Does Medicare Cover Orencia Infusions
Orencia is also a biologic DMARD its available as an infusion or an injection. If you have an infusion, your doctor will administer the drug through a vein in your arm.
Because you obtain infusions outside the home, Part B covers them. If you have a Medigap plan, it will pay the coinsurance costs.
The sticker price for one Orencia infusion is $3,527, but the manufacturer says Medicare patients pay from $0 to $705. If you have Medicare Advantage, your cost will depend on your plan.
If you take Orencia injections at home, the medication falls under Part D. Your benefits will depend on the kind of plan you have. You could pay as much as $1,500 a month. But, Orencias website says more than 80% of Medicare patients pay $25 or less per month.
Sorting Out Insurance Plans And Covered Treatment Options
It is incomprehensible to me why insurance companies make the process so cumbersome and difficult and unpleasant. Add to that the fact that we often shift insurance carriers over the years for various reasons. That adds a whole new level of complication as we try to sort out which plan to get or what medications and treatments are covered. Additionally, we have to START ALL OVER with the approval process for medications!
For Medicare Advantage Plans That Do Not Offer Prescription Drug Coverage And Medicare Advantage Plans That Offer Prescription Drug Coverage
Inflectra and Renflexis, for the indications listed below:
-
Ulcerative Colitis
Are not covered for new starts, unless the member meets ANY of the following:
- Inadequate response to a trial of Avsola, Entyvio, or Remicade
- Intolerable adverse event to Avsola, Entyvio, or Remicade
- Avsola, Entyvio, or Remicade is contraindicated for the member.
Recommended Reading: How Do I Apply For Medicare In Missouri
When Does Medicare Part B Cover Orencia
Generally, Medicare Part B covers the cost of intravenous infusions performed in a doctor’s office, provided that the treatment is deemed medically necessary and the physician participates in Medicare. You will usually have to first pay your deductible to receive coverage. Once your deductible is satisfied, Medicare Part B typically pays for 80% of the cost, leaving you responsible for the remaining 20%. A Medicare Supplement or Medigap plan may help you pay all or some of what you owe
Appendix A: Examples Of Conventional Therapy Options For Cd
Mild to moderate disease induction of remission:
Mild to moderate disease maintenance of remission:
Moderate to severe disease induction of remission:
Moderate to severe disease maintenance of remission:
Perianal and fistulizing disease induction of remission
Metronidazole ± ciprofloxacin, tacrolimus
Perianal and fistulizing disease maintenance of remission
Don’t Miss: What Is The Best Medicare Part D Plan For 2020
Infusions Under The Medical Side Of Medicare
The good news for me, and anyone who uses injectables that are also available by infusion, is that I now can get my medication under the medical side of Medicare, rather than through the RX side, simply by switching to infusions as the medication delivery method. I did not get this information as a routine matter of course from my care team.
Rather, when I spoke to the new rheumatology practice physicians assistant during my first visit, I mentioned my dismay at the fact that my RX for Orencia would cause a serious financial burden for us once we moved to Medicare and the Part D for prescriptions. It turns out it is a tier 3-5 and so it would not be covered by any of the reasonably priced Part D prescription plans we were considering. My monthly premium would go from $15 to nearly $300 plus an over the top deductible!
Ra Costs: What Are Payment Options For Treating Rheumatoid Arthritis
Rheumatoid arthritis is a chronic disease that requires ongoing medication and treatment for the majority of patients. Many of these treatments are highly effective and can stop the diseases progression, preventing further joint damage.
However, specialized medications like disease-modifying antirheumatic drugs and the newer, more expensive biologics can create an affordability concern. This leaves many patients wondering how they will be able to afford their personalized RA treatment over the long-term even if they are covered by health insurance.
Fortunately, there are a number of assistance programs available both privately and through the government to help patients struggling with paying for RA treatment.
Read Also: Does Medicare Require A Referral For A Colonoscopy
Rheumatoid Arthritis Treatment And Medicare Coverage
Home / FAQs / Medicare Coverage / Rheumatoid Arthritis Treatment and Medicare Coverage
Medicare covers a wide range of treatments to slow the progression of rheumatoid arthritis and help with its symptoms. Rheumatoid arthritis treatments can be costly, even with Medicare. If you dont have supplemental coverage, you may pay thousands of dollars. In this context, well discuss which parts of Medicare will cover Rheumatoid Arthritis treatments.
