Does Medicare Cover Weight Loss Revision Surgery
Yes. Previous weight loss surgery may fail, and you may need a revision. Requesting a weight loss revision surgery may initiate many questions at first. Make sure to be open and transparent with your doctor to ensure you both agree with your condition.
After your doctor recommends surgery, Medicare pays for weight loss revision surgery when its medically necessary.
When Congress designed Original Medicare back in the sixties, health insurance coverage in America was different than it is now. Our legislators broke Medicare into two parts: hospital and outpatient coverage. Medicares guidelines for covering almost any procedure center around whether the procedure is medically necessary.
Today in America, weight loss surgery is often considered medically necessary to combat obesity. Bariatric surgery helps to reduce the overall size of your stomach so that you feel full earlier and eat less food. Medicare offers coverage for several weight loss procedures.
Medicare will cover some or all of the following procedures: gastric bypass, lap band surgery, sleeve gastrectomy, and duodenal switch. It will not, however, cover any procedure which it considers experimental.
Does Medicare Cover Bariatric Weight Loss Surgery
The demand for Medicare coverage of bariatric weight loss surgery is steadily growing as the obesity rate of Americans is on the rise. After meeting various requirements and gaining approval from a licensed physician, Medicare coverage includes different bariatric weight loss surgeries to treat obesity and related health conditions.
Although Medicare pays for bariatric procedures, the program decides denial or approval of benefits on a case-by-case basis. To be considered for approval, the bariatric surgery must first be approved by the FDA. However, even after a Medicare beneficiary meets the requirements for bariatric surgery, Medicare coverage is still at the discretion of their doctor and Medicare.
Not all situations in life are the same. Unfortunately, this means coverage may vary from person to person. However, bariatric surgery is often deemed medically necessary because many conditions stem from morbid obesity.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
Biliopancreatic Diversion And Duodenal Switch Procedures
While appropriate surgical procedures for severe obesity primarily produce weight loss by restricting intake, intestinal bypass procedures produce weight loss by inducing a malabsorptive effect. Biliopancreatic bypass or diversion consists of a subtotal gastrectomy and diversion of the biliopancreatic juices into the distal ileum by a long Roux-en-Y procedure the result is a 200-cm long alimentary tract, a 300- to 400-cm biliary tract, and after these 2 tracts are joined at the distal anastomosis, there is a 50-cm common absorptive alimentary tract. The BPD was designed to address some of the drawbacks of the original intestinal bypass procedures, which resulted in unacceptable metabolic complications of diarrhea, hyperoxaluria, nephrolithiasis, cholelithiasis and liver failure.
A decision memorandum from the Centers for Medicare and Medicaid Services concluded that open or laparoscopic BPD with or without DS are reasonable and necessary for Medicare beneficiaries.
Also Check: Does Medicare Cover Urgent Care Centers
Read Also: What Is A Ppo Medicare Plan
Lets Take A Closer Look At The Different Types Of Bariatric Surgery
Some of the common types of Medicare bariatric surgeries include gastric bypass, lap band surgery and gastric sleeve surgery.
Gastric bypass surgery
This common malabsorptive weight loss surgery is also known as Roux-en-Y gastric bypass . In this procedure, a small stomach pouch is created to restrict food intake. The rest of the stomach is bypassed via a Y-shaped segment of the small intestine, which reduces the amount of calories and nutrients the body absorbs.
LAP-BAND® surgery
This surgery is defined as Laparoscopic adjustable gastric banding . This common weight loss procedure involves the placement of a hollow band around the upper end of the stomach, creating a small pouch and a narrow passage into the larger remainder of the stomach. The band is inflated with saline solution, which can be increased or decreased over time to alter the size of the passage.
