I What You Should Know About In
When people say in-home care, there are several different types of care to which they could be referring. This range of options is one of the appealing things about home care, as it can be customized to meet each individuals needs. In-home care can range from tasks as basic as providing companionship during the day to as involved as round-the-clock medical monitoring.
To help you better understand the different types of in-home care and how they differ from one another, weve broken the varieties of in-home care into three categories below.
What Are Medicare Medicaid And Obamacare
There are four typical ways that many Americans receive health insurance today:
- A group health plan sponsored by an employer
- Private insurance purchased through the
- Medicare, which is a federally-funded health insurance program for adults over age 65 and some younger people with certain disabilities and medical conditions
- Medicaid, which is a government health insurance program for people who have limited financial resources
Recommended Reading: How Much Is Premium For Medicare
Home Health Care Services Covered By Medicare
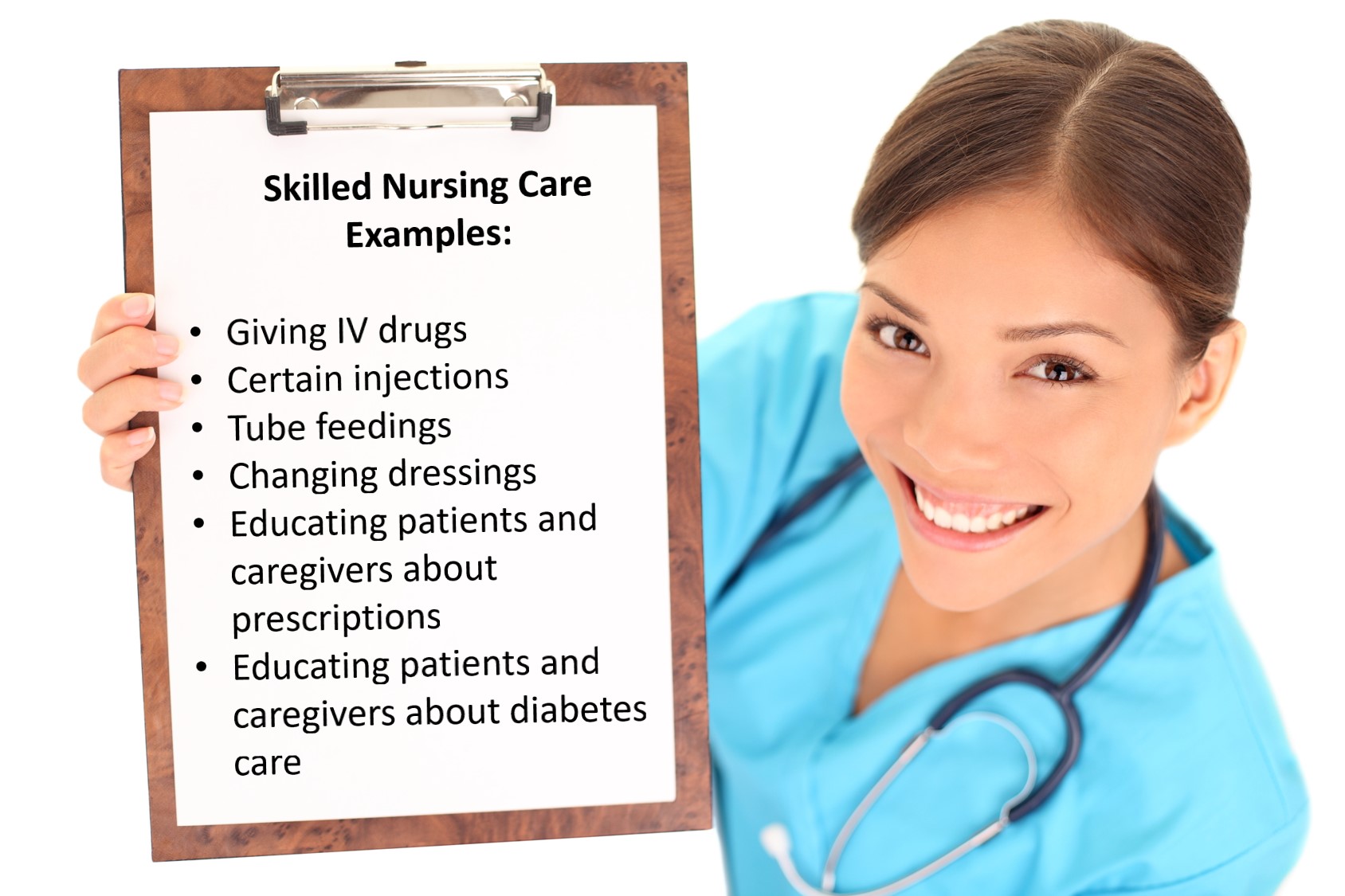
As opposed to standard in-home care, home health care is considered skilled nursing care and thus is covered by Medicare. A range of home care services falls under the benefit. Some of the covered home health care services include:
- Skilled Nursing Care: This includes all care services that must be carried out by registered or licensed nurses, such as medication administration and monitoring of your vital signs. Medicare only covers intermittent nursing services, which means part-time. There are time limits on how many hours per week and/or days per month of care that Medicare will cover.
- Therapy Services: Often needed when recovering from an illness or injury, this includesrehabilitation services such as physical and occupational therapy and speech-language pathology.
- Medical Social Services: Medical social services involve counseling to help seniors deal with the emotional and social impact of their illness or injury.
- Medical Supplies: Any medical supplies related to the condition for which youre being treated, such as catheters and wound dressings, are covered by Medicare. Durable medical equipment like wheelchairs may be partially covered.
Its important to note that even when the above criteria are met, Medicare never covers full-time home health care. If you need around-the-clock care and cannot financially support full-time, in-home health care without Medicare, a skilled nursing community may be a better option.
