Costs Of Pace For Medicare Beneficiaries
Your costs to join a PACE program depends on your financial situation. But there is no deductible or copayment for any drugs, medical services or any type of care approved by your interdisciplinary team regardless of your situation.
PACE Costs If You Have Medicare But Not Medicaid
- A monthly premium for the long-term care part of PACE benefits.
- A monthly premium for Medicare Part D prescription drug coverage.
If you qualify for Medicaid, it can cover the premium for the long-term care portion. If you dont have Medicare or Medicaid, you can still pay your PACE premiums out of your own pocket.
International Community Health Services
98004, 98005, 98006, 98007, 98008, 98009, 98015, 98033, 98034, 98039, 98040, 98052, 98055, 98056, 98057, 98083, 98101, 98102, 98103, 98104, 98105, 98106, 98107, 98108, 98109, 98112, 98115, 98116, 98117, 98118, 98119, 98121, 98122, 98124, 98125, 98126, 98134, 98144, 98145, 98146, 98154, 98164, 98168, 98178, 98181, 98185, 98191, 98195, 98199.
Medicare Advantage Plans Can Also Cover Pacemaker Costs
Medicare Advantage plans are sold by private insurance companies as an alternative to Medicare Part A and Part B .
All Medicare Part C plans must provide at least the same benefits as Part A and Part B. Most Medicare Advantage plans also include prescription drug coverage .
Additionally, many Medicare Advantage plans provide additional benefits, such as:
Recommended Reading: How Much Does Medicare Cover For Home Health Care
Medigap Plans In Pace
There are gaps in Original Medicares coverage, or things that you must pay because Medicare does not. These are usually deductibles and copays, but there are other leftover costs Medicare leaves behind. This is where a Medigap plan comes into play.
Costs covered by Medigap may include:
- Coinsurance and hospital costs after Part As deductible
- First three pints of blood for a blood transfusion
- Hospice care
- Medicare Part A deductible
- Part B deductible
- Part B excess charges
- Medical costs incurred while traveling outside of US
And some plans put a cap on the amount of out-of-pocket costs associated with Medicare.
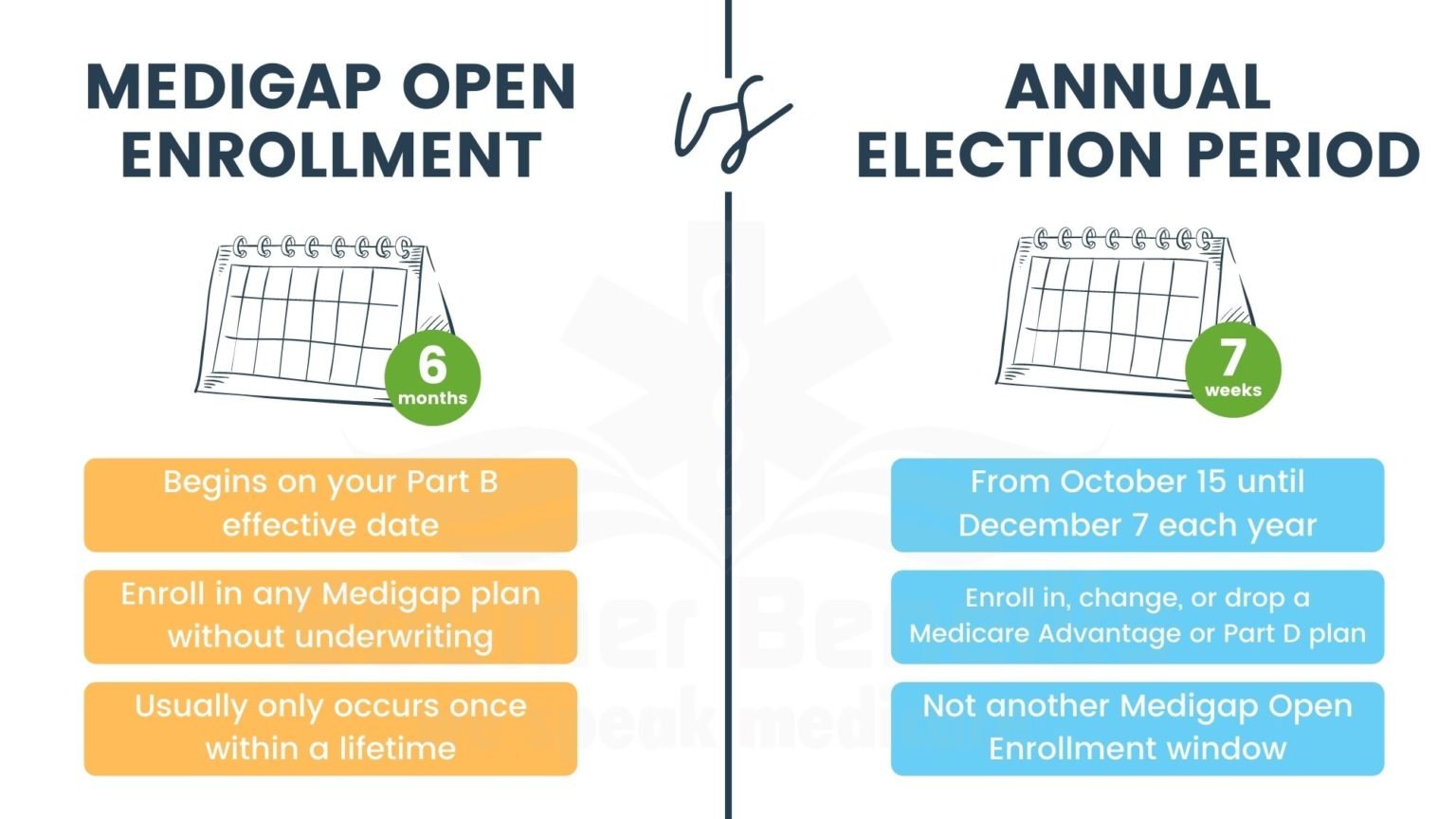
Open enrollment for a Medicare supplement begins the first day you are 65 and enrolled in Medicare Part B and lasts six months after.