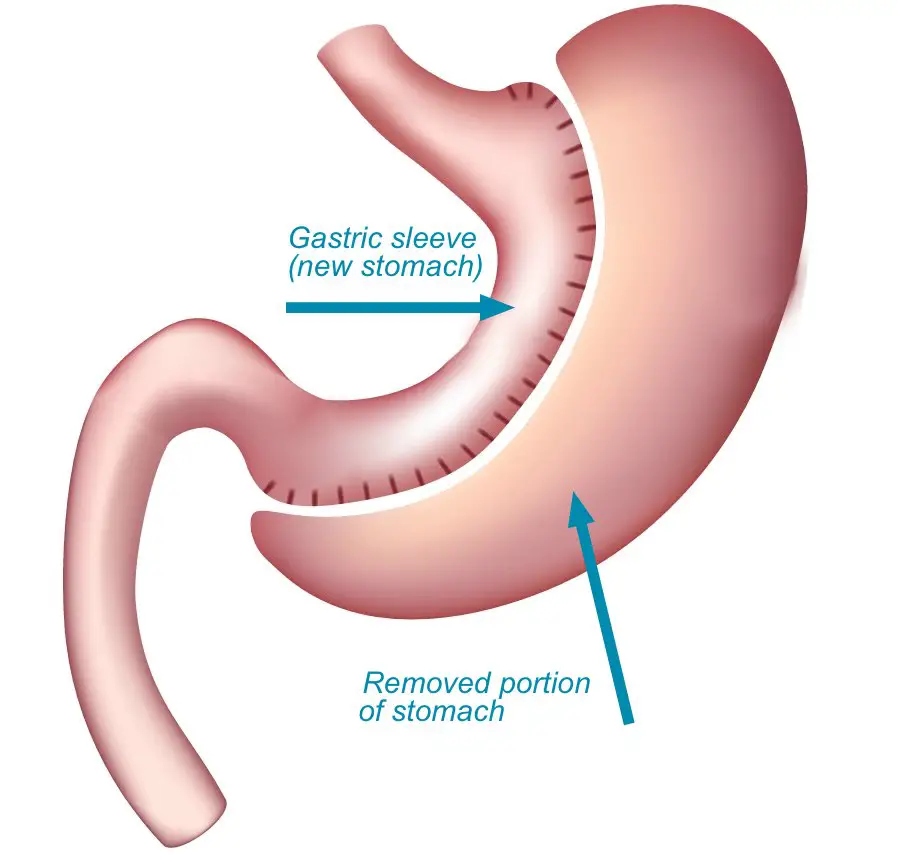
Gastric sleeve surgery
This weight loss surgery is also commonly known as vertical sleeve gastrectomy or sleeve gastrectomy . This procedure involves the removal of the greater curvature of the stomach and approximately 80% of the stomach volume. While pyloric sphincter and stomach functions are preserved, the remaining stomach resembles a slender curved tube.
Is Bariatric Surgery Covered By Insurance
Most commercial insurance plans approve all four typical weight loss surgical procedures gastric bypass, vertical sleeve gastrectomy, gastric banding with LAP-BAND® or REALIZE® bands, or duodenal switch procedures for the appropriate patients.
To receive approval, a patient usually needs to have a BMI above 40, or a BMI between 35 and 39 if the patient also has certain medical conditions such as diabetes, sleep apnea, or high blood pressure. Some insurance companies have a mandatory three-month weight management protocol that you must complete before surgery. Some have a protocol as long as six months.
For all plans, dietary and psychological evaluations are mandatory. This is a practical step that helps ensure your readiness for the procedure.
Your medical team can work with you to help you meet the particular requirements of your health plan in order to qualify for insurance coverage.
Also Check: How To Opt Back Into Medicare
Average Cost Of Bariatric Weight Loss Surgery With Medicare
In the United States, the average cost of bariatric weight loss surgery can be as much as $25,000-$30,000. With Medicare Part A and Part B, those who meet the eligibility requirements and are accepted for coverage will be responsible for the Medicare Part A and Part B deductibles, Medicare Part B 20% coinsurance, and any coinsurance or deductible payments for Medicare Part D.
Medicare Part A helps cover the inpatient hospital expenses. However, if your surgery is an outpatient procedure, Medicare Part B helps pay 80% of doctor services and supplies. Then, Medicare Part D will cover any prescription medications that your doctor prescribes after surgery.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
A Medicare Supplement plan would cover most, if not all, of your out-of-pocket expenses after Original Medicare pays. On the other hand, if you receive coverage from a Medicare Advantage plan, you may need to go through more extensive pre-requisites. This is because your coverage will differ from Original Medicare.
- Was this article helpful ?
Medicare Coverage For Bariatric Weight Loss Surgeries
Home / FAQs / Medicare Coverage / Medicare Coverage for Bariatric Weight Loss Surgeries
According to the Centers for Disease Control and Prevention , nearly 40% of US adults are obese. Obesity increases the chance of major health risks and may significantly decrease a persons quality of life. Thus, shortening the lifespan. When fighting obesity, weight loss surgery such as bariatric surgery is one of the most efficient approaches.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
If you are a Medicare beneficiary hoping to receive bariatric surgery, you could receive coverage through your Medicare plan. Medicare coverage for bariatric weight loss surgery is available for beneficiaries who meet specific criteria. While not all bariatric weight loss surgeries receive coverage, several options are available for those with Medicare.