Also Check: Will Medicare Part B Pay For Shingrix
Home Health Research And Demonstration Initiatives
Central to efforts to redesign the home health benefit is an understanding of home health users’ needs, preferences, and resources, and how these change over time. Payment, QA, and service delivery changes need to reflect and be responsive to these needs. To increase HCFA’s understanding of these issues, research and demonstrations focus on the following:
For example, HCFA is sponsoring several research and demonstration initiatives in home health care payment reform, including prospective payment, bundling post-acute-care services , and capitation payments.
Prospective payment is being tested on a per visit and per episode basis. As described in greater detail in this issue , impact analyses from the first year of per visit prospective payment indicate that this payment methodology has not affected agencies’ cost per visit, revenues or profits, or quality of care. Under a per episode prospective payment , providers will have greater opportunity to alter the way they provide services by changing the way in which they deliver a series of visits during the course of an episode and by changing the way in which they provide specific visits. Per episode payment may also more appropriately support a focus on patient outcomes.
- Improve functional outcomes and increase independent living.
- Increase efficiency of care.
- Increase appropriate use of post-acute-care services, defined by outcomes .
Status Of The Initiative
To date, three meetings have been held with consumer, provider, research, and State Medicaid agency representatives to explore quality assurance, administrative, and operational issues in greater detail. Physicians’ and other professionals’ roles in home health care and care plan oversight have emerged as central issues during the course of these meetings, culminating in a planned symposium to address these issues in a more focused way. Smaller groups have been convened to provide technical expertise in areas such as the development of a comprehensive assessment instrument. Work has also begun on revising HHA Conditions of Participation and in developing a multi-focused strategy to improve communication regarding the home health benefit. Demonstrations in outcome-based quality assurance and per-episode prospective payment are scheduled for Fall 1994. Discussion sessions with consumer, provider, and research communities on payment issues are also scheduled.