This is the best time to get a Medigap plan because you are allowed to enroll without answering any health questions and it is a guaranteed issue.
You are allowed to enroll in a Medicare Supplement at any time once you are enrolled in Part B, but you will be subject to health questions after open enrollment is over.
If you are under the age of 65 but are enrolled in Medicare because you are receiving Social Security benefits, youll get Medicare on your 25th month of disability. Once your Part B benefits become active, that is when your six-month window will begin.
How To Get Help Covering Pacemankers With Medicare
To purchase the best supplement for your needs, call one of our agents at the number above. Were here to assist you with every concern and question you may have. Cant call now? Fill out an online rate form and an agent will contact you to discuss your needs and the best plans in your area.
- Was this article helpful ?
Disclaimer: By clicking the button above, you consent to receive emails, text messages and/or phone calls via automated telephone dialing system or by artificial/pre-recorded message from representatives or licensed insurance agents of Elite Insurance Partners LLC, its affiliates or third-party partners at the email address and telephone number provided, including your wireless number , regarding Medicare Supplement Insurance, Medicare Advantage, Medicare Part D and/or other insurance plans. Your consent is not a condition of purchase and you may revoke your consent at any time. This program is subject to our Privacy Policy and Terms of Use. This website is not connected with the federal government or the federal Medicare program.
Also Check: Does Quest Diagnostics Accept Medicare
Pace Special Medical And Community Care For Chronically Ill
PACE programs are designed to provide a range of integrated preventative, acute care, and long-term care services to manage the often complex medical, functional, and social needs of the frail elderly. Health care services are designed to meet the following objectives:
PACE organizations must provide all Medicare and Medicaid covered items and services as authorized by the interdisciplinary team, as well as additional medically necessary services not covered by Medicare or Medicaid to participants in all settings. PACE organizations must establish and implement a written plan to furnish care that meets the needs of each participant including medical, health and social services that integrate acute and long term care services.
Both Silver Star and Alexian have 60 days to file a request for a hearing if they disagree with the finding of the audit that triggered the $25,000 fines. They dont request an appeal the civil monetary penalties are due October 2, 2013 and may be deducted from Medicares monthly payment to them.
Medicare Coverage For Pacemakers
Home / FAQs / Medicare Coverage / Medicare Coverage for Pacemakers
Medicare coverage for pacemakers is available when medically necessary. Pacemakers are incredibly reliable devices that aid in the treatment of heart arrhythmia.
Arrhythmia or Atrial fibrillation is an irregular heartbeat in which the heart can beat either too slow or too fast. This condition can become dangerous because the bodys organs dont receive a constant supply of blood and can become severely damaged.
A pacemaker is programmed, especially for the patients medical condition and needs. The device is a battery, electrodes, and a generator.
The electrodes attach to the patients heart and works of sensing your heart rate. The electrical pulse the device puts off helps to correct the irregular heartbeats.
Your doctor may recommend a pacemaker if you have any of the following:
- You cannot perform everyday activities
- You suffer from health issues that increase the chances of heartbeat complications
- The use of a pacemaker can correct heart rhythm
To have a pacemaker inserted, a patient must undergo a surgical procedure. The surgery typically lasts a few hours and can be done as an outpatient procedure.
Risks associated with this procedure are usually low, and patients tend to resume regular activity within a week.
Read Also: Where Can I Sign Up For Medicare
What Services Does Pace Cover
PACE covers all health care and medical services that would be covered by Medicare and Medicaid, so long as your health care team determines you need it. If your team determines you need care Medicare and Medicaid does not cover, PACE may cover it anyway.
