Do All Medical Services Performed Require Prior Authorization
Prior authorizations are usually only required for more costly, involved treatments where an alternative is available. For instance, if a physician prescribes an invasive procedure such as orthopedic surgery, it will likely require preauthorization. An alternative therapy, like injecting the patient with Cortisone to reduce pain and inflammation, is less likely to require payer review.
Update Posted December 18 2012
We know that recently youve been experiencing some issues with J9035 and J9355 authorizations and we apologize for any inconveniences this may have caused. Our goal is to continue to work with you to help ensure that you are able to provide your patients the best care possible.
Effective, February 1, 2013, all participating Hematologists and Oncologists will be required to receive prior authorization before administering injectable drugs with costs over $250. If drugs are administered without authorization, the claim will be denied and the provider will not receive payment. There are some exceptions to this policy, so please call Provider Services to determine if a drug needs prior authorization.
We are reviewing denials weekly for claims that have been denied due to the new authorization requirements and will override these denials until January 31.
Original Medicare Medicare Supplement And Prior Authorization
The Social Security Act didnt require any form of prior authorization for Medicare services in the past. However, the law was altered to allow prior authorizations for specific services and items, such as durable medical equipment.
Although these changes were made to the act, prior authorization will only be necessary with Original Medicare in exceedingly rare circumstances. Medicare Part A rarely requires prior authorization as an inpatient. However, if you must have prior authorization, you would obtain the needed forms and submit them to Medicare.
Medicare Part B may require prior authorization whenever you are administered a specific drug in an outpatient facility. Some medications require your physician to submit a drug prior authorization form, which your physician would provide. Once the form is approved, Medicare will provide its share of coverage.
Overall, when you only have Medicare Part A and Part B, you wont have a network of providers, you can visit any hospital outside the state that accepts Medicare, and a referral is not needed to see a specialist.
Don’t Miss: Can I Submit A Claim Directly To Medicare
Does Medicare Require Prior Authorizations
Beneficiaries with Original Medicare generally do not need to obtain a prior authorization form for most Medicare services, such as doctors visits, hospitalizations, diagnostic studies or treatments.
Original Medicare beneficiaries may sometimes need to seek prior authorization for durable medical equipment and certain types of Medicare outpatient services.
Its not uncommon, however, for beneficiaries of Medicare Advantage plans and Medicare Part D Prescription Drug plans to need prior authorization before receiving some types of care.
Prior authorization is most common for getting certain prescription drugs covered by your plan. You may also need a prior authorization form if youre seeking care from an out-of-network provider.
What Is A Medicare Prior Authorization Form
- Medicare beneficiaries are sometimes required to obtain a prior authorization form for certain prescription drugs or medical services. We provide links to Medicare forms and explain why you might need them.
Prior authorization is a type of rule that requires a health care provider to get approval from Medicare before delivering a particular service, prescription drug or item to a beneficiary.
You dont typically need to get a Medicare prior authorization form, as your doctor, provider or pharmacist should be able to submit the form to Medicare on your behalf.
Don’t Miss: What Does Medicare Supplement Plan N Cover
Medicare Advantage Prior Authorization
To obtain out-of-network, specialist, and emergency care, Medicare Advantage recipients may need prior authorization. Unfortunately, if Medicare doesnt approve the request, the Advantage plan typically doesnt cover any costs, leaving the full cost to you.
Reports have shown that as many as four out of five members with Advantage plans require prior authorization for certain services. The services most often requiring prior approval are durable medical equipment, skilled nursing facility stays, and Part B drugs.
But, each Advantage plan is different. If you have an Advantage plan, contact your plan provider to determine if or when prior authorization is necessary. Your plan will have forms you can download online.
Also, Advantage members may appeal to their plans denial. Yet, most dont take advantage of this.
How Prior Authorization Can Impede Access To Care In Medicare Advantage
While Medicare Advantage plans are required to cover the same health services as Original Medicare, they are not required to offer the same level of provider access and can impose coverage restrictionslike prior authorizationthat require enrollees to take additional steps before accessing prescribed care. If a service is covered with prior authorization, enrollees must get approval from the plan prior to receiving the service. If approval is not granted or sought, the plan generally will not cover it.