Recommended Reading: When Do You Stop Paying For Medicare
Medicare Payment System And Other Policies Create Obstacles To Care
Misunderstanding about the scope and duration of services available under the home health benefit is driven and reinforced by Medicare payment policies. For example, the most recent Medicare payment model, effective in 2020, called the Patient-Driven Groupings Model , changed home health agencies financial incentives and disincentives to admit or continue care for Medicare beneficiaries. For instance, under the PDGM, payments are higher for beneficiaries who are admitted after an inpatient stay and lower for those admitted from home. Further, the PDGMs financial incentives include higher payment rates for the first 30 days of home care and declining payments after the first 60 days.
Similarly, the Home Health Value-Based Purchasing Model, which will be expanded nationwide in 2023, increases or decreases payment to home health agencies based on their performance on measures intended to promote higher-quality care. In practice, however, this payment model rewards health improvement and may incentivize providers to avoid serving people with ongoing, debilitating, and chronic conditions who benefit from services but may not improve or improve quickly.
Health Insurance Open Enrollment: If You Need Health Insurance Coverage In Michigan Help Is Here
This site contains everything you need to know about health insurance, how to get covered, and how to use your coverage to keep yourself and your family healthy.
Open Enrollment for 2023 health insurance runs from November 1, 2022 through January 15, 2023. Consumers must select a plan no later than December 15, 2022 for coverage to start on January 1, 2023.
Open Enrollment gives Michiganders the chance to take advantage of newly extended tax subsidies that can help make insurance more affordable. During 2022, approximately 85% of enrolled Michiganders qualified for a subsidy, with many finding a plan for less than $10 per month.
Consumers who still need health insurance for 2022 may qualify for a Special Enrollment Period if they experience a qualifying life event, such as a birth, job loss, or divorce. In addition, Michiganders who qualify for the states Medicaid or MIChild programs can apply at any time. For help getting started, and to review their eligibility for these programs, consumers should visit Healthcare.gov/lower-costs.
Your local agent or assister can help with the application or answer your questions. Find Marketplace help near you by visiting LocalHelp.HealthCare.gov.
Dont Miss: Does Medicare Cover Synvisc Shots
You May Like: Is There A Copay With Medicare Part D
Does Medicare Cover Home Health Care
Medicare Parts A and B cover home health care if the services needed are considered reasonable and necessary for the persons specific illness or injury, says Ari Parker, co-founder and head advisor at Chapter, an independent Medicare advisor organization. Furthermore, you must be under the care of a doctor who declares you homebound to qualify for home health care under Medicare.
Medicare covers skilled nursing care, physical therapy, occupational therapy and speech-language pathology services. In addition, Medicare covers home health aide services and Medicare social services, which is when a doctor may recommend counseling to help with social and emotional concerns that could hinder the recovery process, adds Parker.
While Medicare covers part-time or intermittent skilled nursing, physical and occupational therapy and other qualified services in the home, it becomes less beneficial when the level of home health care shifts toward custodial or constant care.
Medicare will not cover 24-hour-a-day care, delivery of meals or home care services, such as cleaning, laundry or support with activities of daily living , such as bathing, toileting or dressing, says Chris Orestis, Certified Senior Advisor and president of Retirement Genius, a website dedicated to helping seniors navigate retirement.
How Do I Find Medicare
Medicare.gov has a search and comparison tool to help you find certified home health agencies in your area that Medicare covers.
If you have coverage from a private Medicare Advantage plan, rather than original Medicare, you may have to use an agency that works with that Advantage plan. Talk with a Medicare Advantage plan representative about coverage details and requirements.
Before you start receiving care, the agency should let you know, both verbally and in writing, of services provided that Medicare wont cover and what you can expect to pay for them.
Keep in mind
You may be able to get additional caregiving support through local and state programs, which may provide services such as adult day care programs, equipment, meal delivery, respite care for caregivers and transportation. You can find out more about programs in your area through your Area Agency on Aging. Type your zip code or city and state into the U.S. Administration on Agings Eldercare Locator or call 800-677-1116, to find contact information for your local agency and other resources.
