Does Medicare Cover Counseling
- Activity therapies like art, dance, and music therapy
- Family counseling to address a mental health condition
- Drugs that usually arent self-administered
- An annual depression screening with a primary care physician
- An annual alcohol misuse screening with a primary care physician
Medicare Part B has an annual deductible that changes over time. It was $183 in 2018 and is $233 in 2022. After the deductible, Medicare covers 80% of outpatient services and you have to pay 20% coinsurance on the Medicare-approved amount for the service you are receiving.
The standard monthly premium for Medicare Part B in 2022 is $170.10. This amount is usually deducted from your Social Security check.
Qualified Registries For Mips Data Submission
Under the Medicare Quality Payment Program option, MIPS, there are several data submission methods, one of which is Qualified Registries. A qualified registry is a CMS-approved entity that collects clinical data from MIPS eligible clinicians and submits it to CMS on their behalf for purposes of MIPS. CMS has designated the qualified registries that can report data for the Quality, Advancing Care Information, and Improvement Activities performance categories, on behalf of individual MIPS eligible clinicians and groups. The APAs PsychPRO registry is approved by CMS.
Cpt Coding For Therapy
CPT coding for psychotherapy doesnt have to be difficult! There are an overwhelming amount of total CPT Codes , however only 24 are specifically designated for psychotherapy and other mental health services.
To make matters even simpler, nearly all therapists will regularly use an even smaller subset of these 24.
CPT is a large and dynamic code set that changes year to year, but the psychotherapy codes seldom change.
The most recent change for psychotherapy codes took place in 2019, then 2013, and previously 1998.
To ensure your coding is current and up to date, consider using a billing service instead of having to remember all the codes.
Don’t Miss: What’s The Number For Medicare
Psychiatry And Psychotherapy Documentation
Proper payment and sufficient documentation go hand in hand. CMS has created a video series to help providers improve in areas identified with a high degree of noncompliance. The CMS Provider Minute: Psychiatry and Psychotherapy video includes pointers to properly submit documentation for these services. In about three minutes, the video explains:
- Use of add-on codes when billing for same day evaluation and management and psychotherapy services
- Three factors needed for sufficient documentation
Looking Forward: Research Priorities
Rigorous analysis of how the policy recommendations above influence care delivery, consumer outcomes, and costs will be necessary. Future research should include evaluations of implementation strategies to support uptake of systematic depression screening and behavioral health integration activities like care management, as well as studies of strategies to improve mental and physical health outcomes for beneficiaries enrolled in primary care medical homes and accountable care organizations. Additional research is needed on models for delivering psychosocial services, like supportive employment, for Medicare beneficiaries with serious mental illness one potential option could be to incentivize additional mental-illness-focused Special Needs Plans.
Finally, further investigation is needed to identify telehealth policies most likely to increase access to mental health services and improve consumer outcomes. This line of research should explore consumer preferences for telemental health services versus in-person treatment.
Read Also: When Are You Eligible For Medicare Part A
Proposed Legislation Allows Lmft And Lmhc To Bill Medicare
The US Congress is currently considering two bills, S. 1879 and H.R. 3032, entitled the Mental Health Access Improvement Act of 2017, which amend title XVIII of the Social Security Act.
The Proposed Changes
The two bills, which both must pass, amend the language in the current legislation of the Social Security Act to cover marriage and family therapist services and mental health counselor services under Medicare Part B. The updated language that includes LMFTs and LMHCs must pass in both the House and the Senate in order to become law.
Currently, the covered mental health professionals recognized by Medicare include psychiatrists, psychologists, mental health clinical nurse specialists, and clinical social workers.
Marriage and Family Therapists and Mental Health Counselors are not listed as Medicare-covered providers despite the fact that these mental health professionals have education, training, and practice rights similar to other covered providers.
This legislation, if passed, will give greater access to mental health services to elderly and disabled persons on Medicare, and provide a significant increase in potential revenue for LMFTs and LMHCs currently unable to bill Medicare.