Paying For Rheumatoid Arthritis Treatment
There are many programs and organizations available to help support RA patients in need of financial support. Be sure to speak with your healthcare team about any financial concerns. Your doctor or rheumatologist may be able to suggest programs and offer assistance in order to ensure you get the personalized treatment that you need. Your rheumatologist may also suggest generic brands or other types of drugs that may be just as effective for your particular case which are available at a lower cost to you.
Recommended Reading: What’s The Difference Between Medicare And Medicaid
Criteria For Initial Approval
Aetna considers infliximab , infliximab-abda , infliximab-axxq , and inflixmab-dyyb medically necessary for members with any of the following indications, where the member has had a documented negative tuberculosis test , an interferon-release assay , or a chest x-ray)Footnotes* within 6 months of initiating therapy for persons who are naive to biologic DMARDs or targeted synthetic DMARDs associated with an increased risk of TB:
Moderately to severely active Crohns disease
Moderately to severely active ulcerative colitis
Moderately to severely active rheumatoid arthritis
Member meets either of the following criteria:
What If I Have Medicare Advantage
Medicare Part C is also called Medicare Advantage. Part C plans are sold by private insurance companies, and you can enroll in one as an alternative to original Medicare.
The cost of a Part C plan can vary based on your location.
Part D prescription drug coverage is included in most Part C plans. If you want prescription drug coverage with your Part C plan, youll have to include that coverage when you shop for a plan.
You cant enroll in a separate Part D plan if you have Medicare Advantage.
As with Part D, its important to review a Part C plans formulary to see if the medications you take are listed there. If you have additional questions or concerns, dont hesitate to contact your pharmacy or the plans company directly.
Also Check: What Is Medicare Ffs Program
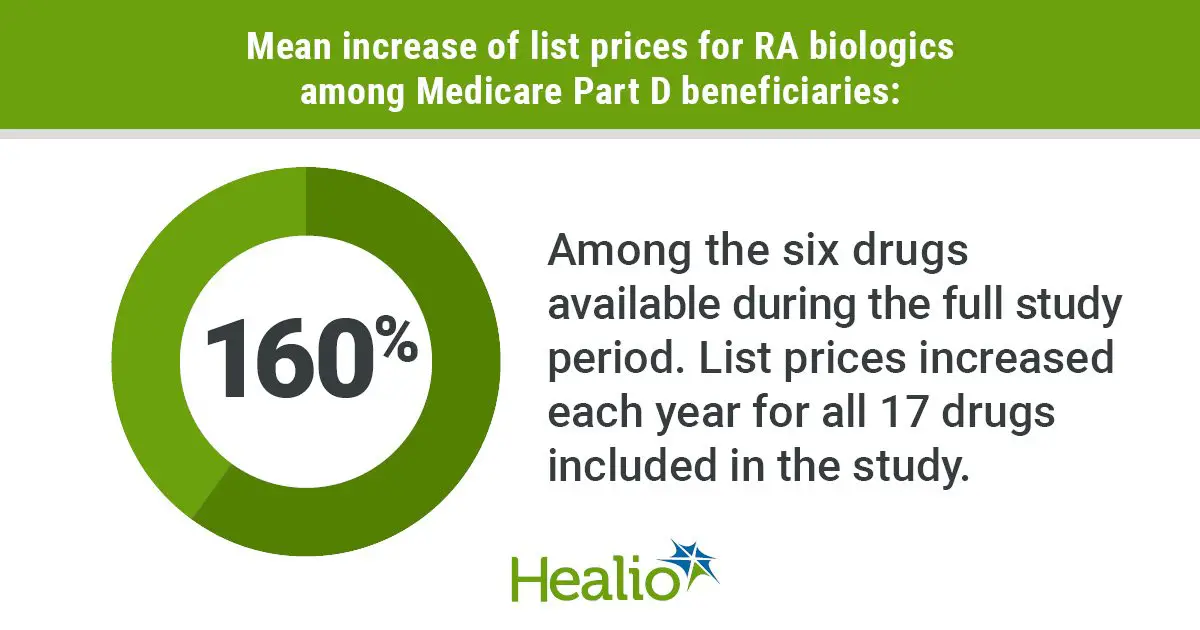
Impact Of Medicare Part D On Access To And Cost Sharing For Specialty Biologic Medications For Beneficiaries With Rheumatoid Arthritis
Polinski JM, Mohr PE, Johnson LArthritis Rheum. 2009 61:745-754
Study Summary
Medicare coverage for biologic therapies — a mainstay of treatment for rheumatoid arthritis — has been in flux recently. Medicare Part B coverage for biologic therapy ended in 2004, and the Medicare Replacement Drug Demonstration program that provided temporary drug insurance until the start of Medicare Part D ended in 2006.