You May Like: How Many Parts Medicare Has
Which Medicare Parts And Plans Cover Home Health Care
If youre enrolled in Original Medicare, you will use both Part A and Part B to cover limited home health services, says Parker.
Some Medicare Advantage plans also offer additional benefits, such as caregiver support services or home modifications. However, the benefits offered for home health care vary widely from plan to plan, so its important to understand the coverage offered before you sign up for a Medicare Advantage plan, adds Parker.
Does Medicare Cover Occupational Therapy At Home
Occupational therapy in a patients own home or residence is generally covered by original Medicare, Parts A, and B.
Occupational therapy helps patients navigate through sensory, cognitive, and physical problems. An occupational therapist may help patients refine their motor skills by working on keenness and concentration through picking items with tweezers. They also guide their patients through normal daily activities like dressing up or cooking.
Read Also: Does Medicare Cover Dental Root Canals
Can I Choose Marketplace Coverage Instead Of Medicare
Generally, no. You can choose Marketplace coverage instead of Medicare if you have to pay a Part A premium. Before making this decision, check if Marketplace coverage meets your needs and fits your budget. Also consider:
- If you dont sign up for Medicare when youre first eligible , you might have to wait to sign up. You might also have to pay monthly late enrollment penalties.
Also Check: Is Medicare Free In Usa
Pros And Cons Of Home Health Care
The benefits of properly administered home health care can be enormous. The fact that Medicare will pay for an unlimited number of home health care visits with no copayments makes home care a very good financial value compared to recovery in a hospital or nursing facilityin addition to the recuperative benefits of being at home.
Being in your own home or even that of a friend or relative is often more conducive to a speedy recovery than the impersonal and sometimes frightening environment of a hospital. You have familiar things around you, your friends and family can come and go without worrying about “visiting hours,” and they can lend a hand with your care. You have greater privacy and are free from dreadful hospital routines and late-night noise and lights.
On the other hand, home health care is not always the best solution. Hospitals sometimes push people out the door before they are well or strong enough, and as a result the people may take longer to recover at home, or suffer more pain and discomfort at home, than they would have if they had remained in the hospital just a few days more. This is particularly true when a patient does not have family or friends available to supplement the care provided by a home care agency.
Also Check: How To Qualify For Medicare In Ohio
What Is The Eligibility For Medicare Advantage Plans
Most people arent eligible for supplemental Medicare plans, or Medicare Part C, unless theyve already been approved for traditional Medicare. Also, applicants must be under the care of a physician and receive services that are regularly reviewed by the doctor. Those applying for supplemental Medicare must also be receiving physical or occupational therapy and be certified as homebound.
Eligibility for a Medicare Advantage Plan depends on the requirements for each plan. Coverage varies according to the provider and the state. Even within a state, different areas may have different types of eligibility requirements.
For questions, call Medicare at 1-800-MEDICARE or TTY at 1-877-486-2048.
How Do Unitedhealthcare Medicare Advantage Plans Cover Home Health Care
UnitedHealthcare Medicare Advantage plans are required to provide all the same benefits as Medicare Part A and Part B, and most UnitedHealthcare Medicare Advantage plans cover some extra benefits not found in Part A or Part B).
That means all UnitedHealthcare Medicare Advantage plans pay for any home health care services covered by Original Medicare, which can include :
- Part-time skilled nursing care
- Medical supplies for use at home
- Home hospice care
Read more information about how Medicare covers home health care services.