A new analysis from the Kaiser Family Foundation looks at the prevalence of prior authorization in MA and found that many plans utilize this flexibility: 80% of MA enrollees are in plans that require prior authorization for at least one Medicare-covered service. Original Medicare, in contrast, does not require prior authorization for the vast majority of services, making this an important distinction between the two coverage options.
In some instances, prior authorization may be an appropriate utilization management tool. In particular this is true when both beneficiaries and providers are likely to benefit from advance knowledge of Medicare coverage. However, MAs broad application of prior authorization can impede access to care.
In such situations, there is minimal value to beneficiaries or providers in procuring pre-service determinations. Instead, these requirements can often create barriers that may delay or prevent timely access to needed, affordable care.
Read Also: Do Any Medicare Supplement Plans Cover Dental And Vision
What Is Electronic Prior Authorization
Electronic prior authorizations refer to those instances where some or all of a prior auth determination is processed electronically.
What constitutes an ePA is up for interpretation. Manual keystroke entries to a payer portal or an eFax might technically count as ePA, as would more sophisticated computer-to-computer information exchange using electronic data interchange or clearinghouse transmissions.
To more legitimately lay claim to offering an electronic prior authorization solution typically requires the following:
EDI capabilities, particularly the capability to send a 278 transaction. This is the standard protocol to electronically transmit patient data pertaining to authorizations and referrals between providers and payers.
- Integration with EHRs, LIMS, and other clinical and financial management systems.
- Direct connections with health plans.
- Rule sets that automate the submission and tracking of prior auth requests.
- Use of multiple web-based prior authorization applications for each payer/PBM with their own username and password requirements.
What Type Of Medical Information Is Commonly Requested When Submitting A Prior Authorization Form
While the format and requested information for a prior authorization form may differ from health plan to health plan, they will generally require that healthcare professionals provide the information below. Here is a sample prior authorization request form.
- Identifying information for the member/patient such as:
- Name, gender, date of birth, address, health insurance ID number and other contact information
You May Like: How To Make Medicare My Primary Insurance
Can A Prior Authorization Decision Ever Be Overturned
Yes.
If a health plan denies treatment or medication requested as part of the prior authorization process, the provider has the right to appeal on behalf of their patient.
The denial will often be communicated by phone from payer to provider first. A letter from the payer to provider will then follow. An Explanation of Benefits document will typically be sent from the payer to the patient.
The provider can then follow a formal appeals process specific to each payer. This can be a protracted, multi-step process that requires a material amount of time from providers and insurers alike.
- Level One: The initial phase begins with the doctor and patient contacting the payer to demonstrate that the requested treatment is medically necessary, and to request that the health plan re-evaluate the denial.
- Level Two: If the initial phase does not resolve the issue, the appeal is then escalated to a medical director at the carrier who has not yet been involved in the adjudication process. The medical director will evaluate whether the denial was properly assessed.
- Level Three: If the previous steps do not yield a satisfactory result for the provider and patient, the appeal may be taken to a more neutral party for review often a physician with a similar specialty as the appealing doctor, and an intermediary from the insurance company.
Does Medicaid Require Prior Authorization For Referrals
Today in the United States, Medicaid covers over 17 percent of all U.S. healthcare spending and assists with healthcare expenses for more than 75 million Americans of all ages. Where Medicare is a health insurance program, Medicaid is an assistance program that helps low income individuals and families with their medical needs and expenses.
Every U.S. state runs its own Medicaid program, but they are all based on federal guidelines. Each state has its own regulations regarding what services are covered, when written referrals are necessary, and which referrals require prior authorization.
Through Medicaid services, a referral is issued in writing by your primary care physician when he or she feels it is necessary for you to visit another health care provider for treatment or tests. A prior authorization for this referral is necessary in some cases. The authorization is issued by your Medicaid provider who reviews the case and allows you to visit the specialist or other health care provider.
Because states may vary in their requirements for coverage of services, referral allowances, and need for prior authorization, you should contact your local Medicaid office for details. Your health care provider can give you information also.
Non-formulary medications Hospice care Specialized care
If you need emergency room services or post stabilization services, these do not require prior authorization.