You May Like: Does Medicare Cover Nursing Home For Dementia Patients
Estimating The Cost Of Getting Bariatric Surgery
Its hard to know exactly how much your weight loss surgery may cost because its difficult to determine what services you may need during and after your procedure. If you are at an inpatient hospital, then Medicare Part A will help cover costs. If your weight loss surgery is performed at an outpatient center, then Medicare Part B will assist with these costs.
Since Original Medicare doesnt cover the entire cost of the surgery, you can also consider buying a Medicare Supplement plan to help offset any out-of-pocket expenses you may incur, such as some of the deductibles, copayments or coinsurance.
Medicare Advantage plans must cover the same benefits as Original Medicare, but many offer additional benefits such as prescription drug coverage and an annual out-of-pocket maximum.
Prophylactic Mesh Placement For Prevention Of Incisional Hernia After Open Bariatric Surgery
In a systematic review and meta-analysis, Dasari and colleagues examined if mesh prevents post-operative incisional hernia in open and laparoscopic bariatric surgery patients. A total of 7 studies met inclusion criteria. These investigators abstracted data regarding post-operative IH development, surgical site infection, and seroma or wound leakage and performed a meta-analysis. The prophylactic mesh group had significantly decreased odds of developing IH than the standard closure group . No included studies evaluated outcomes after prophylactic mesh during laparoscopic bariatric surgery. The authors concluded that prophylactic mesh during open bariatric surgery appeared to be beneficial in reducing post-operative IH without significant increasing the odds of surgical site infection or seroma or wound leakage. Moreover, they stated that higher quality studies, including those in laparoscopic patients, and cost-utility analysis, are needed to support routine use of this intervention.
Read Also: What Age Does Medicare Take Effect
Are Weight Loss Plans Covered Under Medicare
Original Medicare does cover weight loss programs, therapy, screenings and surgery if your doctor or health care provider decides that treatment is medically necessary.
Medicare Advantage plans also cover weight loss programs when theyre medically necessary.
Some Medicare Advantage plans also offer free memberships to wellness programs like SilverSneakers, gym memberships and nutritional home meal delivery.
Also Check: Does Medicare Plan F Cover International Travel
Mini Sleeve Gastrectomy By Natural Orifice Trans
Erridge and colleagues summarized the clinical applications of natural orifice transluminal endoscopic surgery in bariatric surgery. These investigators carried out a review of data, until December 2014 regarding techniques and outcomes of bariatric NOTES procedures. A total of 9 publications were included in the final analysis, with another 6 papers describing endolumenal procedures included for comparison. All NOTES studies adopted a hybrid procedure. Hybrid NOTES sleeve gastrectomy was described in 4 humans and 2 porcine studies. In humans, 6 subjects were converted to conventional laparoscopic methods, and 1 post-operative complication was reported. Mean excess weight loss was 46.6 % . The authors concluded that transvaginal-assisted sleeve gastrectomy appeared feasible and safe when performed by appropriately trained professionals. However, they stated that improvements must be made to overcome current technical limitations.
Also Check: Do Doctors Have To Accept Medicare Advantage Plans
You May Like: How Old Do You Have To Be To Draw Medicare
What Is The Safest Form Of Weight Loss Surgery What Types Of Surgery Are There
Answer: Weight loss surgery, also known as bariatric surgery, is a tool to produce significant weight loss for morbidly obese people. If you have unsuccessfully battled a serious weight problem, Baylor Frisco can help you take control of your health and change your life. We have devoted the necessary resources to provide you with comprehensive care, including patient education, pre-surgical counseling, advanced surgical options, and long-term post-surgical care. Baylor Frisco offers several different kinds of weight loss surgery designed to help patients manage their weight including:
Do I Qualify For Bariatric Surgery With Medicare
If you are enrolled in Medicare, the first step is to see your doctor. You will need a doctors approval and diagnosis, both to see if bariatric surgery is right for you, and to have a record for when you start discussing your options with Medicare and your bariatric surgeon.
There is no pre-approval process for Medicare bariatric surgery. Each patient is reviewed on a case by case basis. If you are interested in undergoing this type of surgery through Medicare, start with the following process:
- Find a Medicare-approved bariatric surgeon.
- Ensure that you qualify for Medicare to pay for bariatric surgery.
- Complete any and all special meetings and consultations the surgeon requires.
- Complete all of your testings, including lab work, x-rays, and more.
- Have the surgeon contact Medicare with all of the results of your medical tests.
The approval process can be lengthy. For those that are in need of immediate treatment, it may be best to see if there are other options out there. But once you have completed this process, if you meet all of their requirements, you should be able to receive bariatric surgery medical treatment.
Danielle Kunkle Roberts is the co-founder at Boomer Benefits, an agency that helps baby boomers navigate their entry into Medicare.