Part D has resulted in a complicated set of options for patients to obtain medication coverage, including various cost-sharing mechanisms. The Medicare Part D plan has the following basic structure, administered by stand-alone providers or by Medicare Advantage plans: initial deductible an initial coverage period a coverage gap interval and catastrophic coverage .
In the stand-alone programs or Medicare Advantage programs, patients may select from various cost-sharing options, including deductibles, monthly premiums, co-insurance, copayments, and coverage limits. There are subsidies for low-income individuals to reduce the costs of the Part D plans. In addition, many Part D plans put biologic therapies in specialty tiering, meaning that the drugs would be subject to higher patient cost sharing.
Viewpoint
Cite this: Kevin Deane. Guiding RA Patients Through Medicare Maze Toward Payment for Biologic Therapies – Medscape – Aug 25, 2009.
Tables
What Does Enbrel Do

Rheumatoid arthritis occurs when your immune system begins to attack your joints, giving rise to inflammation. A protein called tumor necrosis factor drives the process. Enbrel is a type of injectable drug known as a biologic agent or biologic. It works by attaching to TNF proteins, preventing them from acting on the joints. Typically, doctors prescribe one 50-gram injection of the drug per week for the treatment of RA.
Read Also: Are Doctors Required To Accept Medicare
What Tier Is Orencia
Medicare Part D plans establish drug tiers that determine how much you pay out of pocket for your medications. Orencia usually falls under Tiers 3 or 4, which correspond with brand name medications. Tier 3 is the drug your plan specifies as the preferred treatment. Generally, your share of the cost is less with Tier 3 than Tier 4 drugs.
Physical And Occupational Therapy
You may be referred to a physical therapist to help you learn exercises to maintain joint flexibility and range of motion. Your physical therapist may also recommend assistive devices such as walkers or canes to help with mobility, or braces and arthritis gloves to protect tender, swollen joints. An occupational therapist can assist you with adaptive devices to help you perform daily living activities such as dressing and preparing and eating meals.
You May Like: When Are You Eligible For Medicare Part A
Appendix E: Ra Classification And Disease Activity
RA Classification
Rheumatoid arthritis classification criteria include a scoring system for the following four domains: joint distribution , serology , symptom duration , and acute phase reactants . A score of 6 or more equals definite RA however, a person might fulfill the criteria prospectively over time , or retrospectively if data on all four domains have been adequately recorded in the past. The criteria are meant to be used for persons with clinical synovitis in at least one joint. The classification are not diagnostic criteria, but they can inform the diagnosis. For more information see, American College of Rheumatology – Endorsed Criteria.Source: 2010 ACR/EULAR
Disease Activity
Disease activity is categorized as low, moderate, or high as per validated scales. Moderate and high disease activity categories have been combined . Structured assessments of disease activity which include multiple composite measures have been developed for RA. Eleven measures have been identified by the American College of Rheumatology as having utility in clinical practice to accurately reflect disease activity. The choice of measure is based upon clinician preference some measures require both patient and clinician input, while others are based only upon patient-reported data .
Medicare A Supplemental Plan And A Part D Prescription Plan
I knew in October that I would be starting Medicare and picking up a Supplemental Plan and a new Part D prescription plan in January so I started the process of getting my rheumatologist on board with the changes we needed to make. As it turns out, there were many complications along the way, human error and just incompetence. All of which made the transition chaotic and scary because I was on the verge of running out of my medication.
Don’t Miss: Is Medicare Part D Necessary
Medicare Advantage Plans Can Cover Rheumatoid Arthritis Treatments
The CHRONIC Care Act of 2018 expanded coverage for Medicare beneficiaries with chronic conditions such as rheumatoid arthritis. The bill granted greater flexibility for Medicare Advantage plans to cover non-medical benefits going forward.
Thanks to the bill, Medicare Advantage plans may now cover additional services and items related to home care that can be of use to someone with rheumatoid arthritis.