Qualifications Under the New Bill
What You Can Do
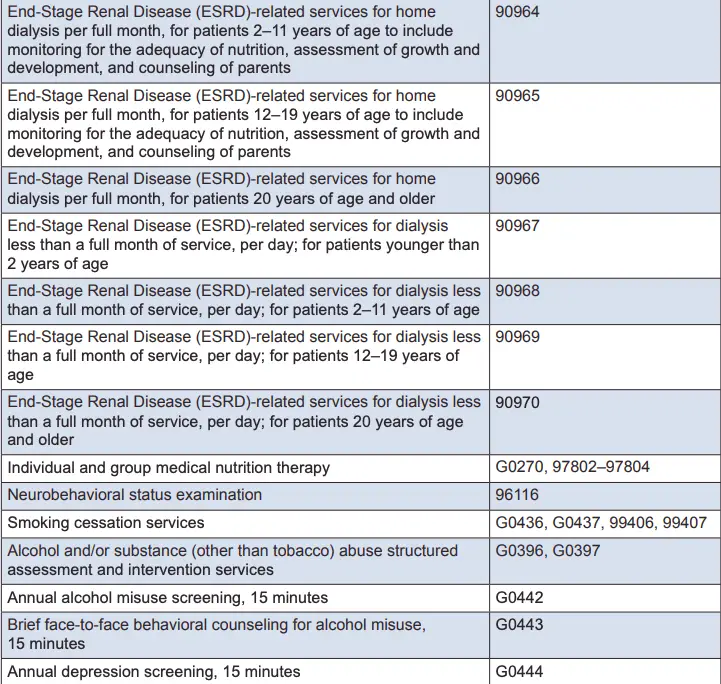
Other Behavioral Health Cpt Codes:
- +90785 Interactive Complexity add-on code. Covered below.
- 90404 Cigna / MHN EAP CPT Code. These two companies use a unique CPT code for EAP sessions.
- 96101 Psychological testing, interpretation and reporting by a psychologist
- 90880 Hypnotherapy limit 10 units/hours per application
- 90876 Biofeedback
- 90845 Psychoanalysis
Also Check: Which Medicare Supplement Plan Covers The Most
Mental Health Cpt Codes: The Definitive Guide
CPT is a standardized medical codeset maintained by the AMA. CPT codes are five digit numeric codes describing everything from surgery to radiology to psychotherapy.
CPT Codes are different from Diagnosis Codes or ICD10 F-Codes for billing and coding your insurance claims. Heres our mental health diagnosis code list if you need to look one up.
For therapists that are on managed care panels or provide superbills to their clients, knowing your CPT codes is paramount to getting paid in full and avoiding insurance audits.
The amount insurance companies will reimburse depends on a number of different factors , but using the correct CPT Code and add-on code to express the exact service is an important part to the whole process and in ultimately determining your payment!
Errors, accidental or otherwise, will directly impact insurance companys payment of services. If you need help with making sure your billing and coding is error-free, our mental health billing service can help.
Think about reaching out if the rest of this article hurts your feelings.
Medicare Mental Health Coverage
CMS is proposing to extend key flexibilities in place during the PHE for 151 days after the public health emergency ends, such as allowing telehealth services to be furnished in any geographic area and any originating site setting, including the beneficiarys home, and allowing certain services to be furnished via audio-only telecommunications systems. They also propose delaying the in-person visit requirements for mental health services furnished via telehealth until 152 days after the end of the PHE.
- CMS is proposing that telehealth claims will require the appropriate place of service indicator to be included on the claim, rather than modifier 95, after 151 days following the end of the PHE
- They propose that the modifier 93 be used to indicate that a Medicare telehealth service was furnished via audio-only technology, where appropriate.
- Please note that CMS is proposing these changes. They have not yet been approved.
Also Check: What Is Medicare Part B Monthly Premium
Tips For Mental Health Billing
When learning how to bill for therapy services, there is always room for improvement and efficiency. Some elements can speed up insurance billing and ensure a reduction in errors benefitting mental health providers and patients alike. Consider these mental health billing tips that can help make the process smoother.
Macra Assistance From The Apa
The Medicare Access & CHIP Reauthorization Act completely transforms Medicare payment and quality reporting, though the Merit-Based Incentive Payment System and new incentives for advanced alternative payment models . To help members understand the new regulations, APA has relaunched its Payment Reform webpage and prepared free educational materials and a webinar series. Download the MACRA 101 Primer For Psychiatrists. The recorded presentation Quality Reporting 101: A How-to Guide for Psychiatrists is available through the APA Learning Center.
The APA Practice Management Helpline at 1-800-343-4671 is available for coding, reimbursement and practice management questions.
Also Check: What Medicare Supplement Plans Are Available
Does Medicare Cover Marriage Counseling
Medicare generally only covers marriage or couples counseling in a very limited number of cases.