UnitedHealthcare Medicare Advantage plans may also cover some extra benefits that may be of use to someone confined to the home. These can include:
- Home delivery of prescription drugs and certain over-the-counter health products
- Telehealth, which allows you to use video conferencing to conduct appointments with your doctor right from your own home
- A membership to Renew Active, a fitness and wellness program that can be done from home
- A 24-hour nurse hotline that connects you with a registered nurse over the phone at any time of day
- Covered transportation to doctors appointments, pharmacies and other health care-related travel
- HouseCalls, which is the UnitedHealthcare in-home health and wellness visits service
Read Also: Can I Draw Medicare At Age 62
When Is Physical Occupational Or Speech Therapy Covered By Medicare
Physical therapy will be covered by Medicare when it will help the client regain strength or movement after an illness or injury. The same holds true for occupational therapy where the goal is to restore functionality, and for speech therapy to help patients relearn how to communicate.
The services will only be covered if they are expected to result in an improvement within a predictable period of time. Additionally, the frequency, duration, and number of services must be reasonable and provided by a qualified therapist. To be eligible for the services your condition must either:
- Be expected to improve,
- Require a maintenance program from a skilled therapist, or
- Require a skilled therapist for maintenance.
Professional therapists will restore or improve the clients ability to perform routine everyday tasks, speak or even walk following an illness or injury. They may also help prevent a condition from worsening and will only be covered if the services specifically, safely and effectively treat the clients condition.
How Does Home Health Care Work
The first step toward receiving home health care is to obtain a physician’s orders and work with a home health care company to develop a detailed care plan. From there, you will be asked to complete an initial consultation with the patient, during which they assess the patient’s needs and develop a plan for treatment. Family members and other caregivers are encouraged to participate in this planning process to ensure consistent and comprehensive care.
When services begin, home health care staff will implement the plan following all physician orders and keep the physician updated about the patient’s progress. The frequency and type of home health visits will vary depending on the patient’s needs. Some patients require daily care while others require only a short visit once or twice per week.
All services are tailored to the patient’s needs.
Read Also: Are Continuous Glucose Monitors Covered By Medicare
How To Get Approved For In
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
You cant simply decide that you prefer your nursing care and other therapy needs in your home. You must meet the qualifications for in-home care.
You cant simply decide that you prefer your nursing care and other therapy needs in your home. You must meet the qualifications for in-home care, and they include the following
You Must Be Under The Care Of A Doctor:
The primary step in getting approved for in-home care is that you and the nursing plan must be under the care of a Medicare-approved doctor. This doesnt mean that the doctor will be at every visit. A home health nurse specialist will administer your plan, which your will create and regularly review.
Youre Homebound:
This is when youre unable to leave your house for treatment. Homebound patients require assistance from a person or piece of durable medical equipment such as a walker or wheelchair to get around the home or to get to services outside the home. Immobile people are considered homebound as well. A doctor can deem that youre homebound if he or she believes that your illness or condition could get worse if you left the home.
You Doctor Certifies That You Need Home Care:
You Dont Need Round-The-Clock Care:
Your In-Home Care Comes From An Approved Home Health Agency:
How Much Does Medicare Cover For Home Health Care
If your client has original Medicare, they dont pay anything for home health services although they will be liable for a co-pay of 20% of the Medicare-approved amount for durable medical equipment .
Before starting with home health care, you, as the agency, will need to advise your client what costs will be incurred and which are covered by Medicare. Youll also need to inform them of any services that arent covered by Medicare. This should be communicated in-person and in writing and youll also need to provide them with an Advance Beneficiary Notice before any non-Medicare services are provided.
In some states you may submit a pre-claim review request to Medicare. This helps you and the client determine whether Medicare is likely to cover the services.
The specific amount a client will owe for non-Medicare covered services will depend on:
- Any other medical insurance they have
- Their doctors rates
- If their doctor accepts assignment
- The type of treatment facility
- Where they get their tests or services.
In some cases, your clients doctor may recommend a treatment plan that requires more regular treatments than are covered by Medicare, or they may recommend services that arent covered. If this happens, the client will be liable for the costs.
Recommended Reading: Does Medicare Pay For Crowns