Examples of PACE Services
- Adult day care, including nursing
- Home health care
- Hospital and nursing home care when needed
- Lab and X-ray services
- Medical care from a PACE doctor familiar with your condition and medical history
- Medically necessary transportation to the PACE center for activities or medical appointments
- Medical specialties including vision, hearing, dental and other care or therapy
- Medical transportation to some medical appoints in your community
- Occupational, physical and recreational therapy
- Prescription drug coverage
- Preventative care
- Social services such as caregiver training, support groups and temporary care in a nursing home, hospice inpatient facility or a hospital
- Social work-related counseling
Program Benefits And Services
PACE/LIFE Programs are designed to provide all of a participating seniors medical and personal care needs.
Program benefits come only in the form of medical and care services. Seniors do not receive cash payments. Benefits are determined on a case-by-case basis, are provided by a dedicated team of healthcare professionals, and can include any of the following.
- Adult Day Care / Adult Day Health
- Audiology
- Durable Medical Equipment
- Emergency Services
- Womens Services
PACE programs do not pay for assisted living in a traditional sense. But persons residing in assisted living communities can still receive care services paid for by PACE. To clarify, a PACE program would treat an individual residing in an assisted living community the same as a person living at home. PACE would arrange daytime transportation to take the individual to and from an adult day care center. This could greatly reduce the amount of care services provided by the assisted living community . However, PACE will not pay for the room and board in assisted living.
Recommended Reading: What Is A 5 Star Medicare Plan
What Are The Qualifications For Pace
Eligibility Requirements for Programs of All-Inclusive Care for the Elderly To qualify for PACE, a person must be age 55 or over, live in a PACE service area, and be certified by the state to need a nursing home level care. The typical PACE participant is similar to the average nursing home resident.
How To Apply For Pace / Life Programs
Persons can apply for the PACE or LIFE Program with the individual, regional PACE providers. . For more information about PACE Policy, please visit the National PACE Association website.
While there are many positives to these programs, an unfortunate reality is the application process can require patience and perseverance. For some programs in certain areas, the application and approval process can take as long as nine months. This is by no means the case everywhere, but applicants and their families should be aware of this possibility.
Don’t Miss: What Is The Yearly Deductible For Medicare
Medicare Coverage For Transtelephonic Pacemaker Monitoring
Medicare covers transtelephonic monitoring devices when the record is at least thirty seconds long and viewable on an ECG strip. Transtelephonic pacemaker devices are small electronic mechanisms that work hand in hand with the pacemaker. Their job is to transfer the patients heart rhythm live over the phone. Technology, like the transtelephonic pacemaker, allows patients to send heart rhythm recordings to doctors by the internet or fax.
What Is The Main Goal Of The Pace Program
Objectives: The Program of All-inclusive Care for the Elderly is a long-term care delivery and financing innovation. A major goal of PACE is prevention of unnecessary use of hospital and nursing home care. Setting: PACE serves enrollees in day centers and clinics, their homes, hospitals and nursing homes.
You May Like: Who Is Eligible For Medicare Extra Help
Eligibility For Pace Programs
Before you can join a PACE program, you must first be enrolled in Medicare, Medicaid or both. In some states, PACE is only available to people on Medicaid. You will need to check with your state Medicare or Medicaid office about the rules in your state.
In addition, you will need to meet other requirements to join PACE.
Eligibility Requirements to Enroll in PACE
- Be age 55 or older.
- Live in the PACE programs service area.
- Be certified by your state as needing nursing home-level care.
- Be able to safely live in your community with help from PACE.
Enrollment in PACE is voluntary, but if you want to join and meet the eligibility requirements, you sign an enrollment agreement. Your enrollment continues as long as you want it to, regardless of changes in your health. If you decide that PACE isnt for you, you can leave it at any time.
What Is The Pace Program
If you are 55 or older, PACE can help you stay in your home instead of moving to a nursing home facility. A team of health-care providers coordinates your care so all your needs are met.
PACE provides both medical care and support services, such as meals and household chores. If you join PACE, you can receive care in your home, in the community, or at a PACE center in your area.
PACE is not an add-on to Medicare, and you dont need to be enrolled in Medicare to join the program. If you qualify for PACE, it will become your only health-care coverage program.
Read Also: Can Medicare Be Used Out Of State
Qam I Eligible To Join Pace
You are eligible to join if you:
- Are 55 years or older
- Live in a designated PACE service area
- Are able to live in the community safely
- Meet the level of care requirements as determined by the California Department of Health Care Services
To qualify for PACE, individuals must meet certain financial requirements. For more details, speak with one of our PACE care experts by calling TTY: .