First, Medicare has only been reimbursing marriage and family therapists since 2019, and it currently only reimburses them for services provided to people with a primary substance use disorder diagnosis.
Second, Medicare only covers services linked to a primary psychiatric diagnosis listed in the Diagnostic and Statistical Manual of Mental Disorders . So, it wont cover any kind of marriage or family therapy from any kind of provider if it isnt required to treat a mental health condition.
This means that if you want to see a social worker or psychologist to address communication or other relationship issues that arent directly related to a mental health diagnosis, Medicare wont cover it.
Gaps In Medicare Mental Health Coverage
Inpatient day limits. Medicare beneficiaries are limited to 190 days of inpatient psychiatric hospital care in their lifetime, a much stricter limit than the 90-day-per-benefit-period limit on general medical hospitalizations. People with chronic mental illness, particularly younger beneficiaries who qualify for Medicare because of a disability, may exceed this limit and may be subject to high out-of-pocket costs for needed inpatient care. This is predominantly an issue for beneficiaries who are not dually eligible for Medicaid: state Medicaid programs pay for inpatient psychiatric services for most dual-eligible beneficiaries who have exceeded Medicares 190-day limit. The Congressional Budget Office estimated that eliminating the Medicare 190-limit would increase federal spending by $3 billion over 10 years.23
Medicare mental health provider payment issues.
Read Also: Does Medicare Plan F Cover International Travel
Do Mental Health And Substance Use Disorder Parity Laws Apply To Medicare
Prior to 2010, Medicare beneficiaries paid a higher coinsurance rate for outpatient mental health services than for other outpatient services covered under Part B . The Medicare Improvements for Patients and Providers Act of 2008 phased in parity for cost sharing for all outpatient services covered under Part B between 2010 and 2014, so that as of 2014, cost sharing for outpatient mental health services is the same as for other Part B services.
Federal parity laws, including the Mental Health Parity Act of 1996 and the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 , do not apply to Medicare, however. The Mental Health Parity Act of 1996 requires parity in annual and aggregate lifetime dollar limits for mental health benefits and medical or surgical benefits in large groups plans, but not Medicare. The Mental Health Parity and Addiction Equity Act of 2008 , which expanded on the 1996 law, extends parity to substance use disorder treatments, and prevents certain health plans from making mental health and substance use disorder coverage more restrictive than medical or surgical benefits, also does not apply to Medicare. In 2016, some of these parity rules were applied to Medicaid Managed Care Organizations but not to Medicare benefits that are provided by Medicaid MCOs to beneficiaries dually enrolled in Medicare and Medicaid.
Which Outpatient Mental Health Care Services Does Medicare Cover
Medicare covers the following outpatient mental health care services:1
- Annual depression screening
- Family counseling, when the goal is to help with treatment
- Psychiatric evaluation and diagnostic tests
- Outpatient treatment programs
- Medication management and certain medications that are not self-administered, like some injections
- For treatment of drug or alcohol abuse
- Partial hospitalization
Read Also: Is Belsomra Covered By Medicare
Faqs On Mental Health And Substance Use Disorder Coverage In Medicare
The COVID-19 pandemic has taken a heavy physical and mental health toll on all ages, including older adults, heightening interest in strategies to improve access to mental health and substance use disorder services generally, and in Medicare. In April 2022 more than two years into the pandemic one in six adults 65 and older reported anxiety and depression, according to KFF analysis of the Household Pulse Survey, somewhat lower than the quarter of older adults who reported anxiety and depression in August 2020, when the country was in still the midst of widespread lockdowns in the early stage of the pandemic. Additionally, nearly a third of adults 65 and older say that worry or stress related to coronavirus has had a negative impact on their mental health, according to KFF polling,a somewhat lower rate than reported among younger adults.
These FAQs review mental health and substance use disorder coverage and out-of-pocket costs in Medicare and discuss policy proposals related to coverage of mental health and substance use disorder treatments.
Increased Roles For Psychologists Social Workers & Psychiatrists
Additionally, CMS proposes Medicare mental health coverage for clinical psychologists and licensed clinical social workers to provide integrated behavioral health services as part of a patients primary care team. CMS has proposed the creation of a new General Behavioral Health Integration Services delivered by clinical psychologists or clinical social workers . The new service would be responsible for monthly care integration where the mental health services furnished by a CP or CSW serve to focus the care integration.The new CMS proposal includes a psychiatric diagnostic evaluation as the initial visit for the new general BHI service. See TBHIs article for specifics: Practice Alert: Proposed CMS Reimbursement for LMFTs, LPCs, Addiction Counselors, Psychologists, Social Workers & Others.