Related articles:
You May Like: What Is The Best Medicare Part D Plan For 2020
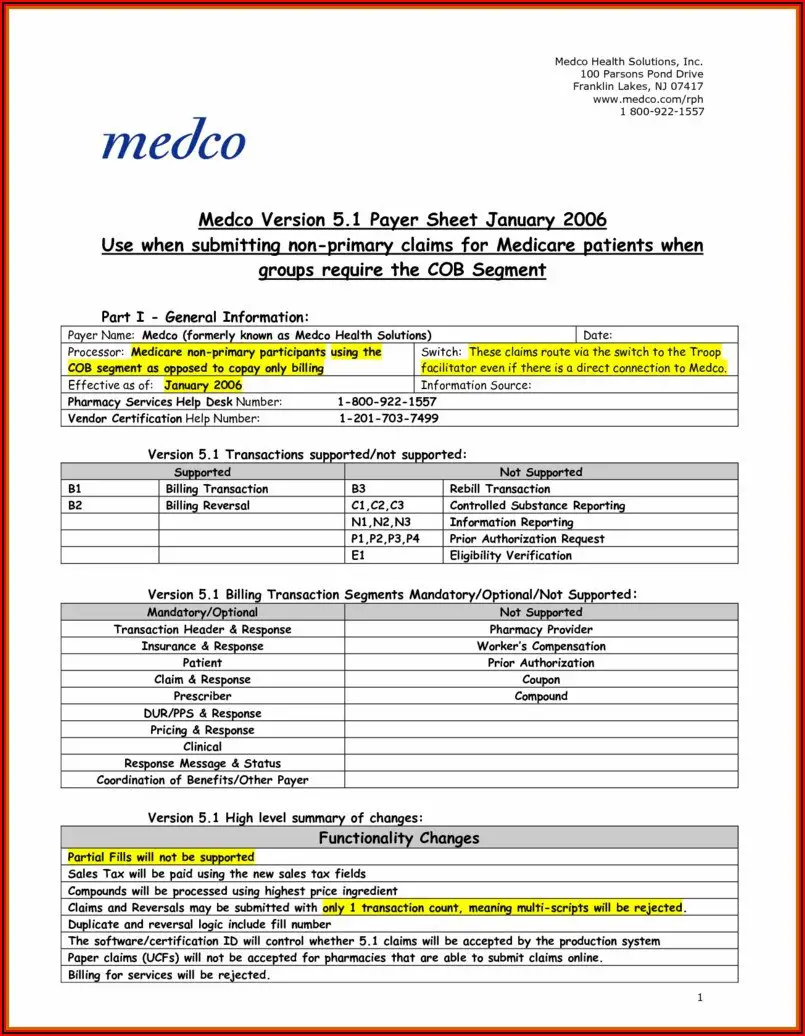
Medicare Announces Prior Authorization Requirement
Radiologists who perform venous ablation in a hospital outpatient department are now required to obtain prior authorization before performing such services on Medicare patients. This new requirement became effective for services performed on or after July 1, 2020, and physicians were notified by letters from the Centers for Medicare and Medicaid Services late in June. The prior authorization requirement was included in the 2020 Hospital Outpatient Prospective Payment System Final Rule, and encompasses the following procedures that might be performed by interventional radiologists:
|
Description |
|
|
36473 |
Mechanochemical destruction of insufficient vein of arm or leg, accessed through the skin using imaging guidance |
|
36474 |
Mechanochemical destruction of insufficient vein of arm or leg, accessed through the skin using imaging guidance |
|
36475 |
Destruction of insufficient vein of arm or leg, accessed through the skin |
|
36476 |
Radiofrequency destruction of insufficient vein of arm or leg, accessed through the skin using imaging guidance |
|
36478 |
Laser destruction of incompetent vein of arm or leg using imaging guidance, accessed through the skin |
|
36479 |
Laser destruction of insufficient vein of arm or leg, accessed through the skin using imaging guidance |
|
36482 |
Chemical destruction of incompetent vein of arm or leg, accessed through the skin using imaging guidance |
|
36483 |
Chemical destruction of incompetent vein of arm or leg, accessed through the skin using imaging guidance |
Is It Possible To Speed Up Prior Authorization
One of the primary reasons that prior authorizations take so long to resolve is that incomplete or incorrect information is submitted to the health plan, which triggers a denial and lot of manual rework on the provider side.
Any errors contained in the prior authorization form, from egregious to innocuous, may flag it for denial. A number on a patients health ID card may be transposed. A middle initial may be incorrectly input. An address may be incomplete.
Errors often arise because the prior authorization process can be overly complicated and often involve a lot of manual steps and stakeholders, which can make it ripe for mistakes. Information about the patient, the ordering provider, the requested service, and the medical scenario are required and if any of it is amiss, it will precipitate a denial. Once a denial has been rendered, it is difficult to reverse.