Pace Interdisciplinary Provider Team
PACE uses an interdisciplinary team of health care providers to deliver medical services to its participants. The team consists of a staff of health care professionals and paraprofessionals that assess your needs, develop care plans tailored for you and then deliver the services you require.
Those services can include acute care services or nursing facility services if you need them.
Basic Members of a PACE Interdisciplinary Team
- Primary care doctor
- Recreational therapist or an activity coordinator
- Social worker
Teams usually meet daily to discuss the status of participants in the PACE program and to ensure each of them is getting their medical and social needs met.
Recommended Reading: Does Part B Medicare Cover Dental
How Do I Get More Information On Pace
For information on the PACE program and enrollment, contact:
- Providence PACE intake at 320-5325, or visit .
- ICHS PACE at 462-7100 or visit www.ichsPACE.org
For policy and contract information please contact PACE Program Manager, Kathryn Pittelkau at 725-2366 or
Additional information can also be found on the National PACE Association website or the CMS website.
Plan Benefits For 2022 Healthpartners Journey Pace
Jump to:
HealthPartners Journey Pace H4882-002 is a 2022 Medicare Advantage Plan or Medicare Part-C plan by HealthPartners available to residents in Minnesota. This plan includes additional Medicare prescription drug coverage. The HealthPartners Journey Pace has a monthly premium of $0 and has an in-network Maximum Out-of-Pocket limit of $5,500 . This means that if you get sick or need a high cost procedure the co-pays are capped once you pay $5,500 out of pocket. This can be a extremely nice safety net.
HealthPartners Journey Pace is a Local PPO. A preferred provider organization is a Medicare plan that has created contracts with a network of “preferred” providers for you to choose from at reduced rates. You do not need to select a primary care physician and you do not need referrals to see other providers in the network. Offering you a little more flexibility overall. You can get medical attention from a provider outside of the network but you will have to pay the difference between the out-of-network bill and the PPOs discounted rate.
Recommended Reading: Can I Sign Up For Medicare Part B Online
Qualifications For Pace/life Programs For Pace Programs
- Age participants must be at least 55 years old.
- Disabilities / Health- participants must require the level of care typically provided in nursing homes. During the screening process, they will be certified as such by a team of doctors, therapists and nurses. A diagnosis of Alzheimers, Parkinsons or dementia does not automatically ensure the applicant will be medically qualified. For these conditions, the progression of disease is important.
- Family the participants marital status has no impact on their eligibility.
- Financial the programs in and of themselves do not have financial eligibility requirements. However, most participating seniors are enrolled in Medicare, Medicaid, or both. Therefore, they must meet the Medicare requirements or the Medicaid requirements. Those who are dually eligible for both Medicare and Medicaid comprise 90% of seniors in PACE. That said, if one is not eligible for Medicare or Medicaid, there is a private pay option.
- Veteran Status Medicare PACE / LIFE programs are available to both Veterans and non-Veterans.
- Geographic currently PACE programs are not available nationwide. Participants must live or be willing to live in a Medicare PACE or LIFE Program eligibility area.
For many low to middle income seniors, Medicare PACE programs are the best long term care option, balancing quality of life with quality care and affordability.
Medicare Coverage For Biventricular Pacemaker

Biventricular pacemakers work both lower chambers of the heart. Medicare covers biventricular pacemakers but requires regular monitoring of the devices. Biventricular devices are monitored every two weeks within the first month, and every four weeks from that point up until the 7th month. From seven months until three years post-surgery, pacemakers will go through monitoring every eight weeks.
Don’t Miss: Does Aetna Medicare Advantage Have Silver Sneakers
Question: What Is The Pace Program For Seniors
The Programs of All-Inclusive Care for the Elderly provides comprehensive medical and social services to certain frail, community-dwelling elderly individuals, most of whom are dually eligible for Medicare and Medicaid benefits.The Programs of All-Inclusive Care for the Elderly provides comprehensive medical and social services to certain frail, community-dwelling elderly individuals, most of whom are dually eligible for Medicare and Medicaid benefitsMedicaid benefitsIn general, Medicaid recipients must be U.S. citizens or qualified non-citizens, and may include low-income adults, their children, and people with certain disabilities. Along with Medicare, Tricare, and ChampVA, Medicaid is one of the four government sponsored medical insurance programs in the United States. https://en.wikipedia.org wiki Medicaid
How Much Does The Pace Program Cost
There is a monthly premium that covers the long-term care portion of the PACE benefit.
If you dont have Medicare or Medicaid, youll be responsible for paying this premium. The premium amount will depend on the services you need and your PACE service area.
If you dont qualify for Medicaid, youll also pay a premium for your Medicare Part D medications. But you wont have to pay any deductibles or copayments for services provided by your PACE care team.
Don’t Miss: Can I See A Doctor In Another State With Medicare