You May Like: Is Medicare Running Out Of Money
Medicare Outpatient Mental Health Services
Medicare Part B covers outpatient mental health services, such as care youd get in a health clinic or doctors office. Youll generally pay 20% of the Medicare-approved cost for outpatient care delivered by providers that accept Medicare assignment.
Medicare covers the following types of psychotherapy :
- Psychiatric assessment
- Family counseling, when the primary goal is to treat your condition
- Alcohol misuse counseling, up to four sessions
You may need to meet other criteria to be eligible for therapy coverage, and the doctor, psychologist, or other health-care professional must accept Medicare assignment. Medicare doesnt cover certain types of therapy, such as pastoral counseling or marriage counseling.
If you need more structured or frequent treatment, Medicare Part B also covers partial hospitalization programs, which are outpatient mental health programs where treatment is provided throughout the day and doesnt require an overnight, inpatient stay. The programs are usually run through a community mental health center or a hospitals outpatient department. Services may include therapy with a mental health professional, diagnostic services, and occupational therapy . These programs dont cover meals or transportation to the facility.
Small Practices And Health Professional Shortage Areas & Medically Underserved Populations
CMS launched a new section of the Medicare Quality Payment Program dedicated to clinicians working in small or rural practices as well as those treating patients in underserved areas. This page is a single point of reference for the QPP, especially, for those participating under the Merit-based Incentive Payment System track. Quickly locate contact information for organizations that assist practices through the Small, Underserved, and Rural Support initiative using an interactive map. Review the flexibilities to help reduce the participation and reporting burden on small practices for 2017. More features and information will be added, so submit your feedback to CMS.
MACRA provides direct technical assistance for small practices to participate in the QPP through an organization called IPRO, which serves Maryland, DC and Virginia.
Health Professional Shortage Areas are designated as having shortages of primary care, dental care, or mental health providers and may be geographic , population or facilities . Providers who serve these areas are eligible for bonus payments under Medicare. A search tool is available to check an address for bonus eligibility. Use another online tool to find HPSAs by state, country and discipline.
You May Like: How Do I Contact Medicare Cms
User License Agreement And Consent To Monitoring
End User Agreements for Providers
Some of the Provider information contained on the Noridian Medicare web site is copyrighted by the American Medical Association, the American Dental Association, and/or the American Hospital Association. This includes items such as CPT codes, CDT codes, ICD-10 and other UB-04 codes.
Before you can enter the Noridian Medicare site, please read and accept an agreement to abide by the copyright rules regarding the information you find within this site. If you choose not to accept the agreement, you will return to the Noridian Medicare home page.
THE LICENSES GRANTED HEREIN ARE EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THESE AGREEMENTS. BY CLICKING ABOVE ON THE LINK LABELED “I Accept”, YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THESE AGREEMENTS.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK ABOVE ON THE LINK LABELED “I Do Not Accept” AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THESE AGREEMENTS CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, “YOU” AND “YOUR” REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
LICENSE FOR USE OF “PHYSICIANS’ CURRENT PROCEDURAL TERMINOLOGY”, FOURTH EDITION
Consent to Monitoring
How Much Do Medicare Beneficiaries Pay For Mental Health Benefits And Substance Use Disorder Benefits
Inpatient Services
Beneficiaries who are admitted to a hospital for inpatient mental health treatment would be subject to the Medicare Part A deductible of $1,556 per benefit period in 2022. Part A also requires daily copayments for extended inpatient hospital stays. For extended hospital stays, beneficiaries would pay a $389 copayment per day and $778 per day for lifetime reserve days. For inpatient stays in a psychiatric hospital, Medicare coverage is limited to up to 190 days of hospital services in a lifetime. Most beneficiaries in traditional Medicare have supplemental insurance that may pay some or all of the cost sharing for covered Part A and B services.
Outpatient Services
For most outpatient services covered under Part B, there is a $233 deductible and 20 percent coinsurance that applies to most services, including physician visits. However, some specific Part B services have different cost-sharing amounts :
Prescription Drugs
Those with Part D coverage face cost-sharing amounts for covered drugs and may pay an annual deductible and a monthly premium. For example, most Part D enrollees pay less than $10 for generic drugs, but many pay $40-$100 for brand-name drugs. Beneficiaries with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing.
You May Like: How To Check My Medicare Coverage