This site complies with the HONcode standard for trustworthy health information.
Packages comparable to A Lighter Me®
Dont Miss: What Is The Average Premium For Medicare Advantage Plans
Recommended Reading: Does Cigna Have A Medicare Advantage Plan
Gastric Balloon Cost Insurance & Discounts
The average gastric balloon cost is $8,150. It is usually not covered by insurance, although your doctor may be able to get some of the costs covered.
The price can often be reduced through tax deductions and special doctor-specific discounts.
This page covers everything you need to know about paying for the gastric balloon procedure.
Why Does Medicare Not Pay For Vertical Sleeve Gastrectomy
Morbidly Obese individuals are usually addicted to Food, have extensive health issues and are disabled . Medicare will pay for mal-apsorption procedures making the morbidly obese patient looking for longevity and better quality of life, addicted to expensive Vitamins and Protein for life,or risk severe health issues. The VSG Procedure seems to limit the amount of food you can eat at each sitting without the mal-absorption problems. Why wont medicare cover this procedure?
Also Check: What Should You Do If You Lost Your Medicare Card
Sleeve Gastrectomy Selection Soared Nearly 2000% Following Medicare Coverage Change
Disclosures: We were unable to process your request. Please try again later. If you continue to have this issue please contact .
The 2012 Medicare change to cover sleeve gastrectomy, in addition to Roux-en-Y gastric bypass, for bariatric surgery boosted its selection exponentially, with significant regional and temporal variation between states.
In data published in JAMA Network Open, researchers also noted that the selection of sleeve gastrectomy over gastric bypass depended on how widely used that procedure was used in that state during the prior year.
This study sought to understand whether geographic variation in the use of sleeve gastrectomy following implementation of insurance coverage could be used as an instrumental variable in analysis of observational data,Ryan Howard, MD, a general surgery resident at Michigan Medicine, and colleagues wrote.
In a National Medicare claims database, the researchers identified 76,077 patients who had bariatric surgery from 2012 to 2017 44,367 by sleeve gastrectomy and 31,710 by laparoscopic Roux-en-Y gastric bypass .
Looking at a sample of the 10 largest states, the researchers found that New Jersey had the largest increase in sleeve gastrectomy and Ohio had the smallest increase .
Utilization of sleeve gastrectomy increased during the study period from 515 procedures
Medicare Part A Costs
Your out-of-pocket costs under Medicare Part A may include monthly premiums, deductibles, and coinsurance. Most people get premium-free Part A, because they or their spouse paid Medicare taxes for the required 10 years to qualify. Around 1 percent, though, pay the Medicare Part A premium, which is $499 per month in 2022.
The Medicare Part A deductible is $1,566 per benefit period, which begins when youre admitted as an inpatient and ends once you go 60 consecutive days without receiving inpatient care.
Finally, coinsurance under Part A is $0 per day for the first 60 days. After that, youll pay $389 per day for days 61 through 90 and $778 per day for days 91 through your 60 lifetime reserve days.
Also Check: Is Shingrix Vaccine Covered By Medicare
Recommended Reading: Are Spouses Eligible For Medicare
What Are The Costs And Funding Options For Gastric Sleeve Surgery
- There are a number of factors which may influence the final cost of surgery including hospital fees and the price of medications.
- For patients with private insurance out of pocket, cost is $6,000 .
- For patients without private insurance the cost ranges from $17,500-18,000 which can be paid through your superannuation as well.
Criteria For Coverage Of Surgery Costs
In order for Medicaid to cover the cost of your surgery and the associated surgeon visits, you must meet the requirements below.
- Over the age of 13 for a female and 15 for a male.
- Body Mass Index must be over 35 with at least one comorbidity.
- Co-morbidities include sleep apnea, high blood pressure, high cholesterol, diabetes.
You Might Not Qualify for Weight Loss Surgery Coverage if:
- Long-term steroid use
- Inflammatory bowel disease, chronic pancreatitis, pregnancy, or non-compliance with medical treatment.
- Psychological treatment that might interfere with post-operative compliance with diet and lifestyle.
Recommended Reading: What Does Medicare Part B Include
Read Also: Does Quest Labs Accept Medicare
Will A Medicare Advantage Plan Cover Weight Loss Surgery
Coverage for any procedure with a Medicare Advantage plan can change depending on a range of circumstances. UnitedHealthcare has an Advantage plan that covers weight loss surgery after meeting the plans guidelines.
Advantage plans determine the level of benefits and costs of service based on the service area, health condition, and medical necessity.
Medicare Advantage beneficiaries should contact their policy directly if unsure about coverage and benefits.
