescription medications covered by your plan. Medicare requires all Part D plans to cover anticonvulsant, antidepressant, and antipsychotic medications. In other words, insurance companies cannot discriminate against Medicare beneficiaries who have a mental health condition.
When comparing Part D plans, create a list of prescription medications you take. Then, check the drug formulary to be sure it includes your prescriptions.
Medicare Part D plans typically make changes to their formulary throughout the year. For example, the FDA may pull a drug or approve a safer version of a medication, prompting prescription drug plans to change their formularies.
When the drug formulary changes, your PDP is required to notify you at least 30 days before making the change. Alternatively, they may notify you of the change the next time you fill your prescription, providing a final 30-day supply of your medication.