These can include, but arent limited to:
- Caregiving services for custodial care
- Home-delivered meal services
- SilverSneakers gym memberships
There also may be Medicare Special Needs Plans specifically for beneficiaries suffering from rheumatoid arthritis. A Special Needs Plan is a type of Medicare Advantage plan that features benefits designed especially for people with a certain condition.
Appendix B: Examples Of Conventional Therapy Options For Uc
Mild to moderate disease induction of remission:
Mild to moderate disease maintenance of remission:
Severe disease induction of remission:
Severe disease maintenance of remission:
You May Like: Does Medicare Part A Cover Doctors In Hospital
What If You Can’t Pay
If your doctor prescribes a biologic to treat your RA and your insurance covers it, your portion of the payment can still sometimes run hundreds of dollars per month.
If you can’t afford that, there are still ways to get the medications your doctor recommends:
Patient assistance plans: Most, if not all, companies that make biologics offer plans to help people who can’t afford them. These programs may cover copayments or, in some cases, offer the drugs at a discount or for free. To find out if the drug company that makes your biologic offers assistance, talk with your doctor or check the company’s website.
State programs: Some states offer help to older and disabled people without drug coverage. To learn more about what your state offers, visit the Medicare website and search “prescription drug assistance.”
Private foundations: Some organizations help folks with low and moderate incomes afford their medicines. If you risk going without drugs you need, your doctor may know an organization that can help. So donât be afraid to ask. NeedyMeds has information on more than 2,400 drug assistance programs. The Partnership for Prescription Assistance and Rx Assist also can point you in the right direction.
Pharmacy discount programs: Some pharmacies have discount programs. Ask yours what it offers.
Sticking To Your Treatment Plan

A 2018 report in the journal Arthritis & Therapy found that 50% to 70% of people with RA were nonadherent with their recommended treatment plans. Nonadherence to treatment is one of the main reasons RA treatments fail.
Your rheumatologist has prescribed biologic drug therapy because they believe that the benefits outweigh the risks. The good news is that many of the newer biologic drugs are safe and effective.
If you feel you need to stop your biologic drug because of side effects, cost, or another reason, talk to your rheumatologist first. The decision to stop, change, or reduce the dosing of a drug should be made by you and your doctor, and not one you make alone.
Also Check: Is Rocklatan Covered By Medicare
Biologics For Ra: Costs And Insurance
Biologic drugs for rheumatoid arthritis work for 2 out of 3 people who take them for RA. These genetically engineered drugs often slow or halt the progression of joint damage, and they may even push RA into remission. But the drugs are expensive they cost about $1,000 to $3,000 a month. Even with health insurance, your out-of-pocket costs can add up to hundreds or thousands of dollars.
Hereâs what you need to know about paying for biologics if your doctor wants to add one to your RA treatment plan.
Clinical Characteristics And Demographics
In total, 3 156 628 Medicare beneficiaries were identified in the study period . Of these, 2 924 894 were excluded because they were aged < 65 years, had no continuous health enrolment plan or had no diagnosis of RA during the study period, resulting in a total sample size of 231 734 patients . Mean patient age was 75.2 years 79.4% were women 86.4% were Caucasian and 41.3% resided in the Southern region of the US .
Patient attrition scheme
You May Like: Does Medicare Pay For Stem Cell Treatment
Are There Assistance Programs For Enbrel
Amgen provides a copay card and an assistance program for Enbrel however, these offers aren’t available for people on Medicare. Your state’s Pharmaceutical Assistance programs may be able to help you pay for Enbrel if your Medicare plan doesn’t cover the drug or you can’t afford your copays or coinsurance.
Insured Read Your Policys Fine Print
When the time comes around for open enrollment, look at your insurance contract for how it treats copays. If you see something unfavorable, consider switching. Weve had concerns that insurance companies have hidden copay accumulator programs in the fine print when people re-sign their annual contracts, says Newmark, referring to the practice of applying manufacturers coupons toward the deductible. As a result, patients are caught by surprise that they havent met their deductible and their budget is impacted by unanticipated payments, which could be thousands of dollars spending on the structure of their health plan. Transparency and fairness is needed to protect patients from predatory payer policies.
You may have some measure of protection against this practice if you live in one of four states that Newmark says passed bills last year to curb this practice: Arizona, Illinois, Virginia, and West Virginia.
Also Check: Does Medicare Cover Bed Rails