Even when there are no errors, lengthy medical reviews associated with prior authorization can delay care and introduce uncertainty into the process for both providers and patients. This is especially true when benefit managers are involved.
Automating the end-to-end prior authorization process as early in the revenue cycle as possible reduces the likelihood for errors, lessens the amount of manual work wasted on tedious tasks, and accelerates patient care.
Read: Why Automation is the Key to Fixing Prior Authorization
You May Like: Does Medicare Pay For Ct Scans
Medicare Requires Prior Authorization For Spine Procedures
Over the strenuous objection of the AANS, the CNS and other health care stakeholders, effective July 1, the Centers for Medicare & Medicaid Services now requires prior authorization for cervical spinal fusion and implanted spinal neurostimulator procedures when performed in the hospital outpatient department. Neurosurgeons may submit the prior authorization request to their Medicare Administrative Contractors by mail, fax, CMS Electronic Submission of Medical Documentation or the MACs portal. The MAC must respond to the prior authorization request within 10 days. However, an expedited response may be granted within two days if the provider makes the case that a delay could jeopardize the beneficiarys life, health or ability to regain maximum function.
More information is available as follows:
- for the program overview
- for detailed guidance from CMS
- for answers to frequently asked questions and
- to find your MAC for additional details about the new requirements.
Medicare And Prior Authorization
Have you ever needed a medical procedure or service, but your doctor required prior authorization from your insurance carrier beforehand? A prior authorization, also known as a pre-authorization, is a requirement your doctor needs from Medicare or your Medicare Advantage plan before they can perform a service.
Medicare only covers medically necessary services. With that in mind, your doctor will want to make certain he/she will get paid before they perform this service for you. So, how does this affect you? Here is what you need to know about Medicare and prior authorizations.
Also Check: What’s The Difference Between Medicare And Medicaid
The Daily Journal Of The United States Government
Legal Status
This site displays a prototype of a Web 2.0 version of the daily Federal Register. It is not an official legal edition of the Federal Register, and does not replace the official print version or the official electronic version on GPOs govinfo.gov.
The documents posted on this site are XML renditions of published Federal Register documents. Each document posted on the site includes a link to the corresponding official PDF file on govinfo.gov. This prototype edition of the daily Federal Register on FederalRegister.gov will remain an unofficial informational resource until the Administrative Committee of the Federal Register issues a regulation granting it official legal status. For complete information about, and access to, our official publications and services, go to About the Federal Register on NARA’s archives.gov.
Legal Status
Medicare Prior Authorization Explained
Home / FAQs / General Medicare / Medicare Prior Authorization Explained
Before your doctor can provide specific services, prior authorization from Medicare may be necessary. Depending on your plan type, you might need prior approval to see a specialist.
So, which services and types of plans require prior authorization? Below, well explain what you need to know.
Don’t Miss: Are Synvisc Injections Covered By Medicare
Why Is Prior Authorization Particularly Burdensome For Diagnostics And Genomics Labs
Alternative sites of care like diagnostics and genomics labs dont usually communicate directly with patients. Instead, they are reliant on an originating provider like a hospital or physician practice to refer them business and to communicate with patients on their behalf. This business relationship, where the lab is one step removed from the patient, introduces an additional level of complexity when it comes to prior authorization.
If there is a single mistake in the prior authorization process then the diagnostics or genomics lab is put in the position of having to work through the referring provider as a go-between and to rely on them to resolve any issues with the insurance carrier. Because rendering providers depend on referrals from the originating providers, they know that they can only push the referring hospitals and physicians so hard or risk losing future business.
For a deeper dive on this subject, read: Diagnostics Lab Execs Reveal Their Biggest Revenue Cycle Challenges
Why Is Prior Authorization So Complex
The prior authorization process is often complicated by a combination of factors, including:
- Lots of required steps, each introducing the potential for delays and errors.
- Participation by both payers and providers, each of whom have different motivations, workflows, and infrastructure.
- Lack of standards, particularly when it comes to payer rules.
- Fluctuating payer rules which need to be constantly monitored and revised.
- Thousands of payers and health plans.
- Manual review of prior auth requests and medical charts by clinicians.
Don’t Miss: Does Social Security Disability Include Medicare
